Only a few clinical exploratory manoeuvres are truly discriminatory and useful in shoulder disease. The aim of this study is to correlate the physical examination results of the shoulder with the true diagnosis found by arthroscopy.
MethodsA retrospective case series of 150 patients with the most common surgical conditions of the shoulder. Data were collected on the suspicion of each pathology, the physical examination of the patient, and the actual discovery of the disease during arthroscopic surgery.
ResultsThe Bankart examination manoeuvres of the lesion show the best results, with a 92.1% positive prediction value (PPV), a 99.1% negative predictive value (NPV), followed by the impingement syndrome, with a PPV of 94.4%, and total cuff rupture with a PPV of 92.3%.
Exploration of the superior labrum anterior to posterior (SLAP) lesion had an NPV of 99.1%.
ConclusionPhysical examination is sufficient to diagnose or rule out Bankart. A positive physical examination provides the complete rupture of the rotator cuff, and requires further studies. The patients suspected of subacromial syndrome only need an NMR if the physical tests are negative.
The conclusions drawn from this work can have a significant impact on both cost savings (by reducing forward tests), and saving time in certain cases in which, after appropriate physical examination, surgery may be indicated without losing time in intermediate steps.
En la patología del hombro pocas son las maniobras exploradoras verdaderamente discriminatorias y útiles en la clínica. El objetivo de nuestro trabajo es correlacionar la exploración física del hombro con el diagnóstico real hallado por artroscopia.
MétodosEstudio retrospectivo tipo serie de casos de 150 pacientes con las principales patologías quirúrgicas de hombro. Se recogieron datos de la sospecha de cada patología según la exploración física del paciente y el hallazgo real de las mismas durante la cirugía artroscópica.
ResultadosLas maniobras de exploración de la lesión de Bankart es la que ha obtenido mejores resultados con un valor predictivo positivo (VPP) del 92,1% y un valor predictivo negativo (VPN) del 99,1%, seguida por el síndrome subacromial con un VPP del 94,4%, la rotura total del manguito con un VPP del 92,3%.
La exploración en la lesión SLAP tiene un VPN de 99,1%.
ConclusiónLa exploración física es suficiente para diagnosticar o descartar una lesión de Bankart. Una exploración física positiva es diagnóstica de rotura total del manguito de los rotadores y no requiere estudios complementarios. Los pacientes con sospecha de síndrome subacromial solo necesitarán una RM confirmatoria si los test físicos son negativos.
Las conclusiones extraídas del presente trabajo pueden tener una importante repercusión tanto en ahorro de costes (por reducción de pruebas complementarias), como por ahorro de tiempo en determinados casos en los que, tras la exploración física adecuada, se puede indicar cirugía sin necesidad de pasos intermedios.
Shoulder pain is one of the most common reasons for consultation in everyday clinical practice. One of the most frequent shoulder lesions is the subacromial syndrome, the total and partial tear of the rotator cuff, acromial-clavicular arthropathy (AC), lesions that affect joint stability such as Bankart lesions, SLAP or Hill–Sachs, and tendinosis of the long head of the biceps (LHB).1 Shoulder pain is estimated to have an incidence of 16–26%.2 Its annual incidence is 15 new episodes for every 1000 patients seen in Primary Care, and in this context it is the third most common reason for consultation.3 The incidence of tendon and joint lesions increases with age, as the soft tissues weaken and gradually degenerate; therefore, in the Netherlands, the incidence of subacromial syndrome stands at 19 for each 1000individuals/year. It is higher in women older than 45 years old and lower in younger people.4 LHB tendinosis is far more common in the adult population, and its overall incidence stands at from 29% to 66%.5
One cause of the increase in shoulder injuries is the rise in sports activities, and injury of the superior labrum from anterior to posterior, or SLAP lesion, is one of the injuries most frequently resulting from the practice of sport. SLAP is a pathology that affects the labrum, a fibre-cartilage pad that increases the stability of the joint and contains the humeral head; the upper part of the labrum detaches from the glenoid fossa, largely due to repeated luxations. Its importance lies in the fact that it is a pathology directly associated with sport, and its incidence has increased exponentially over recent years, with a prevalence of about 3.9–11.8%.6
Respecting the rotator cuff, some bibliographical material states that physical exploratory tests achieve good sensitivity and specificity, with an overall precision of approximately 61–75%,7,8 although no test alone has good discriminatory value.9
A meta-analysis by Hegedus et al. showed that very few exploratory shoulder manoeuvres seem to be discriminatory and therefore useful for a definitive diagnosis.10
Of all the pathologies which were evaluated, those of the labrum aroused the most enthusiasm among the researchers. Given these results, they concluded that it is particularly necessary to undertaken high quality studies that would test the diagnostic performance of these exploratory manoeuvres.
At the current time it is hard to achieve an exact diagnosis based solely on the clinical history of the patient and physical examination. This leads to increased use of other techniques to establish a diagnosis. These include MRI, ultrasound scans or diagnostic arthroscopy. These tests are laborious, expensive and/or invasive, so that they should be used as little as possible.
This study aims to compare the results of physical exploration of the shoulder with the intraoperative findings corresponding to 150 patients treated consecutively in our department by surgical arthroscopy of the shoulder.
Based on the results of this comparison, physical exploration of the shoulder will be evaluated in terms of whether or not it is sufficient to reach a decision for treatment, without the need for other diagnostic tests.
Material and methodsA retrospective longitudinal study was designed of the case series type and level of evidence iv.
From 2 October 2012 to 27 September 2014 a total of 246 patients were operated using the shoulder arthroscopy procedure, exclusively by the Upper Limb Unit of our hospital. The participants were selected consecutively. 150 of these patients fulfilled all of the necessary criteria for inclusion in the study.
These inclusion criteria were:
- –
Being older than 18 years old, with no upper age limit.
- –
Presenting one or more of the pathologies under study: subacromial syndrome, partial or total tear of the rotator cuff, AC arthropathy, Hill–Sachs, Bankart, SLAP or LHB tendinosis.
- –
With a report on physical examination of the shoulder prior to the operation, in their clinical history.
- –
With MRI or an arthro-MRI as a complementary imaging test prior to the said operation.
- –
Having been subjected to a shoulder arthroscopy as a therapeutic procedure.
Patients with incomplete data in their clinical history were excluded, as were those with defective imaging tests or ones carried out in another institution, as well as a history of previous surgery.
A total of 96 patients were excluded from the 246 who were analysed. The group of excluded patients included 17 who had none of the pathologies under study, while 67 only had an ultrasound scan or computerised tomography image as a complementary imaging test, 6 had no documented physical examination and 6 had been operated using open surgery.
The Diraya platform was used to access data after signing a confidentiality document. The variables recorded for each patient were the pathologies described above as found by physical examination and arthroscopic findings, of which the latter were the standard technique (gold standard).11 Other variables were also included, such as age, sex and the length of time passed between the physical examination and the operation.
The clinical history of each patient included the data from the physical examination of all their case reports, as well as the intraoperative findings of the arthroscopic surgery.
Physical examination is especially relevant in shoulder pathologies, given that several manoeuvres are specifically aimed at examining individual structures. These may save the patient from having to undergo unpleasant and costly diagnostic tests. There are many clinical tests for the diagnosis of different shoulder pathologies.
In our study we centred on a positive outcome for 2 tests in each type of pathology. These have the purpose of using clinical criteria to diagnose the existence of each pathology, except for the Hill–Sach lesion, which is diagnosed using a single test.
The examination manoeuvres used in this study are described below, divided according to the different pathologies.
The manoeuvres used in the examination of the subacromial space are:
- –
Neer's impingement: this consists of the passive raising of the arm in abduction, flexion and internal rotation, while the examiner blocks the mobility of the scapula. This can be performed when the patient is standing up or lying down, and pain occurs when there is anterosuperior conflict in the subacromial space.
- –
Yocum: the patient places their hand on the side being examined on the contralateral shoulder and actively raises their elbow against the resistance of the hand of the examiner, without raising their shoulder. Pain occurs when there is anterointernal conflict.
The manoeuvres for examining the supraspinatous tendon are:
- –
Jobe: the examiner stands in front of the patient and places their arms at 90° abduction, with 30° of anterior flexion and in internal rotation with their thumb pointing downward. The examiner then pushes the arm down while the patient tries to keep the initial position.
- –
The sign of the fallen arm: the patient sits and places their extended forearm in 120° abduction, keeping the arm in this posture while moving it slowly downward. The examiner exerts pressure against the abduction and evaluates the resistance applied by the patient.
The manoeuvres for examining the LHB tendon are:
- –
Speed's manoeuvre: the examiner stands in front of the patient and opposed the forward pressure of the arm, consisting of anterior flexion with the shoulder in external rotation, the elbow in complete extension and the palm of the hand facing upwards. Pain and a lack of resistance indicate tendinopathy.
- –
Yergason's manoeuvre: this consists of forearm supination against resistance while keeping the shoulder blocked and the elbow on the trunk with an 80° flexion. Pain indicates the problem.
Examination manoeuvre for anterior glenoid-humeral instability associated with the Hill–Sach lesion:
- –
Liu's apprehension test: the patient has to be sitting or standing. The examiner stands behind him and holds their arm, raising it to 120° abduction and 90° external rotation. With his other hand he holds their shoulder with his thumb behind it and his fingers in front of it. This achieves accentuated external rotation and rearward pressure, so that if it causes pain and/or apprehension, with a clear sign of catching or stress, this indicates chronic anterior instability associated with the Hill–Sach lesion (Fig. 1).
Examination manoeuvre for anterior glenoid-humeral instability associated with Bankart's lesion:
- –
Anterior cavity manoeuvre: the patient sits with their forearm resting on their thigh with the arm relaxed. The examiner, from behind them, holds the humeral head between their thumb and other fingers, moving it forwards and backwards. When this manoeuvre is easy to achieve there is a suspicion of Bankart's lesion.
- –
Jobe's re-centring or repositioning test: a first part similar to the apprehension test is performed, followed by a second manoeuvre in which the palm of the hand is placed on the humeral head and is pushed down to recentre it, at which if the pain and apprehension disappear then Bankart's fibrous lesion is suspected, while if the apprehension remains, this is a clinical sign of a Bankart bone lesion.
The SLAP manoeuvres are:
- –
O‘Brien's test: the patient with their shoulder at 90° flexion, 10° adduction and maximum internal rotation, with their elbow extended. Resisted raising is requested that evokes pain in the bicep region. If this is calmed by maximum external rotation, the test is + for a SLAP lesion (Fig. 2).
- –
Meyers’ test: the patient is in supine decubitus with their shoulder at 90° abduction and their elbow flexed. Resisted supination + RE is requested. Pain in the bicep region due to the mechanism of “detaching” of the labrum.
Lastly, the examination manoeuvres for the AC joint are:
- –
The crossed arm test: with the patient in supine decubitus they are requested to place their hand on the rear face of the contralateral shoulder. Of pain arises at the level of the AC joint then the test is positive.
- –
Painful arch test: this examines the painful arch of shoulder movement in abduction. If the movement of actively separating the arm causes pain at from 140° to 180° at the level of the AC joint, the test is conclusive for AC arthrosis.
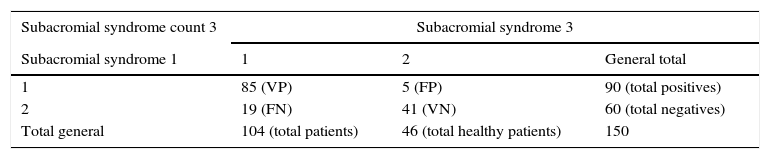
The data obtained were entered into an Excel (Microsoft Office for Windows Vista) database, recording the following dichotomous variables: pathologies (1: yes; 2: no) and sex (1: male; 2: female), with the following as discrete or discontinuous quantitative variables: age and the time from physical examination to arthroscopy. Statistical analysis was then performed using version 3.0 of the R program. Statistically significant values were considered to be those where P<.05 (<0.5%). Descriptive statistics were used to analyse numerical variables and absolute values, while percentages were used for quantitative variables. Kendall's (W) coefficient was used for comparison and concordance testing. P was calculated using the chi-squared test. Multivariable analysis was performed using the Random Forest algorithm. The Excel database was used to obtain a dynamic table for each one of the lesions, showing the number of true positives, false negatives (FN), false positives (FP), true negatives and the total (Table 1).
Example of the comparative analysis dynamic of each pathology. Subacromial syndrome 3 column corresponds to arthroscopy, and subacromial syndrome 1 corresponds to physical examination.
| Subacromial syndrome count 3 | Subacromial syndrome 3 | ||
|---|---|---|---|
| Subacromial syndrome 1 | 1 | 2 | General total |
| 1 | 85 (VP) | 5 (FP) | 90 (total positives) |
| 2 | 19 (FN) | 41 (VN) | 60 (total negatives) |
| Total general | 104 (total patients) | 46 (total healthy patients) | 150 |
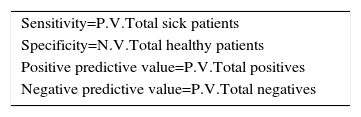
These tables were used to calculate the sensitivity and specificity values, the rate of FN, the rate of FP, the predictive positive value (PPV) and negative predictive value (NPV) for each one of the lesions studied (Table 2).
Results and discussionThis study has a sample size (n) of 150 patients; 76 women and 74 men, with an average age of 52.28 years old (from 19 to 80 years old).
The average time from the first visit by patients to General Orthopedics until they were operated was 462 days (65–776 days).
Kendall's coefficient is a non-parametric technique which measures the degree of association between several sets (k) of entities. It is useful for the determination of the degree of agreement between several observers or the association between 3 or more variables. For samples where n>30 a parametric test is usually used, in spite of the fact that the distribution is not normal. Nevertheless, there is an increasing tendency to use parametric tests only for samples which fulfil all normal distribution requisites. This is why Kendall's coefficient was used for our study.
Kendall's concordance coefficient (W) varies from 0 to 1. 1 indicates complete concordance, while 0 shows complete disagreement. Concordance is the capacity of a test to obtain the same result when the measurement is repeated using different measurement conditions. It is desirable for the result to be as close as possible to 1. A high coefficient means that the observers are using the same standard when evaluating the tests. It is not sufficient to know that W is closer to 0 or to 1, but rather we also have to know whether W is statistically significant to reject the null hypothesis or that of casual concordance.
Unlike the hypotheses, the level of significance (P) is independent of the magnitude of the differences found. A very small P does not imply a higher degree of concordance. In our study the magnitude of concordance is supplied by Kendall's concordance coefficient (W). Landius and Koch12 set levels of concordance depending on the value obtained:
- –
Poor: <0.4.
- –
Moderate: 0.4–0.6.
- –
Good: 0.6–0.8.
- –
Very good: >0.8.
A value of P<.05 is considered to show that the results were statistically significant. All of the results obtained a P value within the desirable range except for the Hill–Sachs lesion.
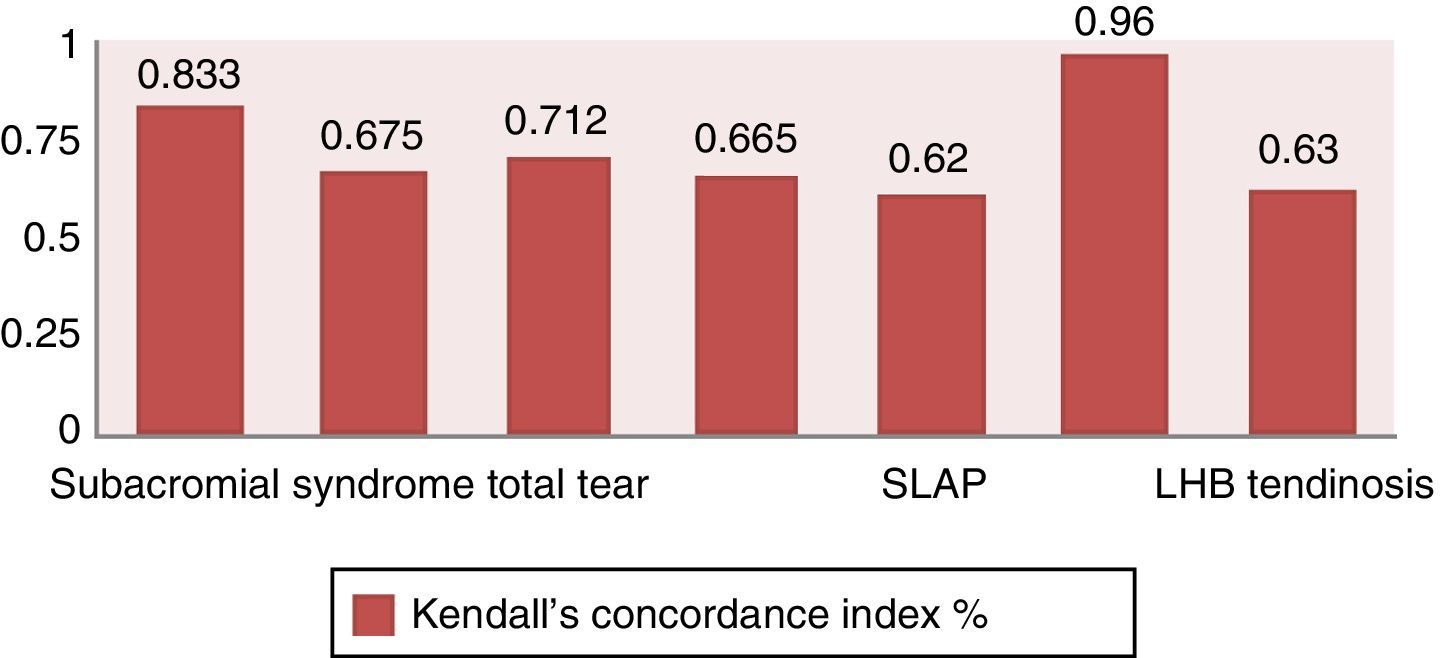
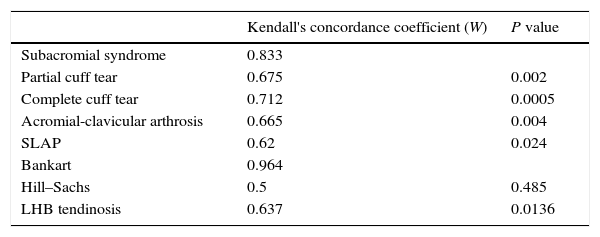
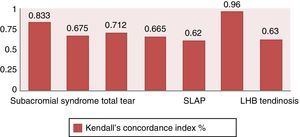
Table 3 shows the values of W for each one of the pathologies: the correlation is very good for Bankart and the subacromial syndrome, and it is good for the others except for Hill–Sachs, where the results are not statistically significant.
Kendall's concordance coefficient (W) between the results of physical examination and arthroscopic intraoperative findings, for the different pathologies studied, as well as the degree of statistical significance.
| Kendall's concordance coefficient (W) | P value | |
|---|---|---|
| Subacromial syndrome | 0.833 | |
| Partial cuff tear | 0.675 | 0.002 |
| Complete cuff tear | 0.712 | 0.0005 |
| Acromial-clavicular arthrosis | 0.665 | 0.004 |
| SLAP | 0.62 | 0.024 |
| Bankart | 0.964 | |
| Hill–Sachs | 0.5 | 0.485 |
| LHB tendinosis | 0.637 | 0.0136 |
Bankart's lesion, where W=0.964, is the one closest to absolute concordance between physical examination and arthroscopy, followed by the subacromial syndrome, where W=0.833, and the total or partial tear of the rotator cuff, for which W=0.712 and W=0.675, respectively (Fig. 3).
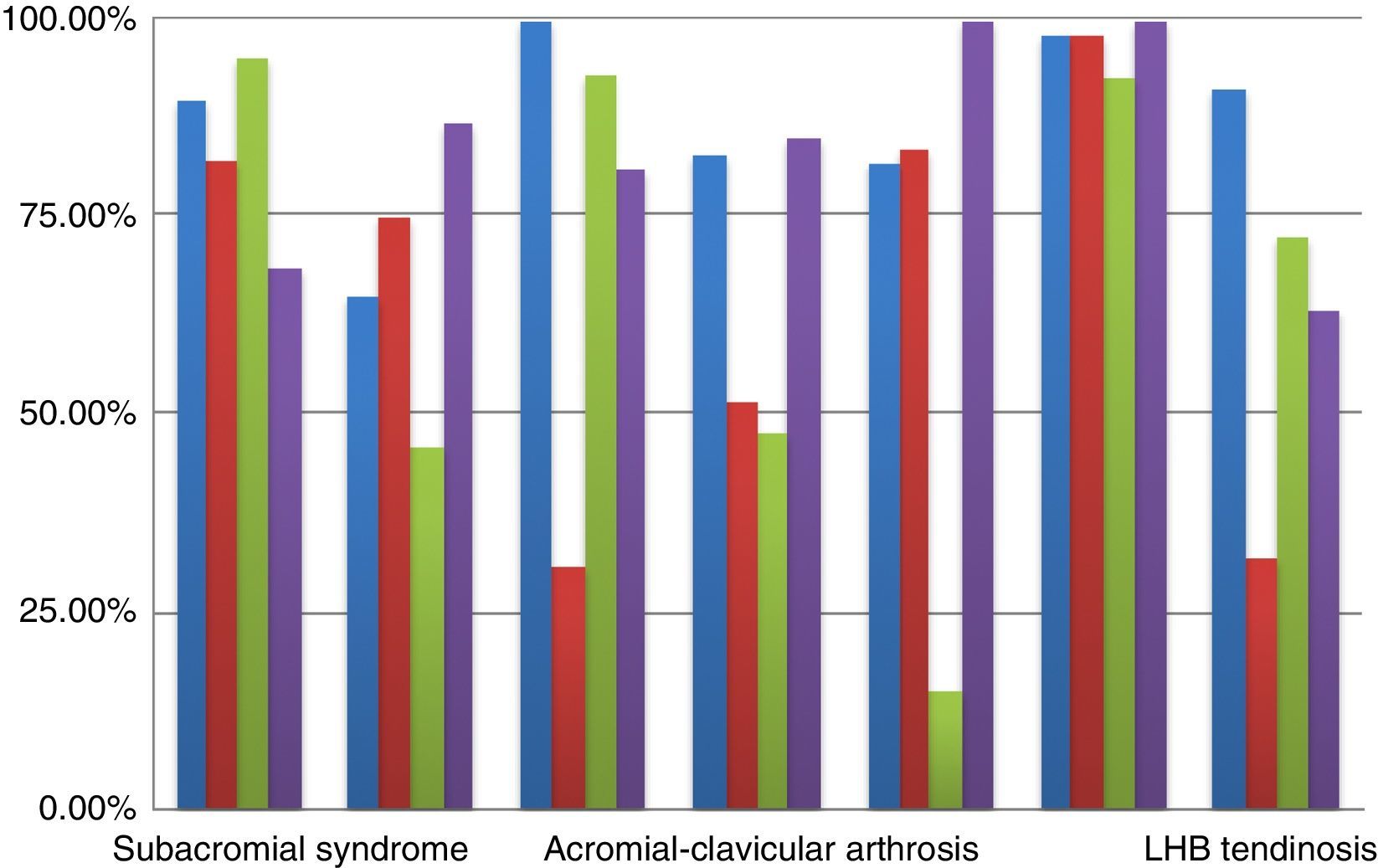
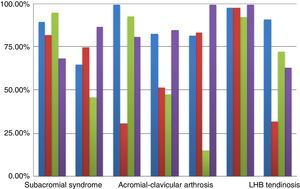
Sensitivity, specificity, positive predictive value and NPV were recorded for each one of the pathologies included in the study (Fig. 4).
Sensitivity is the capacity of the test to detect sick subjects or, expressed in another way, it is the probability that a sick subject (according to the gold standard) scores “+” in the test.
Sensitivity therefore expresses how “sensitive” the test is in detecting the presence of the disease. A high level of sensitivity indicates a low number of falsely healthy patients (Table 1).
Tests with a very high level of sensitivity are therefore very useful in ruling out the presence of disease.
Specificity is the capacity of a test to detect healthy subjects. It is the probability that a subject who is healthy (according to the gold standard) scores “−” in the test. Specificity is the probability that a healthy individual will have a negative result. A high level of specificity indicates a low frequency of FP.
PPV is the probability that a subject who is “+” according to the test is truly infirm. NPV is the probability that a subject who is “−” according to the test is actually healthy. Sensitivity and specificity are internal validity parameters. Internal validity is the capacity of the test to give exact results in sample subjects that do not depend on the prevalence of the disease. The PPV and NPV are external validity parameters: the capacity of the test to generalise the results obtained in the sample of the population, and whether they depend on the prevalence of the disease. Internal validity is a requisite for external validity.
Type I error is also known as alpha-type error (α) or FP. This error arises when the researcher does not accept the null hypothesis when this is true in the population. I.e., the patient is considered to be infirm in spite of being healthy. Type II error, which is also known as beta-type (β) error (β being the probability of this error existing) or FN, arises when the researcher does not reject the null hypothesis when this is false in the population. This is equivalent to the probability of a FN result, or in this case a false healthy patient. Type I and type II errors did not arise in this study.
According to Voigt et al.,13 one of every 10 knee or shoulder MRI gives rise to error. Based on this fact, the statistical values of physical examination with a significance >90% will be relevant for the definitive diagnosis and will not require additional imaging tests.
Subacromial syndromePhysical tests for subacromial syndrome show a high level of specificity, sensitivity and PPV. In a 2012 study Cadoghan et al.14 obtained a maximum sensitivity of 70% (Hawkins-Kennedy). In this case sensitivity is higher (81.7%) which indicates a greater capacity to detect infirm patients; even so, it is still less than specificity. The PPV at 94.4% implies that these tests have a very high capacity to predict whether positive subjects in the test really are infirm. I.e., a positive result in the test would be highly indicative of a true positive (infirm). Nevertheless, the NPV is low, so that a patient with a negative result could be a true negative (healthy) or a FN (infirm). In other words, the positive results that we obtain in physical examination will correspond to more than 94% of truly infirm patients. In this case no imaging test (MRI) will be necessary to confirm the presence of the disease.
Although the sensitivity of tests has improved, some patients will be falsely diagnosed as healthy. In this case we should perform a MRI. On the other hand, Diercks et al.2 considered that a single physical sign was insufficient to diagnose subacromial syndrome. A combination of several tests is necessary to increase the diagnostic value of physical examination. A restriction of our study is that the individual value of each diagnostic test is not known. We are unable to know the weighting of each test within the diagnosis. It would be necessary to design a new study which included the positivity or negativity of each test and compare this with the result of arthroscopy (the gold standard).
Breakage of the rotator cuffThe results obtained for the total or partial tear of the rotator cuff are similar to those in the literature: 68.4% sensitivity and 100% specificity.6 However, in the latter case it is not specified whether these values correspond to the partial or total tear of the cuff. Centring on our own results, in cases of partial tear the best values correspond to sensitivity and the NPV, although they do not attain the predetermined value (90%). In the physical examination negative results will lead us to think that we have a true healthy case. Nevertheless, this does not attain our predetermined value of 90%. In the case of a positive result we should bear in mind that it may be a FP and, if we operate, the patient will be subjected to an unnecessary risk. In patients with a suspicion of partial tear of the rotator cuff it would be prudent to perform an imaging test regardless of the findings in the physical examination. Only if the result is negative will a case be individually evaluated by a surgeon to decide whether or not to perform MRI.
In cases of total tear specificity is close to 100%, as is the PPV at 92.3%. Physical examination will therefore be conclusive for diagnosis of the lesion. When there are positive signs of complete cuff tear, the decision may be taken to operate the patient, with the almost total probability that this will not be an α error, i.e., considering a healthy patient to be sick. In the case of a positive physical examination there is no need to perform MRI. If the result is negative then one will be necessary.
Acromial-clavicular arthropathyThe exploratory clinical manoeuvres for acromial-clavicular arthropathy are painful, and this is also the case for sub-scapular tendinopathy.15 In general the manoeuvres which requires internal rotation and adduction may cause FP, and direct injections in the AC joint are a means of increasing diagnostic precision (by pressing the joint space and inserting the needle from front to rear and 45° from top to bottom) with local anaesthesia of the mepivacaine type.16
The exclusive use of AC arthroscopy is hardly able to detect patients, as is shown by the sensitivity values. There is also a very low probability that a patient with a positive result is infirm. As sensitivity increases the NPV also rises, while when specificity increases the PPV increases. However, this is not the case for this lesion: specificity is high and the PPV is low; sensitivity is low and the NPV is high. The reason is that the PPV and NPV are influenced by the high prevalence of the disease.17 Although physical examination is necessary in AC arthropathy, it must be supported by another diagnostic tool such as MRI or the selective infiltration of the AC joint with local anaesthesia.
The SLAP (superior labrum anterior to posterior) lesionThe literature states that physical examination is unable to be used alone to identify SLAP lesions, given that no test comes close to being diagnostic.18–20 The NPV is 99.1% while the PPV is 15%. Therefore, if the result of examination is negative there is no indication to request a MRI. However, this should be done if the result is positive as in the majority of cases it will be a FP.
Bankart's lesionBankart's lesion is the one that gave the best results. Sensitivity, specificity, the PPV and the NPV are very close to 100%. A positive result in physical examination is almost totally sure to represent a true patient. In the same way, a negative result is almost totally sure to be a true healthy patient. In the light of the results of this study, physical examination is sufficient to reach an exact diagnosis of Bankart's lesion and to decide on a therapeutic attitude.
Hill–SachsAlpha or type I error is the one that arises when differences are due to chance. In this case it would consist of stating that the results of physical examination agree with the real findings of surgery, when no such correlation actually exists. For clinical significance to exist there has to be statistical significance. Therefore, and based on the results of our study, Liu's exploratory apprehension catching manoeuvre as used in our study does not positively indicate the real existence of Hill–Sachs lesion without a complementary imaging test. Subsequent studies should continue researching new ways of reaching a diagnosis of this lesion by means of physical examination.
Tendinosis of the long head of the bicepsClinical diagnosis of this lesion is complicated. The test Palm-Up is one of most widely used here, with a precision of 54%.4 Although traditional tests usually have a high level of sensitivity they have very low specificity and a poor PPV. The opposite occur in our study: the specificity value found is higher than that for sensitivity, and the PPV is good, although not sufficiently to make it possible to rule out MRI as a complementary test.
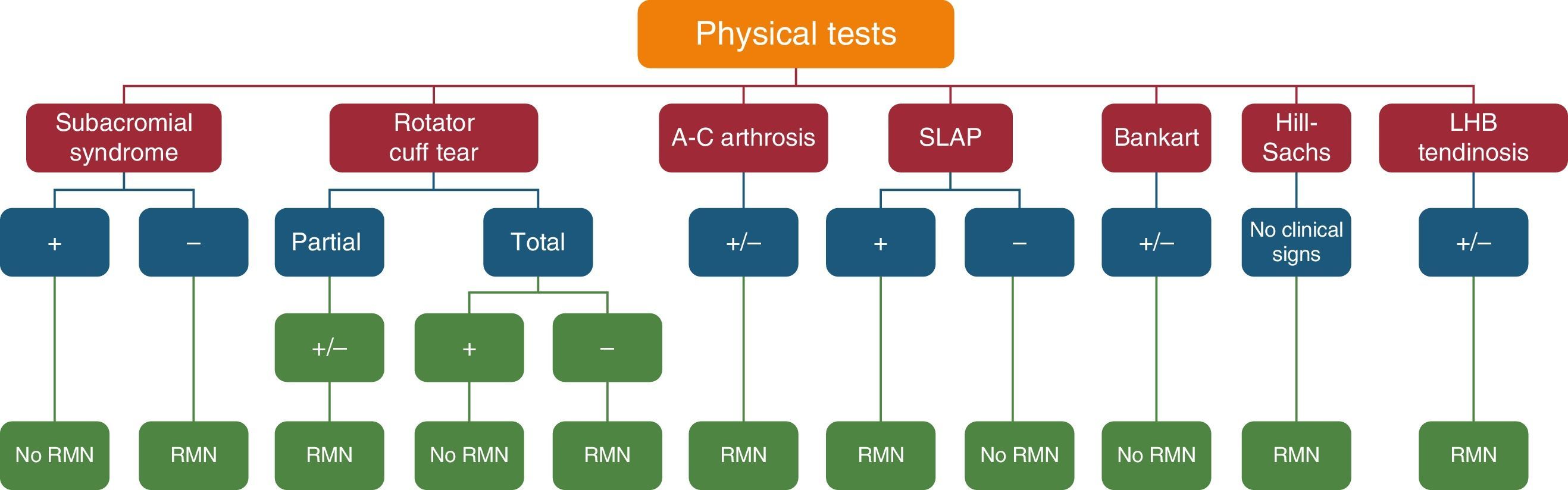
ConclusionsGiven the results of this study it may be concluded that:
- 1.
There is very good concordance between physical examination and surgery in the subacromial syndrome and Bankart's lesion.
- 2.
Physical examination is sufficient to diagnose or rule out Bankart's lesion.
- 3.
Patients with the suspicion of subacromial syndrome will only need MRI to confirm whether physical tests are negative.
- 4.
Positive physical examination diagnoses the total tear of the rotator cuff and does not require MRI.
- 5.
A negative physical examination rules out the SLAP lesion.
- 6.
Age, sex and the time lapse between physical examination and surgery do not influence the precision of the test.
Some publications offer algorithms for the most specific exploratory tests for different shoulder pathologies, although they do not analyse them.21 Nor do they evaluate their precision statistically and compare it with actual arthroscopic findings.
Based on statistical analysis of the results of this study, the algorithm described here summarises the situations in which it is recommended to perform complementary tests and those in which this is not so in connection with the pathologies and positivity or negativity of physical examination (Fig. 5).
The conclusions extracted from this work may have an important affect in terms of reducing costs (due to a fall in the number of complementary tests),as well as by saving time in certain cases when, following suitable physical examination, surgery can be indicated without the need for intermediate steps.
Level of evidenceStudy of a series of cases: level IV.
Ethical responsibilitiesProtection of persons and animalsThe authors declare that for this research no experiments took place with human beings or animals.
Data confidentialityThe authors declare that they followed the protocols of their centre of work for the publication of patient data.
Right to privacy and informed consentThe authors have obtained the informed consent of the patients and/or subjects referred to in the paper. This document is held by the corresponding author.
Conflict of interestsThe authors have no conflict of interests to declare.
We would like to thank Dr. García-Vázquez and Dr. Parra-Serrano for their unconditional support and help throughout this study, as well as the statisticians Pedro Álvarez-García and Elene García-Nieto, for their technical help and much more, together with all of the members of the Upper Limb Unit of the Virgen del Rocío Hospital.
Please cite this article as: García Parra P, Anaya Rojas M, Jiménez Bravo B, González Oria MO, Lisbona Muñoz M, Gil Álvarez JJ, et al. Correlación entre la exploración física y los hallazgos intraoperatorios de patología de hombro tratada mediante artroscopia. Análisis estadístico de 150 pacientes. Rev Esp Cir Ortop Traumatol. 2016;60:306–314.