Chronic recurrent multifocal osteomyelitis (CRMO) is an autoinflammatory disease that presents with aseptic bone inflammation and can be accompanied by multisystemic symptoms. We present the case of a 14-year-old male with a 2-week history of pain located at the tibial metaphysis and fever. X-ray revealed a lytic lesion in the tibial metaphysis. MRI revealed an intramedullary bone lesion with perilesional bone oedema. CT-guided biopsy discounted malignancy and microbiological cultures were negative. The patient's symptoms and fever worsened after the biopsy; therefore antibiotherapy was commenced for a suspected superinfection. A body MRI was performed given the persistence of the fever, which found a second active lesion in the spine that was diagnosed as CRMO and progressed well with anti-inflammatories. CRMO is an entity that is difficult to diagnose. Differential diagnosis is extensive with infectious diseases, tumours and other autoinflammatory diseases. Prompt diagnosis and appropriate treatment are crucial to prevent sequelae.
La osteomielitis crónica multifocal recurrente (OMCR) es una enfermedad autoinflamatoria que cursa con inflamación ósea aséptica y puede acompañarse de clínica multisistémica. Presentamos el caso de un varón de 14 años con dolor a nivel de la metáfisis tibial de 2 semanas de evolución y fiebre. En la radiografía se objetivó lesión lítica en metáfisis tibial. Se realizó RM que mostró lesión ósea intramedular con oedema óseo perilesional. Se realizó biopsia guiada por TAC descartando malignidad y siendo los cultivos microbiológicos negativos. Posterior a la punción presentó empeoramiento clínico y fiebre por lo que iniciaron antibioterapia ante sospecha de sobreinfección. Ante la persistencia de fiebre se realizó RM-body que halló segunda lesión activa a nivel vertebral, diagnosticándose de OMCR y evolucionando bien con antinflamatorios. La OMCR es una entidad de difícil diagnóstico. El diagnóstico diferencial es extenso con enfermedades infecciosas, tumores y otras enfermedades autoinflamatorias. Es crucial su diagnóstico precoz y tratamiento adecuado para prevenir sus secuelas derivadas.
Chronic recurrent multifocal osteomyelitis (CRMO) is a rare, mainly paediatric autoinflammatory disease that presents with aseptic bone inflammation and on occasions is accompanied by multisystemic symptoms.
Initial symptoms are diverse. Patients may present with single or multifocal bone pain commonly located in the axial skeleton, with local signs of inflammation, fever or other symptoms (ocular, gastrointestinal, respiratory or cutaneous).1 In addition to its clinical diversity there are no specific diagnostic tests for this disease and diagnosis is of exclusion.
Clinical caseWe present the case of a male 14-year-old patient who presented with a 2-week history of pain at tibial metaphyseal level, initially related to physical activity and which had progressively increased to being a constant pain when he presented for consultation. Haemogram values were normal and there was no elevation of acute phase reactants.
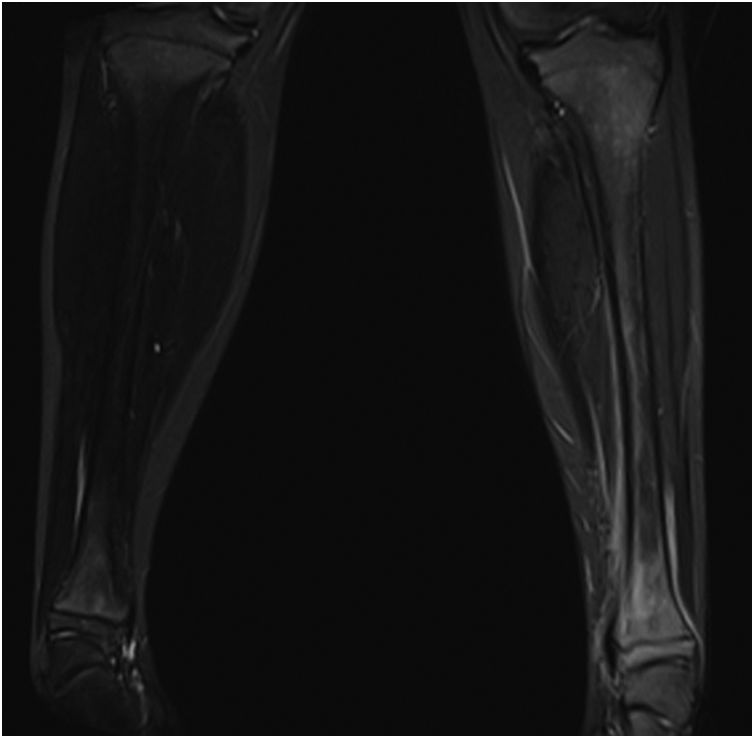
Radiography showed a lytic lesion with well defined edges in the tibial metaphysis with questionable cortical enhancement (Fig. 1.) Magnetic resonance imaging (MRI) was performed which showed intramedullary bone lesion with perilesional bone oedema, signs of periostitis and soft tissue oedema. Due to the aggressive clinical picture a CT-guided bone biopsy was performed which revealed signs of acute and chronic inflammation with no atypical cellularity and microbiological cultures tested negative.
On bone puncture the patient's symptoms considerably worsened with local inflammation (erythema and local heat), an increase in pain, fever and high elevation of acute phase reactants (PCR 240mg/l). After the biopsy, on suspicion of a superinfection of the lytic lesion, haemoculture and further puncture for culture was carried out and the patient was admitted to hospital with intravenous antibiotic treatment with cefazoline. No clinical or analytical improvement ensured. During hospitalisation the patient maintained a good general status, with persistent fever despite the antibiotic for the first 6 days and pain in the medial tibial malleolus. An ultrasound scan was therefore performed to rule out complications, and this resulted normal. Once local complications had been ruled out and with further negative microbiological cultures the antibiotic was suspended.
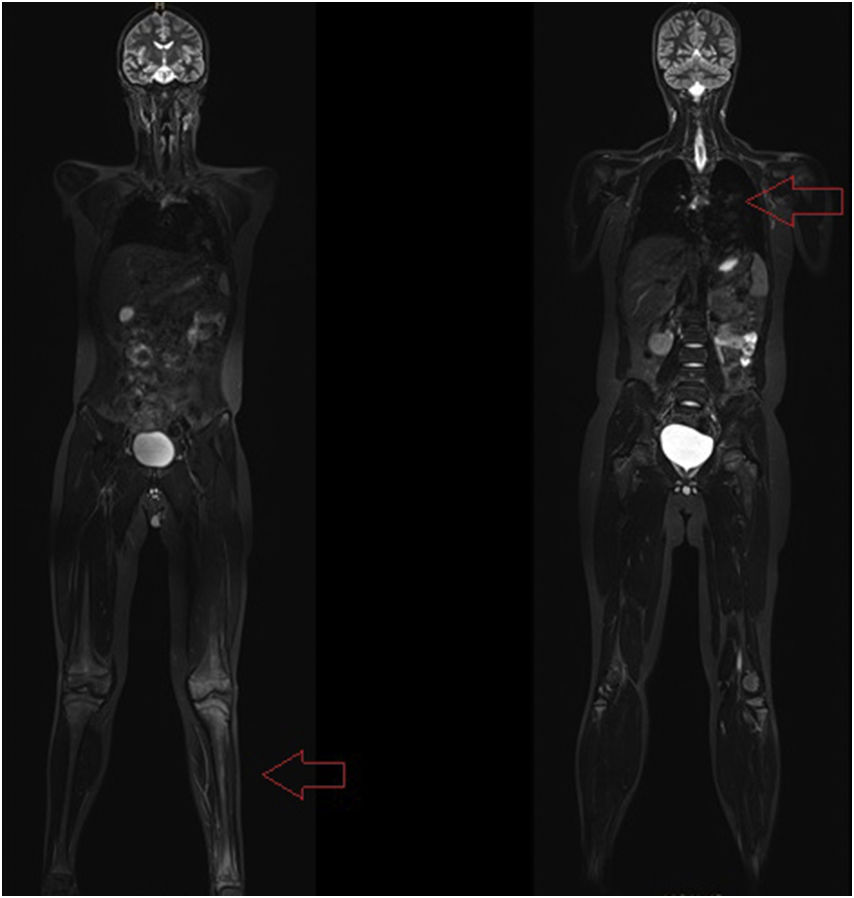
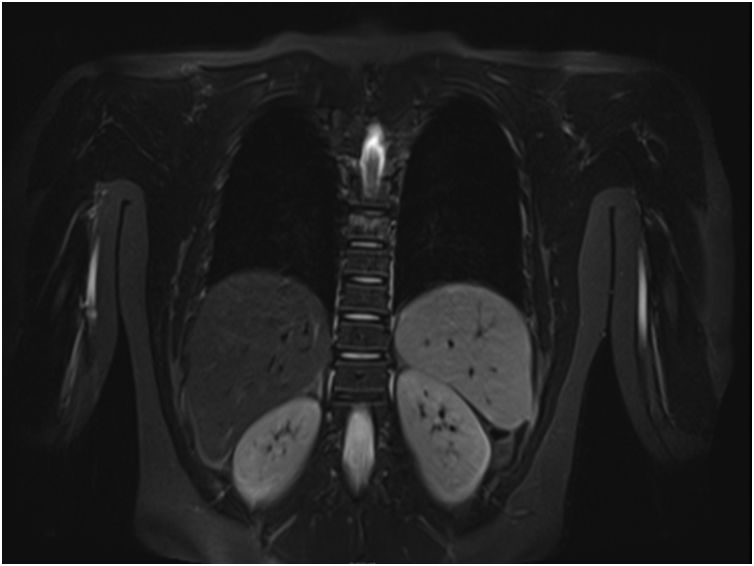
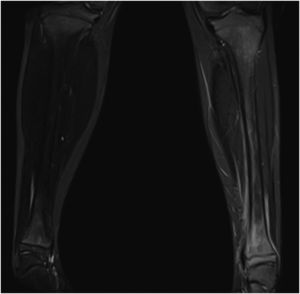
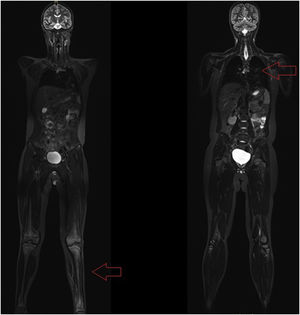
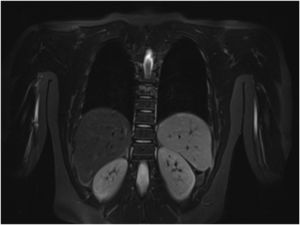
A whole-body MRI was performed which showed persistence of inflammation in the distal metaphysis of the tibia which affected and went beyond the physis, with signs of periostitis and oedema of adjacent soft tissues (Fig. 2). It shows an extensive pattern of oedema of the bone marrow in the left inferior extremity which suggested Sudeck transient-algodystrophy osteoporosis. A second focus of osteomyelitis was also observed at vertebral D8 level with subchondral oedema, and crushing compatible with subacute fracture, as a silent lesion (Figs. 3 and 4).
Due to the lesion characteristics, multifocality and absence of malignancy in the biopsy and also to the repeatedly negative results from the cultures, differential diagnosis was made between recurrent, chronic, multifocal osteomyelitis and Langerhans cell histiocytosis. Immunohistochemcial study was made of the pathologic anatomical specimens with staining for CD1a, S100 and CD68 which was not suggestive of Langerhans cell histiocytosis but was compatible with osteomyelitis with marked reactive changes.
Treatment with nonsteroidal anti-inflammatory drugs (NSAIDS) was initiated and due to the major bone destruction, monthly treatment with pamidronate was added, with good pain control and progressive improvement of lesions in MRI.
DiscussionCRMO is an entity which is difficult to diagnose due to its non-specific symptoms and its wide spectrum of presentation. Its aetiopathogenesis is little known, although an imbalance has been described between pro-inflammatory cytokins (IL-6, TNFα) and anti-inflammatories (IL-10, IL-1β) which produce an increase in bone resorption by activation of osteoclasts.2 The hypothesis of a genetic base has also become more important in recent years in the presence of the described syndromic forms (Majeed syndrome, cherubism, hypophosphatasia and primary hypertrophic osteoarthropathy) and the increased prevalence described among members of the same family.3 A relationship has also been observed with spondyloarthropathies and psoriasis, with increased incidence in these patients.4 This is a disease which mainly affects the paediatric population, with a low prevalence, although this has probably been underestimated (1:160,000 to 1:2,000,000),5 and there are therefore currently no specific treatment guidelines.
Clinical diversity is great, onset is insidious in the form of bone pain with symptoms of local inflammation, typically at night. It mainly affects the long bone metaphyses, and on occasion may characteristically affect other bones such as the sternum, clavicle and jaw. Systemic symptoms such as fever, retarded growth, myalgias and arthritis are commonly present (in up to 30% of patients arthritis is combined with exudation from the adjacent joint and/or lesion of the joint cartilage). In addition to bone lesions other symptoms have been described involving organs and systems in 25% of cases (skin, intestine and kidneys).
No specific diagnostic test exists, and diagnosis is of exclusion. In laboratory tests a slight elevation of acute phase reactants (PCR, VSG) may be observed. Regarding imaging studies, in conventional radiography non specific lesions of osteolysis or sclerosis may be observed but sometimes there are no changes. As a result and because the lesions may be multiple with very few symptoms, scintigraphy and whole-body MRI are the diagnostic tools of choice, with the latter being chosen to avoid radiation and because it is the most sensitive. MRI also enables the differentiation of acute bone oedema or chronic bone oedema and can locate the bone biopsy site to increase performance. Differential diagnosis of this entity principally includes lesions secondary to trauma, infectious diseases or tumours and normally a bone biopsy is performed to rule out other entities. In the biopsy signs of perilesional bone oedema, periostitis and soft tissue oedema are frequently observed.
The disease presents in outbreaks. First line treatment is with NSAIDS. The most commonly used drugs are ibuprofen and naproxen at anti-inflammatory doses. Recently a good response to treatment with indometacin has been described, with its mechanism of action being the inhibition of ossification and the inflammatory response acting at prostaglandin synthesis level, with a clinical and radiological improvement of lesions, achieving complete normalisation of the bone in some cases.6 It is important to maintain treatment with NSAIDS for a minimum of one month prior to considering a patient is not responding, since its mechanism of action begins after 4 weeks of treatment.
Between 20% and 25% of cases do not respond to NSAIDS, and second line treatment is with corticosteroids and methotrexate. When involvement is great or there is resistance biphosphonates, pamidronate and anti-TNF drugs may be effective.7
To conclude, CRMO is a rare disease, diagnosis is from exclusion and is therefore frequently a challenge for the professional (in several series diagnosis is delayed 8–13 months).8,9 Early diagnosis and accurate follow-up with whole-body imaging studies is therefore important, together with appropriate treatment for preventing sequelae such as vertebral crushing or fractures, particularly in the axial skeleton or when lesions are lytic.
In our case differential diagnosis was initially that of a tumour disease and from worsening of symptoms after puncture, that of secondary infection.
The MRI was hugely helpful in detecting multifocality. Although the treatment of choice is NSAIDS, we decided to combine them with pamidronate due to the lytic lesions present, with good evolution and progressive improvement of symptoms.
Level of evidenceLevel of evidence IV.
Ethical liabilitiesProtection of people and animalsThe authors declare that no experiments were carried out on humans or animals for this investigation.
Data confidentialityThe authors declare they have adhered to the protocols of their centre of work on the publication of patient data.
Privacy rights and informed consentThe authors declare that no patient data appear in this article.
Please cite this article as: Roig-Abraham N, Méndez-Hernández M, Martínez-Morillo M. Osteomielitis crónica multifocal recurrente en pediatría: un reto diagnóstico. Rev Esp Cir Ortop Traumatol. 2019;63:447–450.