There is no consensus on the treatment of chronic low back pain of disk origin in the medical literature. The few prospective, randomized, controlled studies evaluating the effectiveness of caudal epidural steroid injections (CESI) have obtained contradictory results. The aim of this study is to evaluate the efficacy of CEI in reducing pain and improving the associated disability.
Material and methodThis is a prospective, randomized, case-control study of a group of 46 patients with chronic low back disk pain. Patients were randomly allocated into 2 groups to either receive fluoroscopy guided CESI (CESI-group), or oral non-steroidal anti-inflammatory drugs (NSAID-group). All patients were clinically evaluated at 4, 12, and 24 weeks, and according to the indications of the Spanish Society for Study of Diseases of the Spine (GEER).
ResultsLumbar pain, measured by the visual analog scale (VAS) and the Oswestry Low Back Pain Disability Questionnaire (ODQ), did not improve significantly during follow-up in any of the two study groups (p>0.05). Younger patients, women, patients with shorter duration of symptoms, low physical job demand, without leg pain, and sport-active, included in CESI-group showed a trend toward better results, but none reached statistical significance (p>0.05).
ConclusionsThe present study has not demonstrated the superiority of CESI over NSAIDs in treating chronic low back pain of disk origin. While CESI could show some improvement in patients with degenerative lumbar disk disease, we consider it should be used with caution, informing patients about realistic expectations on the success of treatment.
La literatura no ofrece consenso para el tratamiento del dolor lumbar crónico de origen discal. La infiltración esteroidea epidural por vía caudal (IEEC) ofrece resultados contradictorios en los pocos estudios prospectivos y aleatorizados realizados acerca de su efectividad. El objetivo de nuestro estudio es evaluar la eficacia del tratamiento mediante IEEC para reducir el dolor y mejorar la discapacidad asociada.
Material y métodoEstudio comparativo, prospectivo y aleatorizado de 46 pacientes con dolor lumbar crónico de origen discal. Pacientes asignados de forma aleatoria para recibir IEEC guiada por fluoroscopia (grupo IEEC), o antiinflamatorios no esteroideos por vía oral (grupo AINE). Pacientes valorados según indicaciones de la Sociedad Española para el Estudio de las Enfermedades del Raquis (GEER). Evaluación a las 4, 12 y 24 semanas.
ResultadosDurante el seguimiento, el dolor lumbar medido mediante la escala analógica visual (EAV), y el cuestionario Oswestry de discapacidad (ODI) no experimentaron mejoría significativa en ninguno de los 2 grupos del estudio (p>0,05). El grupo IEEC presentó una tendencia hacia mejores resultados en pacientes de menor edad, en mujeres, en pacientes con menor tiempo de evolución, actividades laborales sedentarias, sin clínica sobre miembros inferiores y que practicaban deporte, pero sin significación estadística (p>0,05).
ConclusionesEl presente estudio no ha demostrado superioridad de la IEEC frente a los AINE, en el tratamiento del dolor lumbar crónico de origen discal. A pesar de que la IEEC pueda presentar alguna mejoría en los pacientes con afección discal lumbar degenerativa, consideramos que debiera ser empleado con cautela, informando al paciente de las expectativas reales del tratamiento.
Herniation of the lumbar intervertebral disk is one of the most common causes of lumbar (or low back) pain. However, many patients with lumbar pain and sciatica do not present herniation of the lumbar disk on magnetic resonance imaging (MRI) or computed tomography (CT) scans. This paradox is probably attributed to the fact that compression of the nerve root is not sufficient to cause pain by itself, and that both the lumbar pain and sciatica may result from local chemical irritation caused by damaged disk tissue.1–3 Up to 90% of patients experience recovery following a first episode of lumbosciatic pain. However, those who suffer second or third episodes also experience frequent recurrences or report living with a varying degree of chronic lumbar pain, and between 10% and 15% of patients eventually undergo surgical treatment.4
In this context, the literature does not provide a uniform criterion to establish treatment guidelines. Moreover, the principle that the outcome after surgery should be better than that obtained through the natural evolution of the disease, and the risk of suffering the dreaded “failed back surgery syndrome” leaves most of these patients without any justified options for surgical treatment.5 The value of caudal epidural steroid infiltration (CESI) for the treatment of lumbar pain and sciatica has been controversial since its introduction.6–8 The actual effect and mechanism of action of CESI on patients with chronic lumbar pain are largely unknown.1,9 In addition, the literature offers a cautious support for the use of CESI for the treatment of patients suffering chronic lumbar pain due to an evident lack of well-designed, relevant and randomized studies.10
The aim of our study was to evaluate and compare the efficacy of treatment by fluoroscopy-guided CESI compared to treatment with non-steroidal anti-inflammatory drugs (NSAIDs) to relieve pain and its related disability in patients with chronic lumbar pain with a discogenic origin.
Patients and methodologyStudy designThis was a randomized, comparative and prospective study which obtained the consent and approval of the Clinical Research Committee. The study population consisted of patients who were recruited among those attending the Orthopedic Surgery and Traumatology outpatient clinic due to lumbar pain between January 2009 and October 2010. All patients were informed about the study and consented to participate in it.
Study subjects- 1.
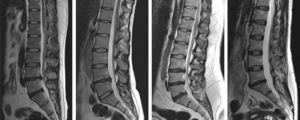
Inclusion criteria were: patients of both genders, aged over 18 years and attending due to lumbar pain and/or pain referred to the lower limbs with characteristics of discogenic pain (non-radicular pain produced in the absence of vertebral deformity, instability and neurological deficit)11 of over 3 months duration, and who freely accepted to participate in the study. All patients underwent an MRI of the lumbar spine to confirm the presence of degenerative disk disease.
- 2.
Exclusion criteria were: manifestation of pain symptoms other than degenerative discal pain, the existence of a history of previous lumbar surgery and the presence of neurological deficit, rheumatic disease or some other prior specific diagnosis for the cause of pain (e.g. lumbar facet syndrome, spondylolysis or spondylolisthesis, spinal stenosis, neoplastic disease, infection and trauma).
Patients were randomly divided into 2 groups to receive either fluoroscopy-guided CESI (CESI group) or else oral treatment with non-steroidal anti-inflammatory drugs (NSAID group). Assignment of patients to groups was done through opaque envelopes, which were randomly selected and opened when patients attended consultation.
All patients were clinically evaluated following the guidelines of the Spanish Society for the Study of Diseases of the Spine (GEER).12 Data on gender, age, anthropometric characteristics, profession, civil status, characteristics and mean intensity of pain and level of disability and impact on quality of life caused by it were collected by elaborating a protocolized questionnaire with a visual analog scale (VAS)13 and an Oswestry14 disability index associated to pain and satisfaction with the treatment received. The level of degenerative discal disease observed in patients through MRI scans was classified according to the Pfirrmann15 criteria and evaluated by examining Modic-type16 changes. We obtained measurements of the intensity of pain, disability and their impact on quality of life by repeating all the questionnaires during reviews conducted after 1, 3 and 6 months.
We considered that the treatment had been successful when patients reported a reduction of pain of at least 50% as measured by a VAS, whilst we labeled it as a failure when patients achieved a lower or no reduction of their pain.
MethodsSurgical procedures were carried out at the Outpatient Surgery Unit by a surgeon specializing in Orthopedic Surgery and Traumatology, with preferential commitment to the vertebral column, as well as a fourth year resident of Orthopedic Surgery and Traumatology with practical experience in spinal surgery who had completed his learning curve, under direct supervision of the surgeon.
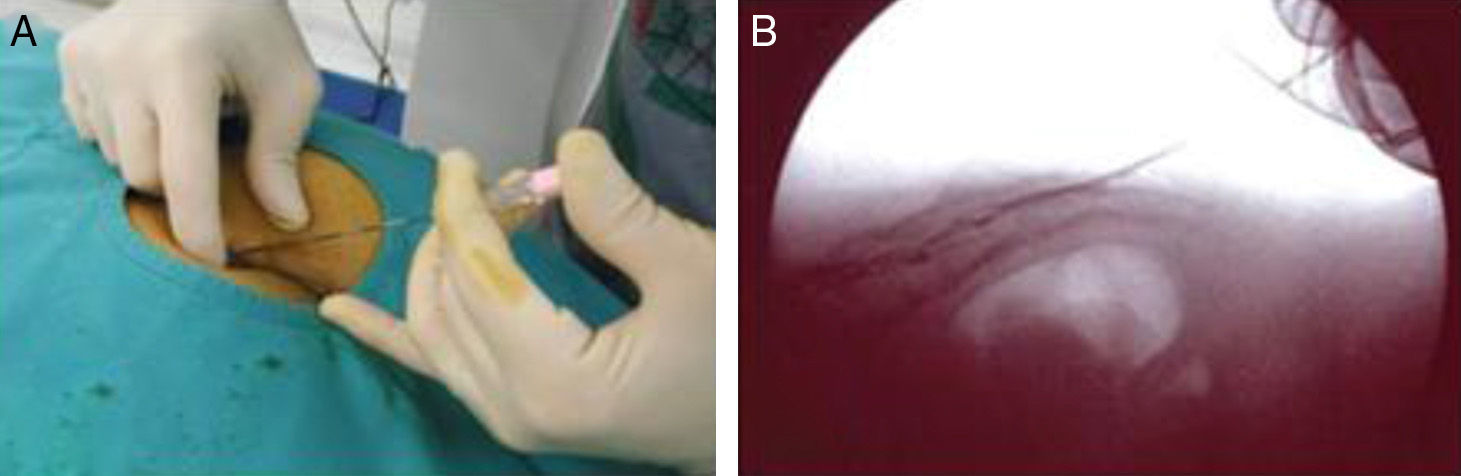
Caudal epidural infiltration techniquePatients in the CESI group were injected with 10ml of ropivacaine 2% (Naropin®), a long-lasting, amide-type, local anesthetic, 3 vials of 1ml triamcinolone acetonide 40mg/ml (Trigon Depot®), a corticosteroid with an intense anti-inflammatory effect, and 20ml of 0.9% saline solution (PSS). Infiltrations were always applied in the surgical area, under radiological control and with sterile conditions in the sacroanal area. Patients were placed in a prone position, with the head turned to one side, in a radiolucent surgical table in a jack-knife position, with hips on the angular point of the operating table, and lowering the legs. Thus, the sacrococcygeal region was left in the raised position, facilitating surgical access. The sacral hiatus was located between the 2 sacral horns, in the midline, near the upper portion of the gluteal cleft. In order to make the procedure more tolerable, local anesthesia was applied in the references marked on the skin and subcutaneous soft tissues. Infiltrations were carried out using an 18G lumbar puncture needle. The needle was placed on the skin and then entered directly through the sacrococcygeal ligament. Once the needle pierced the ligament and was located in the caudal spinal canal, it was made to advance 1–2cm within the caudal canal. The stylet of the cannula was then removed, always under non-ionic contrast control to ensure correct location of the spinal cannula. Once the position of the needle was confirmed, we proceeded to introduce the solution prepared (Fig. 1).17
(A) The sacral hiatus is located between the 2 sacral horns, in the midline, near the superior part of the gluteal cleft. The needle was advanced through the sacrococcygeal ligament and then advanced 1–2cm within the caudal canal. (B) Control was carried out through non-ionic contrast to ensure the correct placement of the spinal cannula.
Patients assigned to the NSAID group followed a set of multifactorial, non-surgical measures, which included the scheduled and regular use of NSAIDs, a physical fitness and functional rehabilitation program and medical advice in order to follow a behavioral treatment for the care of the back.18
Statistical analysisCalculation of the sample size was performed based on the relevant literature of previous comparative studies with epidural steroid injections which had used sample sizes of between 20 and 30 participants per treatment group.19–22 Thus, we estimated a sample size of 21 participants per group to be sufficient for this study, using a desired power of 0.8 and an alpha of 0.05. We created an Excel® for Windows database in which the fieldwork data was entered. The software used for the statistical treatment of the data was SPSS® Statistics Standard. We used the Chi-square and Fisher exact tests, if required, to analyze the association between qualitative variables, and the Wilcoxon and Student t tests, if required, and analysis of variance to compare the means. Significance was set at a value of p equal to or less than 0.05.
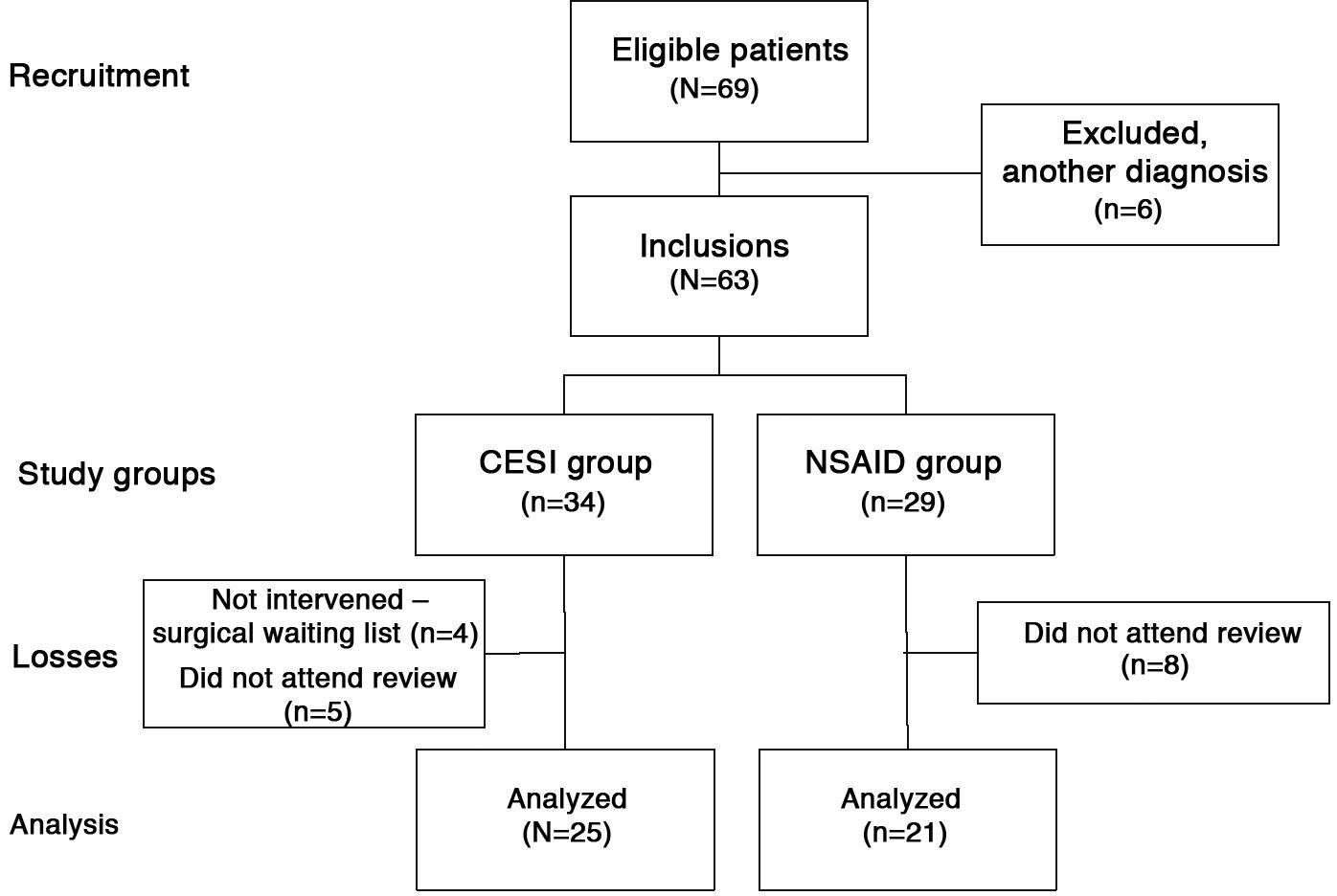
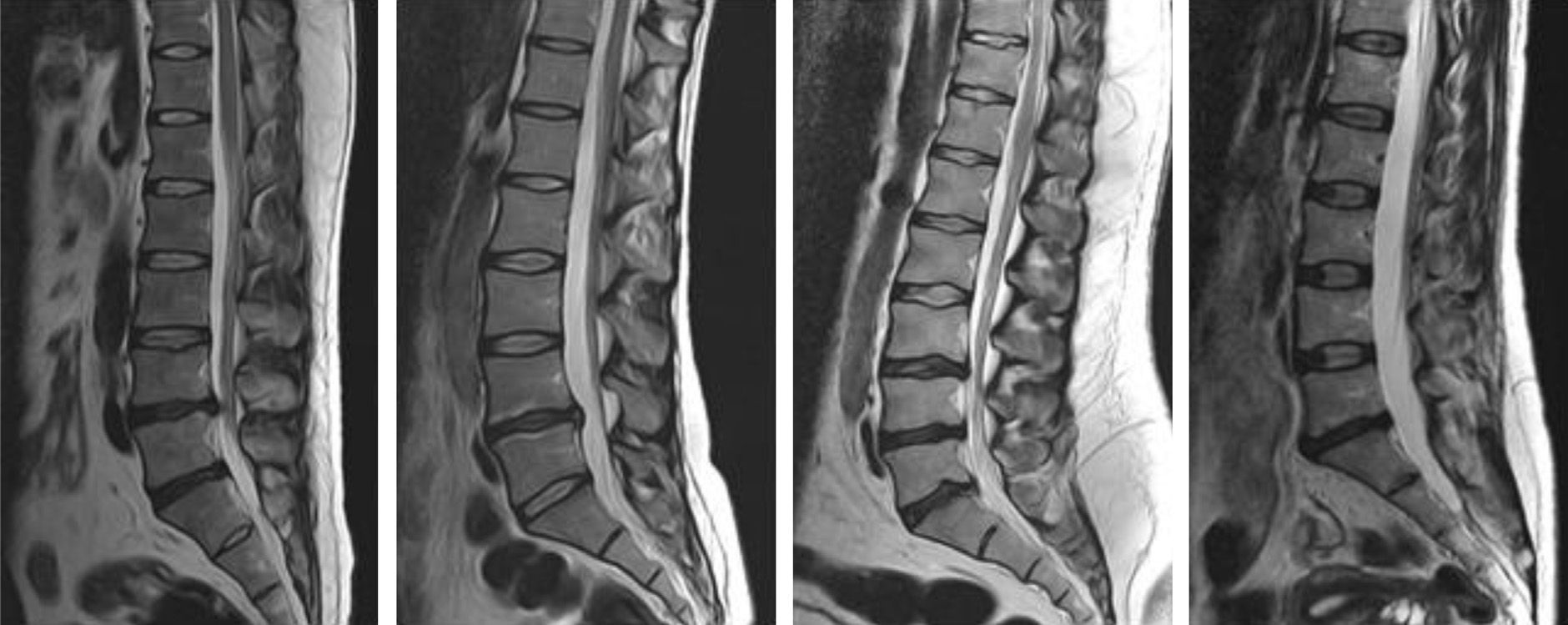
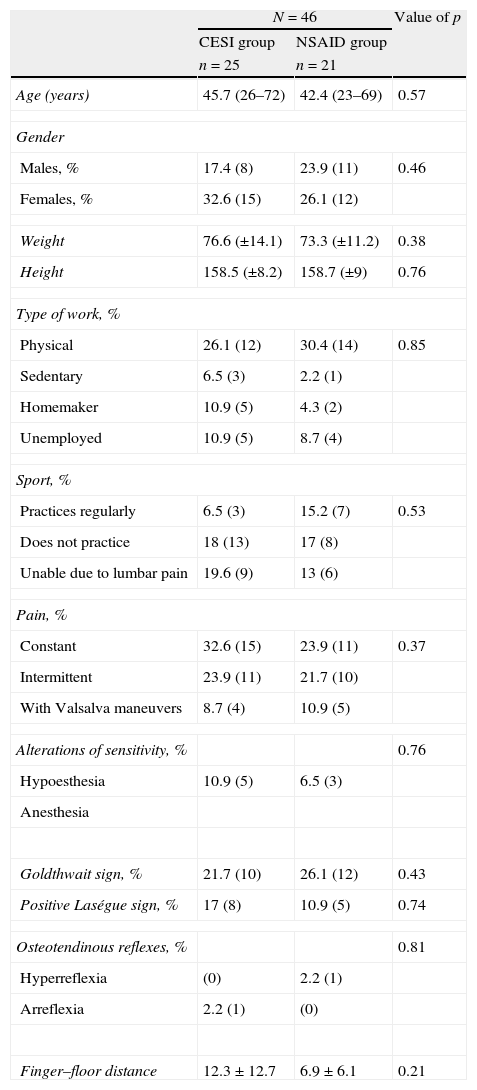
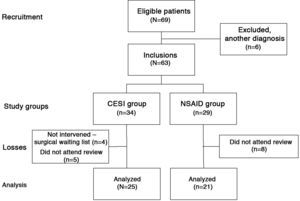
ResultsOf the 69 patients initially included in the study, 6 of them subsequently presented another, prior, specific diagnosis as the cause of their pain, 13 did not attend their scheduled reviews on several occasions, and 4 cases could not complete the study because they were still in the waiting list for CESI at the end of the study. The final number of patients who completed the study was 46, with 25 patients in the CESI group and 21 patients in the NSAID group (Fig. 2). Baseline characteristics were similar between the 2 groups, with a homogeneous distribution of data for the age variable. However, data corresponding to other numeric variables did not fit the normal curve, including the time suffering pain and the finger-floor distance. Of the 46 patients, 19 were male (41.3%) and 27 were female (58.7%), with a mean age of 44 years (range 23–72 years). All patients in the study suffered lumbar pain and, in addition, 12 patients (26%) also suffered pain radiating to the lower limbs. The time which patients had been suffering pain for ranged between 3 and 180 months, with a mean value of 87.3 months. The demographic, clinical and examination characteristics of patients are summarized in Table 1. According to the radiographic findings, all patients presented signs of lumbar degenerative disk disease according to the Pfirrmann classification,15 affecting 1–4 levels, and 8.7% presented type Modic-type changes16 in adjacent vertebral endplates (Fig. 3).
Baseline demographic, clinical and exploration characteristics of the patients in the study.
| N=46 | Value of p | ||
| CESI group | NSAID group | ||
| n=25 | n=21 | ||
| Age (years) | 45.7 (26–72) | 42.4 (23–69) | 0.57 |
| Gender | |||
| Males, % | 17.4 (8) | 23.9 (11) | 0.46 |
| Females, % | 32.6 (15) | 26.1 (12) | |
| Weight | 76.6 (±14.1) | 73.3 (±11.2) | 0.38 |
| Height | 158.5 (±8.2) | 158.7 (±9) | 0.76 |
| Type of work, % | |||
| Physical | 26.1 (12) | 30.4 (14) | 0.85 |
| Sedentary | 6.5 (3) | 2.2 (1) | |
| Homemaker | 10.9 (5) | 4.3 (2) | |
| Unemployed | 10.9 (5) | 8.7 (4) | |
| Sport, % | |||
| Practices regularly | 6.5 (3) | 15.2 (7) | 0.53 |
| Does not practice | 18 (13) | 17 (8) | |
| Unable due to lumbar pain | 19.6 (9) | 13 (6) | |
| Pain, % | |||
| Constant | 32.6 (15) | 23.9 (11) | 0.37 |
| Intermittent | 23.9 (11) | 21.7 (10) | |
| With Valsalva maneuvers | 8.7 (4) | 10.9 (5) | |
| Alterations of sensitivity, % | 0.76 | ||
| Hypoesthesia | 10.9 (5) | 6.5 (3) | |
| Anesthesia | |||
| Goldthwait sign, % | 21.7 (10) | 26.1 (12) | 0.43 |
| Positive Laségue sign, % | 17 (8) | 10.9 (5) | 0.74 |
| Osteotendinous reflexes, % | 0.81 | ||
| Hyperreflexia | (0) | 2.2 (1) | |
| Arreflexia | 2.2 (1) | (0) | |
| Finger–floor distance | 12.3±12.7 | 6.9±6.1 | 0.21 |
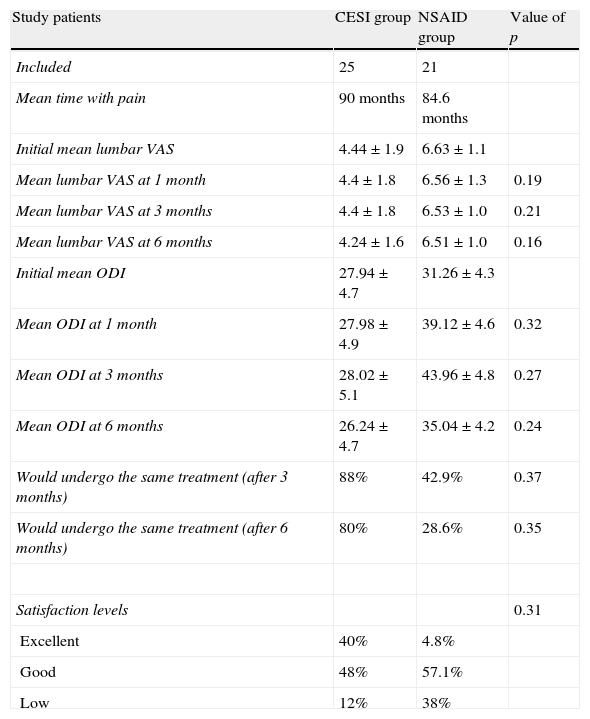
None of the patients experienced adverse effects after CESI or taking NSAIDs. Regarding the analysis of the evolution of lumbar pain and pain-related disability (Table 2), the mean values of the VAS and Oswestry questionnaires did not reflect significant improvement after 4 weeks of treatment in any of the 2 groups. There were no statistically significant differences in the values studied between the 2 groups (p=0.32). At 12 weeks of treatment, the mean values for the VAS and Oswestry questionnaires did not reflect any significant improvement in the CESI group, whilst the worsening in the Oswestry questionnaire was maintained in the NSAID group. However, this difference was still not statistically significant (p=0.27). Finally, the mean values for the VAS and Oswestry questionnaires at 6 months of treatment continued to show no significant improvement, although the mean values in both the CESI and the NSAID groups did improve compared to the values obtained at 12 weeks (p=0.24).
Evolution of lumbar pain measured through a VAS and disability caused by lumbar pain measured through the Oswestry disability index in patients included in both treatment groups throughout the follow-up period.
| Study patients | CESI group | NSAID group | Value of p |
| Included | 25 | 21 | |
| Mean time with pain | 90 months | 84.6 months | |
| Initial mean lumbar VAS | 4.44±1.9 | 6.63±1.1 | |
| Mean lumbar VAS at 1 month | 4.4±1.8 | 6.56±1.3 | 0.19 |
| Mean lumbar VAS at 3 months | 4.4±1.8 | 6.53±1.0 | 0.21 |
| Mean lumbar VAS at 6 months | 4.24±1.6 | 6.51±1.0 | 0.16 |
| Initial mean ODI | 27.94±4.7 | 31.26±4.3 | |
| Mean ODI at 1 month | 27.98±4.9 | 39.12±4.6 | 0.32 |
| Mean ODI at 3 months | 28.02±5.1 | 43.96±4.8 | 0.27 |
| Mean ODI at 6 months | 26.24±4.7 | 35.04±4.2 | 0.24 |
| Would undergo the same treatment (after 3 months) | 88% | 42.9% | 0.37 |
| Would undergo the same treatment (after 6 months) | 80% | 28.6% | 0.35 |
| Satisfaction levels | 0.31 | ||
| Excellent | 40% | 4.8% | |
| Good | 48% | 57.1% | |
| Low | 12% | 38% |
CESI: caudal epidural steroid infiltration; NSAID: non steroidal anti-inflammatory drugs; ODI: Oswestry disability index; VAS: visual analog scale.
When asked if they would undergo the same treatment again, at 3 months, 42.9% (95% CI: 26.2–58.3) of the patients in the NSAID group responded affirmatively. However, at 6 months, only 28.6% (95% CI: 23.9–53.1) maintained this affirmative response. Regarding the CESI group, at 3 months, 88% (95% CI: 76.2–100.7) of the patients responded that they would undergo infiltration again. This percentage was similar after 6 months, with 80% (95% CI: 69.8–93.8) of patients responding that they would repeat the infiltration treatment.
Regarding patient satisfaction with the treatment received at the end of the follow-up period, only 1 patient (4.8%) in the NSAID group reported a good or excellent result, 12 patients (57.1%) reported having achieved an acceptable result, and 8 patients (38%) reported a low level of satisfaction with the result. This translated into a good/acceptable level of satisfaction for 61.9% (95% CI: 38.1–84.9) of cases. On the other hand, at the end of the follow-up period in the CESI group, 10 patients (40%) reported a good or excellent result, 12 patients (48%) reported a satisfactory result, and 3 patients (12%) reported a low level of satisfaction with the result. This translated into a good/acceptable level of satisfaction for 88% (95% CI: 76.2–100.7) of cases.
DiscussionThis was a prospective, randomized study comparing the effectiveness of CESI versus treatment with NSAIDs in the context of chronic lumbar pain with a discogenic origin. There are very few studies in the literature which cover this topic.
All of our patients presented symptoms consistent with degenerative disk disease confirmed by MRI. The injections were performed using fluoroscopic control and verified through the use of previous contrast. However, we were not able to establish the superiority of CESI treatment over NSAIDs.
The traditional concept has been that the characteristic pain which defines disk disease is caused by direct compression by the disk on the nerve root. However, the natural history usually progresses toward the disappearance of pain over time, despite compression being maintained.23,24 Direct compression of the root causes local axonal damage and ischemia. Furthermore, the degenerated disk, and especially the nucleus pulposus, is a biologically active tissue which triggers a chain of inflammatory-type, pathological events.25 The genesis of pain is influenced by inflammatory, biomechanical, vascular, and, of course, compressive phenomena. Following annulus fibrosus rupture, the outpour of the nucleus pulposus will not only irritate the adjacent root, but will also sensitize the annular fibers, and any movement by the lumbar spine which increases the pressure within the disk will cause pain.26 Inflammation plays a key role in this process. The nucleus pulposus is an avascular structure and when it comes into contact with nerve structures it is perceived as an antigen which triggers an intense inflammatory response. The simple rupture of the annulus fibrosus triggers an inflammatory response with increased levels of phospholipase A and cytokine production.3 Therefore, radiculalgia and lumbalgia secondary to disk disease would not be explained by a mere mechanism of direct compression, but instead would be part of a local inflammatory process.
The beginning of the use of drugs injected into the epidural space for the treatment of lumbar pain dates back to the first half of the 20th century.1 Viner27 began injecting large volumes of saline solution and procaine into the lumbar epidural space in an attempt to treat lumbar pain and radiculopathy. Evans28 published his results with a similar procedure in 1930, with only 14% success in 40 patients. The publication of the use of steroids in the epidural space took place in 1960 for the first time. Brown29 reported complete and transient relief in 4 patients with long-standing sciatica who had been treated with methylprednisolone injections.
The routes described for infiltration into the epidural space are the caudal, interlaminar and transforaminal. The choice of route is generally dependent on the experience and preference of each surgeon. The literature contains comparative studies between the 3 alternatives, without a demonstrated superiority by any of them.19,30 The interlaminar route offers the possibility of using smaller drug volumes than the caudal route. However, the risk of dural puncture is less in the caudal route. The transforaminal route deposits the drug closer to the affected root than the other two. However, the possibility of damaging the root by puncture and, therefore, of causing acute radiculalgia is greater.31 The authors consider the caudal route as a safe technique for epidural infiltration. In our series, we did not observe any local or systemic complications secondary to the use of the caudal route for steroid infiltration into the epidural space. Verification through contrast prior to drug infusion reduces the risk of a false route and increases the safety and efficacy of the technique.
There are very few, well-designed, prospective studies regarding the efficacy of CESI in the literature32 and, out the studies published so far, many offer inconsistent results.6,8,26,33–35 In addition, there are significant discrepancies between the various studies when establishing a comparison of the results of different parameters and different conclusions.10
Dilke et al.36 published a double-blind randomized study with 100 consecutive patients treated by CESI who suffered symptoms consistent with unilateral sciatica. The group of patients was treated with 80mg of epidural methylprednisolone, while the control group received an injection of saline solution. Both groups were comparable with respect to age, occupation, gender, neurological deficits and duration of the symptoms. Patients treated with methylprednisolone reported a greater subjective relief of pain during the first 3 months, took significantly less pain medication, had a higher rate of return to work and a lower rate of subsequent surgery. However, Snoek et al.34 did not find any differences between the treated group and the control group in a double-blind study with 51 patients who suffered nerve root compression. The 2 study groups were comparable and suffered nerve root compression confirmed by myelography. The evaluation of results was performed just 24–48h after injection (the maximum response to steroids may be delayed by up to 6 days), and the follow-up study simply consisted of a review of medical records to confirm which patients had required subsequent surgery. Although the treated group reflected greater improvement in mobility, lumbar, motor and radicular symptoms, as well as a lower consumption of analgesics, the differences were not statistically significant. Although a greater percentage of treated patients reported improvement (67% versus 42%) and physiotherapists assessed more treated patients as improved compared to those in the control group (70% versus 43%), these differences did not reach sufficient statistical significance and the authors did not report a superiority of CESI over placebo. Power et al.37 recognized an absolute failure of the use of CESI, therefore considering it unethical to continue the study after their 16 patients showed a complete lack of pain relief following injections of bupivacaine and methylprednisolone, although 10 patients did report some initial relief (from 24h to 3 months), and none could avoid surgical treatment.
Watts and Silagy38 conducted a meta-analysis of various studies regarding CESI related to lumbar radiculopathy (11 randomized trials with 907 patients) and observed that, despite a generally favorable initial result, there was a rapid deterioration of these results over time.
The results obtained in our study were consistent with those studies which failed to find a clear proof of the benefit of CESI treatment in the context of chronic low back pain due to degenerative disk disease. Treatment by CESI has not demonstrated superiority over treatment with NSAIDs, since the values for the VAS and Oswestry questionnaires showed no significant improvement throughout the evolution.
Among all the results in our study, we would highlight the differences found between the results of the VAS and Oswestry questionnaires compared to the values obtained with the questionnaire on satisfaction with treatment received among patients who underwent CESI. Although no significant differences were found between the study groups regarding functional improvement in the evaluation of results in the Oswestry disability questionnaire and the VAS, patients who received caudal epidural steroid infiltration presented higher levels of overall satisfaction (good/acceptable level of satisfaction for 88%) than those treated with NSAIDs (good/acceptable level of satisfaction for 61.9%). This apparent disparity of the results obtained from the pain and related disability questionnaires compared to satisfaction may actually be offering complementary results because, despite the discreet results, patients may be positively evaluating the efforts to provide treatment for their chronic disease.
Another result which subjectively supports the use of caudal epidural infiltration is the fact that 88% of patients at 3 months and 80% at 6 months would repeat the epidural treatment, whilst only 42.9% at 3 months and 28.6% at 6 months would repeat the treatment with NSAIDs.
CESI is a minimally invasive surgical technique. As such, it does not offer considerable difficulties, its use does not limit any subsequent surgery and its associated morbidity is very low. However, its actual effectiveness in patients suffering chronic lumbar pain with a discogenic origin has not yet been established. The limitations of our work, which may be taken into account when conducting future studies, include designing randomized studies with a larger sample size but at the same time using more stringent inclusion criteria, stratification of patients, the use of a control group, the elaboration of a definitive diagnostic method and the exploration of the possible clinical implications of the long-term use of steroids. Meanwhile, taking into account the results of this study, the authors believe that CESI should be applied with caution, and only after adequately informing patients of realistic expectations following the treatment.
Level of evidenceLevel of evidence ii.
Ethical responsibilitiesProtection of people and animalsThe authors declare that this investigation did not require experiments on humans or animals.
Confidentiality of dataThe authors declare that they have followed the protocols of their workplace on the publication of patient data and that all patients included in the study received sufficient information and gave their written informed consent to participate in the study.
Right to privacy and informed consentThe authors declare having obtained written informed consent from patients and/or subjects referred to in the work. This document is held by the corresponding author.
Conflict of interestsThe authors have not received any kind funding for this work. Neither have they signed any agreement which will lead them to receive profit or payment from any commercial organization. In addition, no commercial organization has paid or will pay any foundation, educational institution or any other non-profit organization with which the authors are affiliated.
Please cite this article as: Cervera-Irimia J, Tomé-Bermejo F. Infiltración esteroidea epidural por vía caudal en el tratamiento del dolor lumbar crónico de origen discal. Estudio comparativo, prospectivo y aleatorizado. Rev Esp Cir Ortop Traumatol. 2013;57:324–332.