To achieve in the reconstruction of the anterior cruciate ligament a graft with strength, tension and low comorbidity is fundamental.
An emerging concept is that a graft diameter of less than 7mm carries a greater risk of re-rupture and instability. Consequently, different methods are being sought to predict intra-surgical size.
The objective is to predict the size of the hamstring graft by measuring the area of the semitendinous and gracilis tendon with magnetic resonance imaging (MRI).
MethodologyWe carried out an observational retrospective study of 56 patients. They underwent anterior cruciate ligament reconstruction with 4-GST hamstring graft. The parameters evaluated were anthropometric data, hamstring graft diameter, area of gracilis and semitendinosus tendon in MRI. The measurements were made by three independent evaluators.
ResultsThe mean diameter of the intrasurgical graft was 8.46mm, in the MRI the area of the gracilis was 8875mm and the semitendinosus area was 13,068mm. Their mean was 22.12 for the automatic measurement and 21.53 for the manual measurement. The interobserver correlation was regular for the automatic measurement (ICC=.595) and low for the manual measurement (ICC=.446). The result of the intraobserver correlation was excellent (ICC=.917). We did not obtain a statistical correlation between the measurement of areas and the increase of the graft diameter (R=.069, P=.63).
ConclusionWe determined with our results that the intrasurgical graft size is not predictable with the measurement of the area of the gracilis and semitendinosus tendon on the MRI.
Conseguir en la reconstrucción de una rotura completa del ligamento cruzado anterior una plastia con fuerza, tensión y poca comorbilidad es fundamental.
Un concepto emergente es que plastias menores de 7mm de diámetro tienen mayor riesgo de rerrotura e inestabilidad. Consecuentemente se están buscando distintos métodos que predigan el tamaño intraquirófano de la misma.
El objetivo es predecir el tamaño de la plastia de isquiotibiales mediante la medición del área del tendón semitendinoso y grácil con resonancia magnética nuclear (RMN).
MetodologíaEstudio observacional restrospectivo de 56 pacientes, en los que se realiza reconstrucción tetrafascicular del ligamento cruzado anterior mediante plastia de isquiotibiales.
Los parámetros evaluados han sido: datos antropométricos, diámetro de la plastia intraquirófano, área del tendón del grácil y semitendinoso en RMN.
Las mediciones fueron realizadas por tres evaluadores independientes.
ResultadosEl diámetro medio intraquirófano de la plastia fue de 8,46mm; la medición mediante RMN del área del grácil fue de 8.875mm y del semitendinoso de 13.068mm. La suma de ellas fue de 22,12 para la medición automática y de 21,53 para la manual.
La correlación interobservador fue regular para la medición automática (ICC=0,595) y baja para la forma manual (ICC=0,446). El resultado de la correlación intraobservador fue excelente (ICC=0,917).
No obtuvimos una correlación estadística entre la medición de áreas y el aumento del diámetro de la plastia (R=0,069, P=0,63).
ConclusiónDeterminamos con nuestros resultados que la medición de la plastia intraquirófano de isquiotibiales y la medición mediante RMN no es un método adecuado para predecir su tamaño.
Total rupture of the anterior cruciate ligament (ACL) is one of the most common injuries in knee trauma. The gold standard treatment in adults for this is its reconstruction.
Reconstruction through 4-GST hamstring graft is what has proven to bring about optimum clinical outcomes, with a low morbidity compared with reconstructions using the quadriceps tendon or BTB (patella).1,2
The most common complication after reconstruction of the ACL is recurrent instabililty,3 for which a multitude of clinical and biomechanical trials have been conducted to analyse this surgical failure.
One major consideration to bear in mind is the size of the hamstring graft, since this may affect surgical outcome.4,5
Obtaining graft diameters above 7mm is the aim, because smaller diameters have a greater probability of failing.6,7 It is not always possible to obtain an appropriate autologous thickness, due to the anatomical variability of them. In these cases, should we consider obtaining a different type of graft or alternative surgery?
Different methods have been developed to try to predict graft size: height, weight, sex, preoperative algorithms and images, but all of them have proven to be inconclusive.8,9
The aim of this study was to demonstrate a possible correlation between preoperative measurements using nuclear magnetic resonance imaging (NMR) in the region of the gracilis and semitendinous tendons and the diameter of the graft measured during surgery.
The hypothesis was that our method of measurement should be reproducible, reliable and valid in the prediction of intrasurgical graft size.
Material and methodOur study was approved by the Ethics Committee of our hospital. We conducted an observational, retrospective study of 56 patients who underwent a reconstruction of the ACL with a 4-GST hamstring graft. Inclusion criteria were: patients who had undergone preoperative NMR imaging in our hospital and who had the size of the graft shown on the surgical data sheet. A single exclusion criterion was used: we excluded patients who were not having a primary reconstruction. Our period of recruitment was three years (2014–2016), with data collection being made in 2017.
Anthropometric data such as age, sex, height, weight, body mass index were collected.
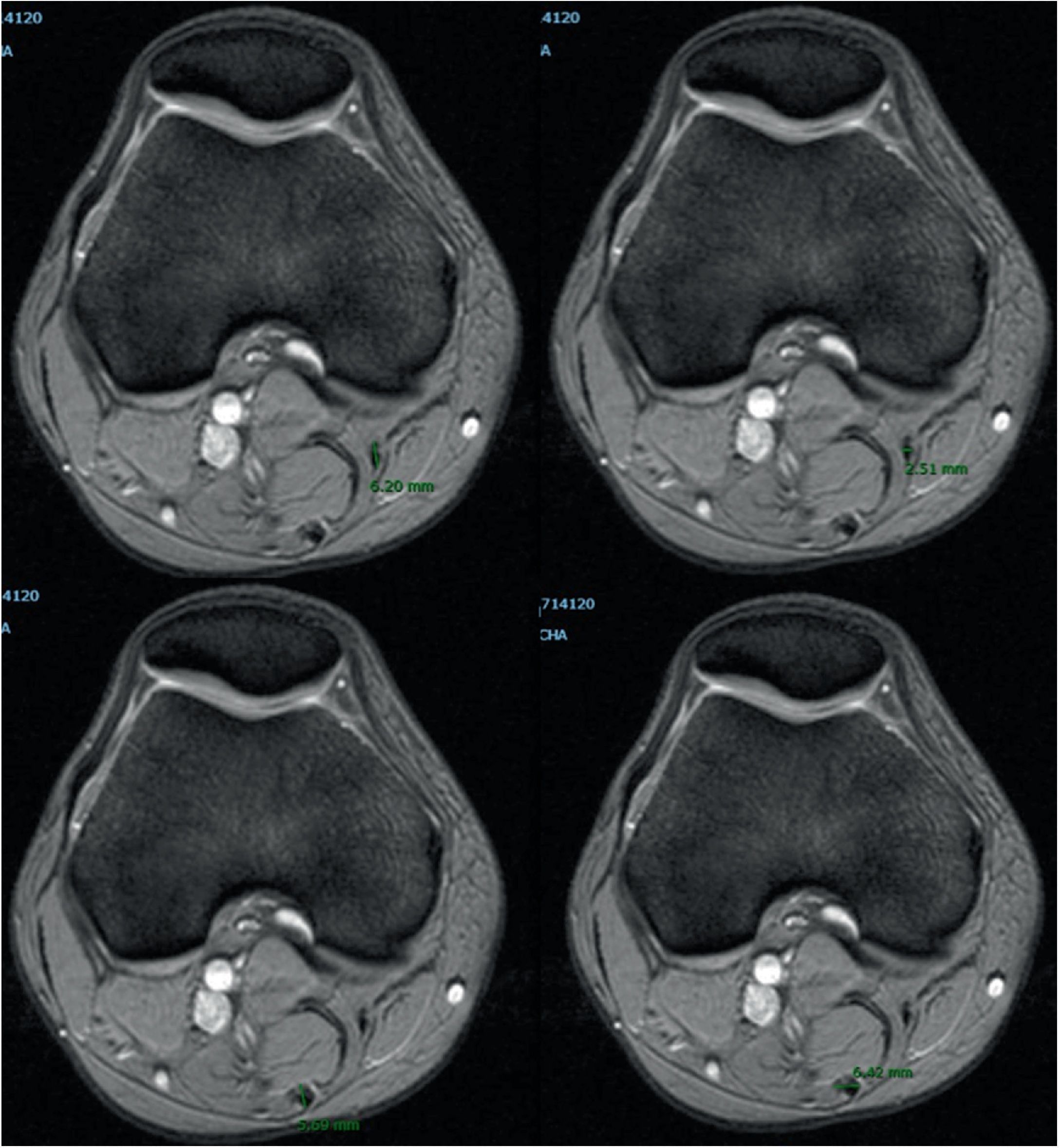
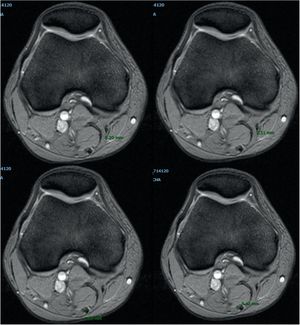
NMR measurement techniqueThe knee was flexed between 10° and 20° in a systematic manner when the imaging test was made. The cut size was 3.5mm in thickness with a matrix of 512×256 and the sequence used for measurement was axial slices with fat suppression.
Measurement technique used to assess the area of the gracilis and semitendinosus tendon (Figs. 1 and 2)Method A. Measurement of the gracilis and semitendinosus tendon was made using the technique described by Bickel and Wernecke.10,11 An axial slice was used where the distal femur would present with the widest cut of the lateral condyle. Using our hospital IT application (Carestream) auto-tracing was carried out of the measurement of the area of interest in the preselected image.
Method B. Two weeks later, at the same level of femoral cut, a second manual measurement was made. The long and short diameter of each tendon was measured. This diameter was divided into two to calculate the short and long radius of the tendon area. We were thus able to apply the formula of any circumference: short radius×long radius×the number pi.
The two measurements were made by three independent evaluators. Data collection of the graft at the time of surgery was blind for each evaluator.
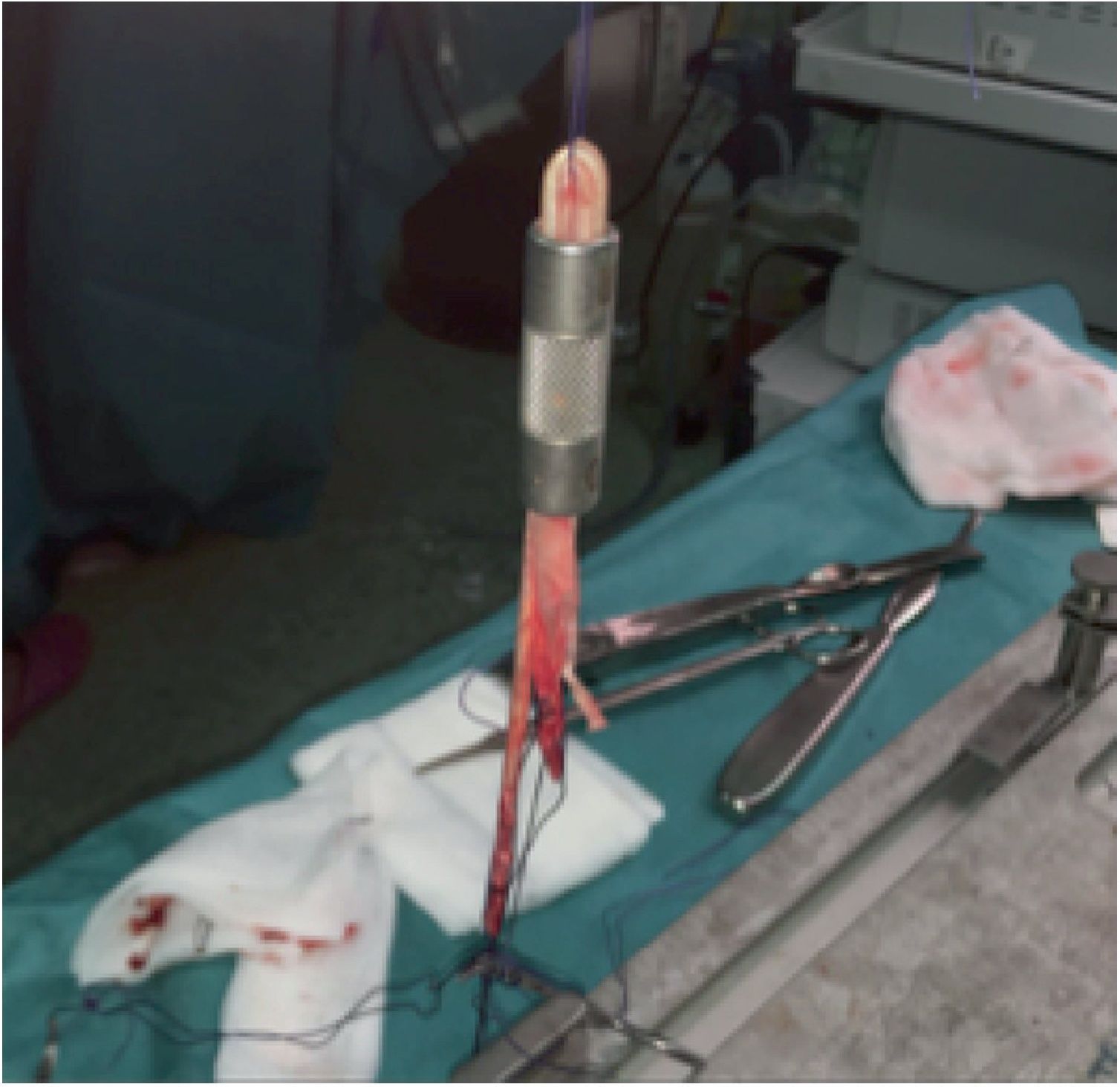
Obtainment of the hamstring graft diameterHamstring graft diameter was obtained by means of a longitudinal incision of 3–5cm medially centred to the anterior tibial tuberosity (Fig. 3). Following incision of the sartorius fascia, each tendon was identified and carefully isolated. The gracilis and semitendinosus tendons were referenced with number 2 nylon thread (Fig. 4).
After preparing the graft, the measurement was made with a device which presented with increments of 1mm diameter (Fig. 5). The shortest diameter through which the graft easily fitted was chosen for making the tunnel. We tried to avoid any possible bias by having the same surgeon carry out the measuring.
Statistical analysisVariables were analysed using the Kolmogorov–Smirnov and Shapiro–Wilko test to see if they followed a normal distribution.
Bivariate correlation was used to assess the correlation between the diameter of the graft compared with height and weight.
We used the Pearson (Pearson's r) correlation test to determine any existing correlation between the two measurements made (method A and B) and the diameter of the graft measured during surgery.
For reproducibility of the test the intra (method A and B) and interobserver (three researchers) correlation coefficient was analysed for the measurement made in the NMR.
A P value of .05 was considered to be statistically significant. All analysis was performed with the SPSS 21 (SPSS Inc., Chicago, Illinois) software programme.
ResultsFifty six patients were recruited for our study. The mean age at the time of surgery was 30 years (range 14–51), and there were 45 men (80%) and 11 women (20%). The mean height was 172cm (range 150–187), whilst mean weight was 76.92kg (range 47–104kg), all of which followed a normal distribution.
Mean size of the intrasurgical graft was 8.46mm (range 7–10mm). The distribution of its diameter was: 7mm (9 cases), 8mm (19 cases), 9mm (22 cases), 10mm (6 cases).
Measurement of the gracilis tendon presented with a mean area of 8.875mm2 (range 3.45–16.41mm2) and the semitendinosus tendon was of 13.068mm2 (range 6.09–19.36mm2). The mean area of measurement using method A was 22.12mm2 (range 10.85–34.61mm2) and the mean are using method B was 21.53mm2 (range 9.34–34.02mm2).
Reproducibility of the measurementsThe interobserver correlation of the three evaluators was slight to moderate for method A, ICC: .595 (range .442 to .727) and low for method B, ICC .446 (range .275 to .610).
If we compare it with the intraobserver correlation for the two actual measurements it was excellent, ICC=.917 (range .858–.952).
Correlation between the area measured in the NRM and graft sizeThe 4-GST hamstring graft had no statistically significant correlation to the area measured in the NMR imaging. Method A showed a P=.63 with R=−.069 and method B a P=.668 with R=−.062 for the Pearson correlation. The use of a formula to predict increase in graft diameter according to the increase in the measurement of the mean area of the NMR did not therefore occur.
Anthropometric data and prediction of graft sizeThe correlation between the graft diameter compared with weight and height did not show up any statistically significant differences (weight: ICC=.12, P=.356 and height: ICC=.185, P=.182).
DiscussionOur study intended to find a method to predict the graft diameter of autologous hamstring tendons prior to surgery so as to select the surgical technique to be used. We sought to do this using measurements of the graft areas in the NMR. However, our results did not correlate with the two measurements, whilst for other authors they did.1,3,6,10–13 At present there are no studies which indicate the non existence of any correlation between the area measured in the NMR and the diameter of the graft, but Yasumoto already advanced the same result with CT reconstructions.14
The first aspect to analyse was that there was a fault in the measurement. In our study we had an excellent intraobserver correlation.15 We interpreted this result as being that the measurement made by the usual tools of our radiography systems and the measurement made using a formulary or manually drawn will present with the same result if performed by the same observer, since the measurements were taken two weeks apart in each patient. However, if we compare these between the different observers, the interobserver correlation falls to low. The interpretation of this is that there is a great deal of variability in the interpretation of the greyscale in the NMR, with the consequent possible errors when establishing the cut-off point in a ROC curve.
The second aspect is that we had a small sample size for obtaining good correlation. Only the studies by Grawe3 and Leiter12 with 84 and 109 patients respectively are higher. Erquicia,6 Bickel,10 Beyzadeoglu,1 Wernecke,11 Galanis13 had a lower sample size than ours.
There are only a few articles in the literature which predict graft size in ACL reconstruction with NMR. We believe this is because of a possible publication bias.
Different studies have attempted to find a correlation with anthropometric data of patients and the diameter of the graft.7 We did not obtain statistically significant differences between weight and height with respect to graft measurement. In published studies any type of result can be found. Hamada16 found there was a slight correlation with weight (ICC=.292, P=.011) but did not find one with height (ICC=.389, P=.0004). Bickel10 did not find any correlation (weight=.31, P>.05 and height=.25, P>.05), and on the other extreme we found that Park demonstrated a correlation between weight (.427) and height (.477) both with a P>.05.7 This is probably not a good procedure for predicting graft size.
ConclusionAccording to our results we cannot determine that measurement of the semitendinous and gracilis tendon in the NMR enables us to predict intrasurgical graft size. We believe this is not a simple, reproducible or reliable method.
Conflict of interestThe authors have no conflict of interest to declare.
Please cite this article as: Oliva Moya F, Sotelo Sevillano B, Vilches Fernández JM, Mantic Lugo M, Orta Chincoa J, Andrés García JA. ¿Podemos predecir el tamaño de la plastia de los isquiotibiales para la reconstrucción del ligamento cruzado anterior mediante resonancia magnética? Rev Esp Cir Ortop Traumatol. 2020;64:145–150.