Calcific tendinitis of the rotator cuff is a common cause of shoulder pain. The aim of the present study was to show a rare presentation of calcific tendinopathy of the shoulder, the intraosseous extension, which can be mistaken for a bone tumour or an infectious disease.
MethodsTwo clinical cases of calcific tendinopathy of the shoulder with intraosseous extension and a review of the literature are presented.
ResultsCortical erosion, osteolytic lesion in the greater tuberosity and perilesional oedema were observed in both cases. Good results were achieved with shoulder arthroscopy including lesion debridement and reinsertion of the tendon in the greater tuberosity with an anchor.
ConclusionIn the presence of an osteolytic lesion with perilesional oedema in the greater tuberosity, the intraosseous expansion of a calcifying tendinopathy should be included in the differential diagnosis. In our cases the arthroscopic treatment was successful.
La tendinitis calcificante del manguito de los rotadores es una de las causas frecuentes de dolor en el hombro. El objetivo fue dar a conocer una presentación poco habitual de la tendinitis calcificante de hombro, la expansión intraósea, que en muchos casos puede ser confundida con una lesión tumoral o infecciosa, y de esta manera evitar biopsias o tratamientos innecesarios, y presentar nuestra experiencia con el tratamiento artroscópico.
Materiales y métodosSe presentan 2 casos clínicos de tendinitis calcificante de hombro con extensión intraósea y una revisión de las series publicadas.
ResultadosEn ambos casos se observa erosión de la cortical, una lesión osteolítica en la tuberosidad mayor y un edema perilesional. Se obtuvieron buenos resultados con el tratamiento mediante artroscopia de hombro con desbridamiento de la lesión y reinserción del supraespinoso en la tuberosidad mayor mediante un arpón.
ConclusionesAnte una lesión osteolítica con edema perilesional en la tuberosidad mayor, hay que valorar, dentro del diagnóstico diferencial, la expansión intraósea de una tendinitis calcificante. En nuestros casos el tratamiento artroscópico fue eficaz.
Calcific tendinitis of the rotator cuff is a frequent cause of shoulder pain, although in 3%–20% of cases it can be an asymptomatic chance finding.1 It is most common in women between the ages of 40 and 60. It is bilateral only in 10%–20% of cases.2,3 Although calcific tendinopathy has been attributed to several aetiologies, its physiopathology has not yet been clarified.2,4 Calcific tendinopathy is characterised by the deposition of calcium salts that most frequently affects the supraspinatus.1,2 Intraosseous extension in the greater tuberosity of the humerus is a rare complication, but is of major importance because it can lead to differential diagnosis with tumour lesions or infectious processes and to the performance of imaging tests or even unnecessary invasive tests.2,4–6
In calcific tendinopathy with intraosseous extension, cortical erosion and osteolytic lesion at the insertion site of the affected tendon can be seen on imaging tests. Significant perilesional oedema can be observed on magnetic resonance imaging (MRI).4,5,7,8
The outcomes of calcific tendinitis of the rotator cuff with intraosseous extension with arthroscopic debridement of the lesion (including the intraosseous part) are as good as calcific tendinopathy without this complication, without the need for an additional gesture.9
The aim of this paper is to present an unusual presentation of calcific tendinopathy of the shoulder, which can in many cases be confused with a tumour or infectious lesion, and thus avoid unnecessary biopsies or treatment, and to present our experience with arthroscopic treatment.
Material and methodsWe present 2 clinical cases of calcific tendinopathy of the shoulder with intraosseous extension where a differential diagnosis with a tumour lesion was suggested and which were treated arthroscopically.
Clinical case 1A 49-year-old woman, consulting with right shoulder pain (dominant limb) of 10 days duration, with more intense pain in supine decubitus. The pain did not subside with non-steroidal anti-inflammatory drugs. On physical examination the patient presented complete articular balance with pain on active motion, especially on adduction over 80°. Jobe and Hawkins tests were positive. Plain X-ray showed calcification between the humeral head and the acromion (Fig. 1), and an MRI was requested given the suspicion of calcific tendinopathy (Fig. 1).
Plain X-ray of the shoulder, anteroposterior projection: a calcification can be observed between the humeral head and the acromion (upper left image). MRI images: calcification of the supraspinatus can be observed with an osteolytic lesion in the greater tuberosity of approximately 1cm in diameter and significant bone oedema of the humeral head of 36×39mm (upper right, lower right and lower left images).
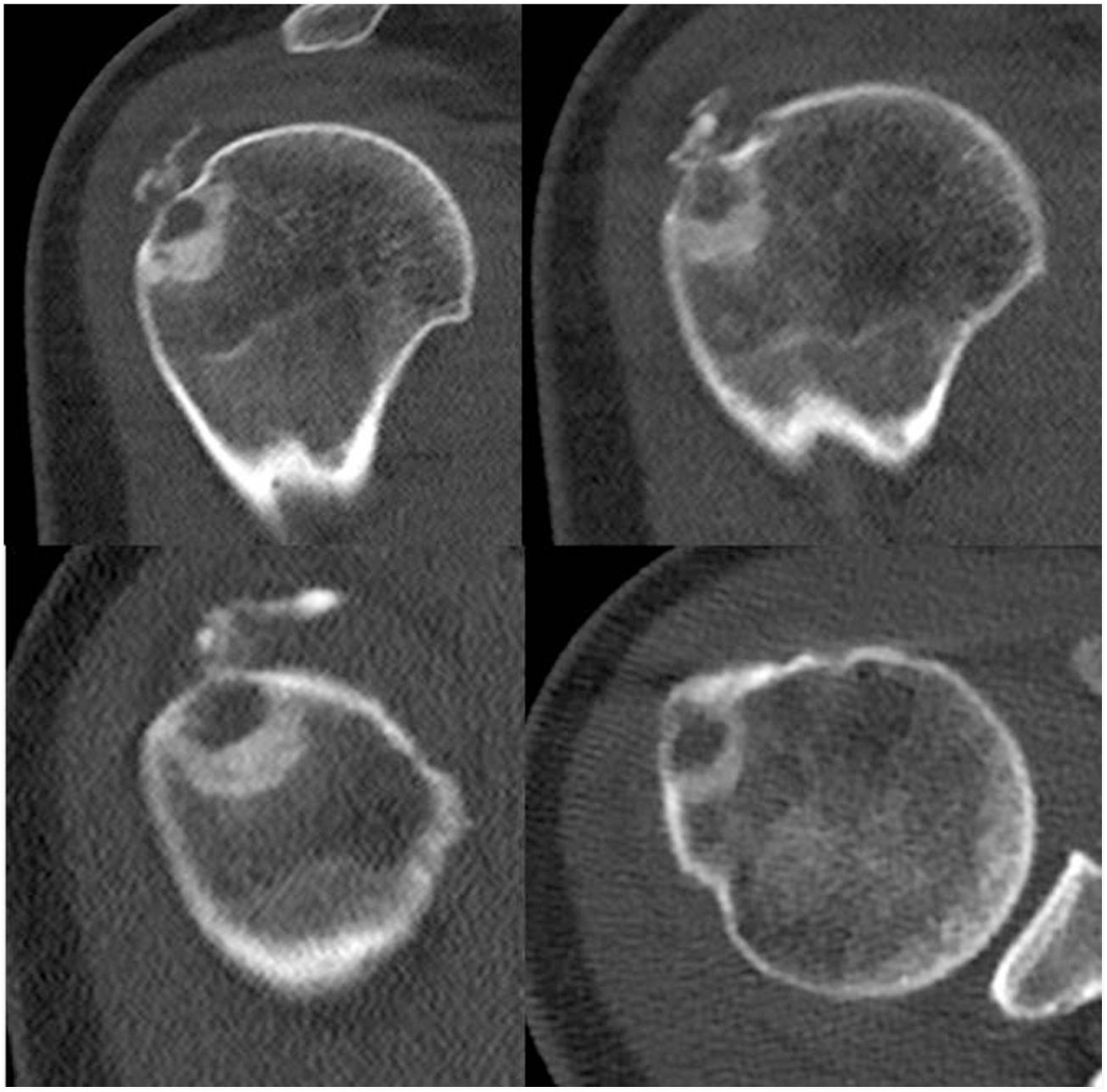
Computerised axial tomography (CT) was recommended to characterise the bone lesion (Fig. 2). The radiological findings could have corresponded to osteoid osteoma (under 2cm), the presence of changes secondary to insertional enthesopathy of the supraspinatus were less likely given the concomitant calcific tendinopathy. A differential diagnosis between both lesions was proposed and a scan performed that was compatible with a diagnosis of osteoid osteoma. The patient did not improve with acetylsalicylic acid (ASA) and the same symptoms persisted. The case was referred to the referral tumour unit for study and treatment if appropriate. The tumour committee ruled out the presence of a tumour lesion and referred the patient back to our department for treatment, with a diagnosis of calcific tendinopathy of the right shoulder with intraosseous extension.
CT images. A lytic cortical lesion dependent on the external side of the humeral head with expansive behaviour can be observed, accompanied by a peripheral osteo-condensing area and peripheral hypodensity in relation to the bony oedema present on the MRI, showing radiological characteristics of local aggressiveness.
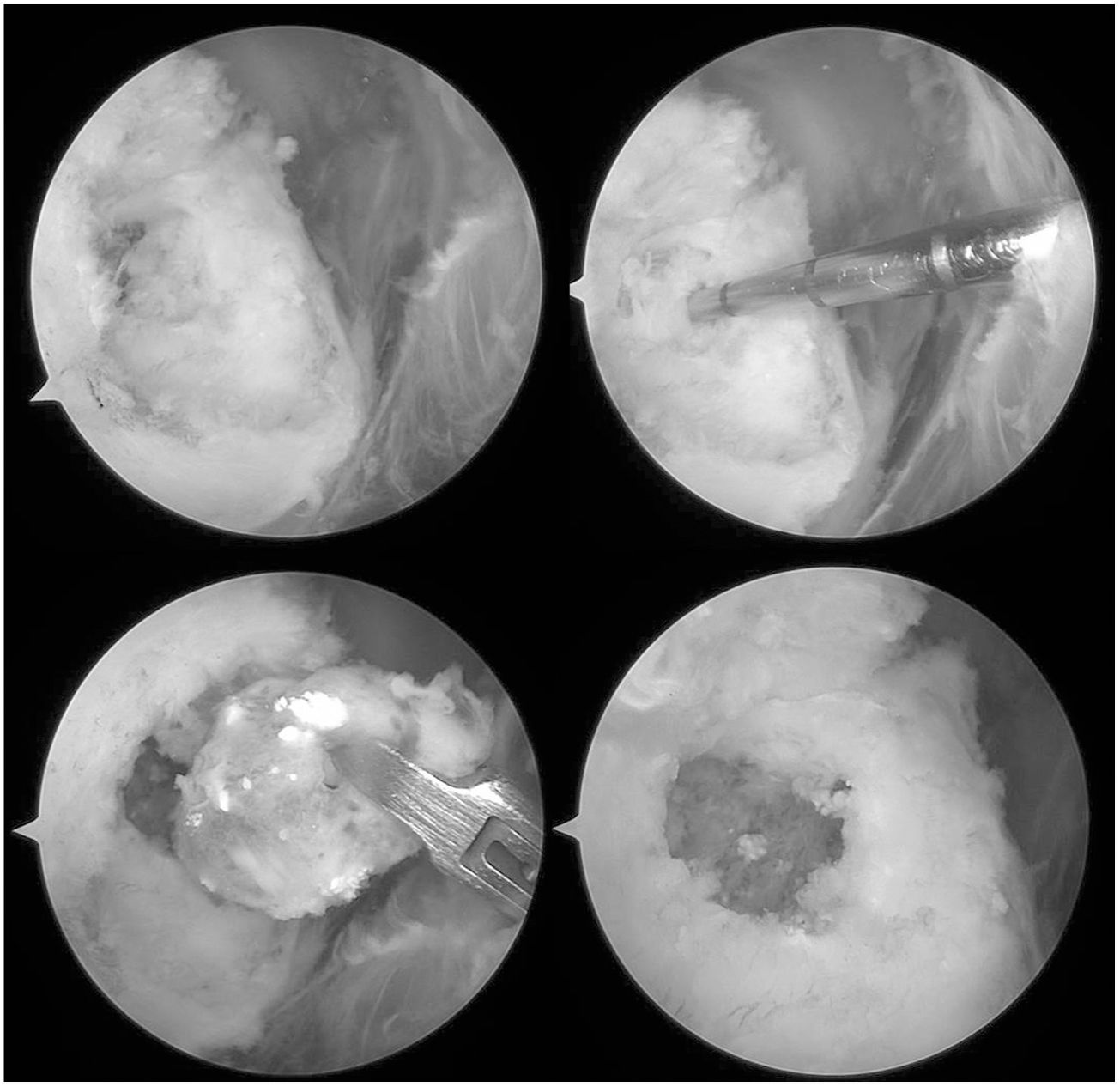
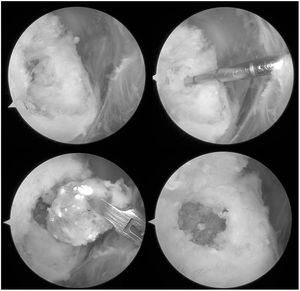
A shoulder arthroscopy was performed, finding calcific tendinitis of the supraspinitus. On debridement of the calcification, an extension of calcification within the greater tuberosity was observed. A single piece was removed in a sac of elastic tissue with calcium deposits from inside the greater tuberosity (Fig. 3); after debridement, a defect of approximately 1cm in diameter was observed with a healthy bone bed (Fig. 3). Finally a suture was placed to reinsert the supraspinatus in the greater tuberosity using a harpoon suture anchor, which was placed lateral to the intraosseous lesion, and 2 simple stitches. The pathological report confirmed the hypothesis of calcific tendinopathy with intraosseous extension: “Dense collagen tissue with calcifications and focal ossification. Compatible with calcific tendinitis”.
Arthroscopic images where the intraosseous expansion of the calcification can be observed once the intratendinous calcification has been debrided (upper right and upper left images). In the lower left image the removal of a single piece of the intraosseous material can be observed, which corresponds with an elastic tissue sac with calcic deposits. In the lower right image, the bone defect bed can be observed in the greater tuberosity once the lesion had been debrided.
The patient made good progress; the postoperative protocol for rotator cuff suture was followed. After 3 months, she returned to work (office). Six months following the operation she had full shoulder motion in all planes, full recovery of strength and a completely normal life with no discomfort. After one year of follow-up there has been no recurrence of the lesion.
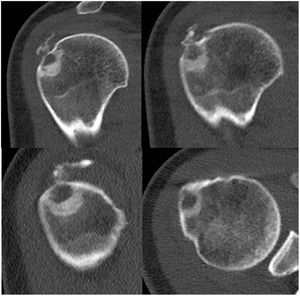
Clinical case 2A 50-year-old woman, consulting with a history over many years of pain in the right shoulder (dominant limb) and with a previous diagnosis of calcific tendinopathy of the shoulder. Prior to the consultation in our centre, she had been treated by means of 6 shock wave sessions (3–4 years earlier), ultrasound-guided needle aspiration (2 years earlier) and numerous physiotherapy sessions. On physical examination the patient had complete articular balance, both passive and active, but painful. She also had painful subacromial provocative tests and pain in the lateral face of the shoulder, the rest of the examination was normal. Plain X-ray showed a calcified nodular and sclerotic lesion at the level of the greater tuberosity that was eroding the cortex, and small calcifications in the subacromial space (Fig. 4). Calcifications were already present in previous studies of the patient, but the sclerotic lesion appeared after the latest treatments. Given the clinical suspicion of calcific tendinopathy of the shoulder, an MRI was requested (Fig. 4). A CT scan was performed to demarcate the extension and assess possible periosteal reaction (Fig. 5).
Plain X-ray of the shoulder, anteroposterior projection: a calcified nodular lesion and sclerosis can be observed at the level of the greater tuberosity eroding the cortex as well as small calcifications in the subacromial space (upper left image). MRI images: calcifications are confirmed in the tendon of the supraspinatus and a nodular lesion of 6mm in the greater tuberosity, hypointense in all the sequences, that is eroding the cortex and is associated with major surrounding bone oedema (upper right, lower left and lower right images).
A differential diagnosis was made between osteoid osteoma, osteoblastoma or possible aggressive calcific tendinopathy with intraosseous involvement. The ASA guideline was followed with no improvement, after reviewing the radiological follow-up and laboratory tests (normal), arthroscopic surgical treatment was considered with a diagnosis of suspected calcific tendinopathy of the shoulder with intraosseous extension.
A shoulder arthroscopy was performed, showing calcific tendinopathy of the supraspinatus. In the debridement of the calcification, extension of the calcification was observed inside the greater tuberosity. Bone debridement was carried out in the area of calcification with major resection of the calcic material. Finally, a suture was made for the reinsertion of the supraspinatus in the greater tuberosity using a harpoon suture anchor, which was placed lateral to the intraosseous lesion and 2 simple stitches.
The patient made favourable progress; the postoperative protocol for rotator cuff suture was followed. After 3 months, she subjectively presented significant improvement in pain compared to before the intervention, with a limitation of 10° in internal rotation and external rotation, antepulsion and abduction were complete. The patient returned to work and in more than 3 years, to our knowledge, there has been no relapse of the lesion.
DiscussionIn the presence of an osteolytic lesion in the greater tuberosity, a differential diagnosis should be considered with calcific tendinopathy of the shoulder with intraosseous extension. Intraosseous extension of calcific tendinopathy of the shoulder is a rare presentation, but described in the literature, although most are short series (Table 1).1,2,4,6–11 In the 2 cases described, doubt arose from the imaging tests as to a differential diagnosis with a tumour lesion, the first hypothesis being an osteoid osteoma; however, contrary to a diagnosis of osteoid osteoma, the pain was not typically nocturnal (it increased in supine decubitus, but not necessarily at night) nor did it subside with ASA. In case 1, the pain developed over a very short time, since in the rare cases where an intraosseous extension of calcific tendinopathy is observed, it usually occurs in longstanding recalcitrant tendinopathy as observed in case 2; in this regard, other studies have not found a relationship between the intraosseous extension of calcification and the evolution time of symptoms or the administration or otherwise of local injections.9 Both cases are women aged 49 and 50, which coincides with the most frequent presentation, which is in women between 40 and 60 years of age.2,9 In both cases we observed the characteristic radiological presentation of calcific tendinopathy with intraosseous extension, since we observed cortical erosion, osteolytic lesion and perilesional oedema in the spongy bone.4–7
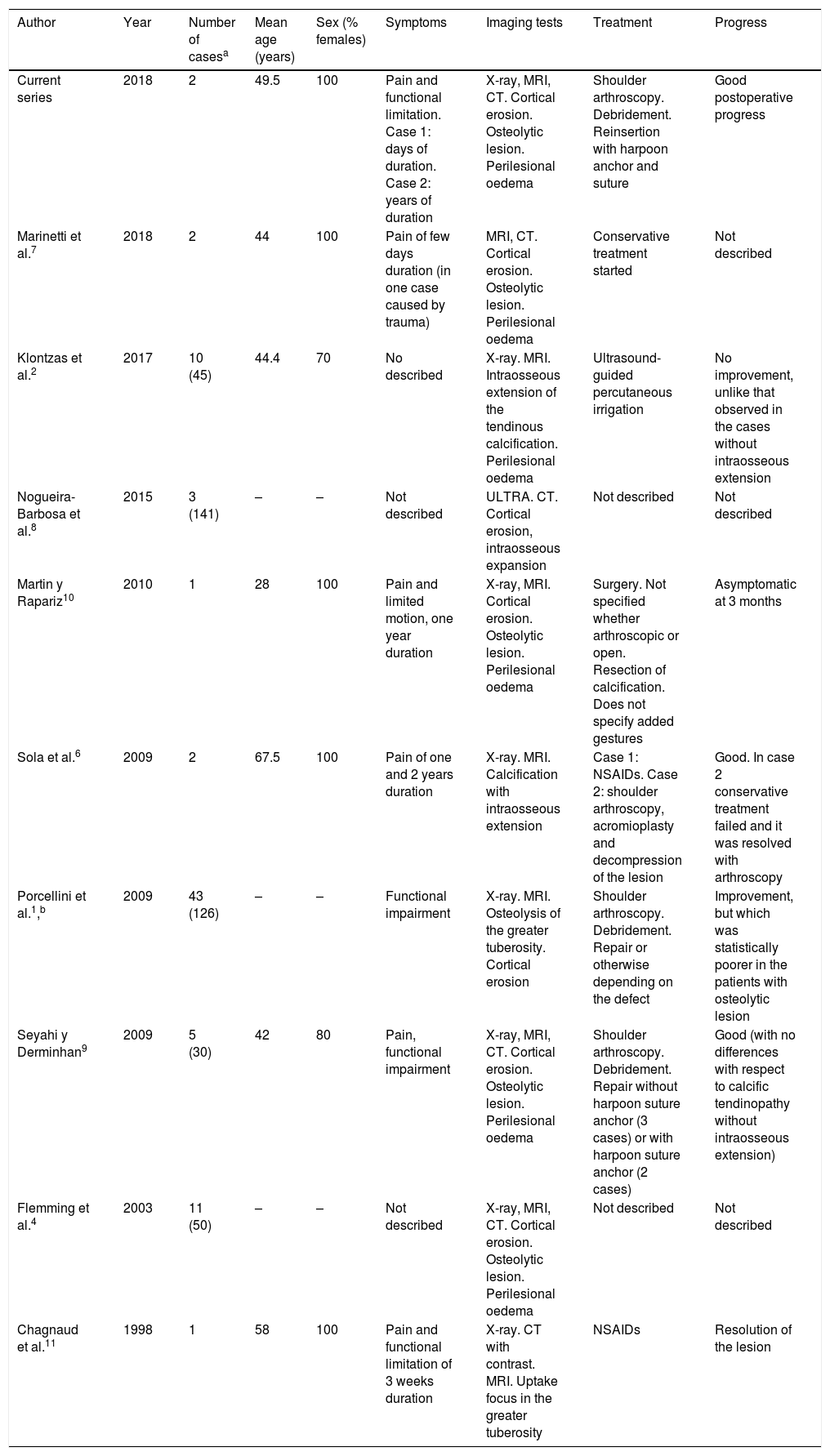
Cases of calcific tendinopathy of the shoulder with intraosseous expansion.
| Author | Year | Number of casesa | Mean age (years) | Sex (% females) | Symptoms | Imaging tests | Treatment | Progress |
|---|---|---|---|---|---|---|---|---|
| Current series | 2018 | 2 | 49.5 | 100 | Pain and functional limitation. Case 1: days of duration. Case 2: years of duration | X-ray, MRI, CT. Cortical erosion. Osteolytic lesion. Perilesional oedema | Shoulder arthroscopy. Debridement. Reinsertion with harpoon anchor and suture | Good postoperative progress |
| Marinetti et al.7 | 2018 | 2 | 44 | 100 | Pain of few days duration (in one case caused by trauma) | MRI, CT. Cortical erosion. Osteolytic lesion. Perilesional oedema | Conservative treatment started | Not described |
| Klontzas et al.2 | 2017 | 10 (45) | 44.4 | 70 | No described | X-ray. MRI. Intraosseous extension of the tendinous calcification. Perilesional oedema | Ultrasound- guided percutaneous irrigation | No improvement, unlike that observed in the cases without intraosseous extension |
| Nogueira-Barbosa et al.8 | 2015 | 3 (141) | – | – | Not described | ULTRA. CT. Cortical erosion, intraosseous expansion | Not described | Not described |
| Martin y Rapariz10 | 2010 | 1 | 28 | 100 | Pain and limited motion, one year duration | X-ray, MRI. Cortical erosion. Osteolytic lesion. Perilesional oedema | Surgery. Not specified whether arthroscopic or open. Resection of calcification. Does not specify added gestures | Asymptomatic at 3 months |
| Sola et al.6 | 2009 | 2 | 67.5 | 100 | Pain of one and 2 years duration | X-ray. MRI. Calcification with intraosseous extension | Case 1: NSAIDs. Case 2: shoulder arthroscopy, acromioplasty and decompression of the lesion | Good. In case 2 conservative treatment failed and it was resolved with arthroscopy |
| Porcellini et al.1,b | 2009 | 43 (126) | – | – | Functional impairment | X-ray. MRI. Osteolysis of the greater tuberosity. Cortical erosion | Shoulder arthroscopy. Debridement. Repair or otherwise depending on the defect | Improvement, but which was statistically poorer in the patients with osteolytic lesion |
| Seyahi y Derminhan9 | 2009 | 5 (30) | 42 | 80 | Pain, functional impairment | X-ray, MRI, CT. Cortical erosion. Osteolytic lesion. Perilesional oedema | Shoulder arthroscopy. Debridement. Repair without harpoon suture anchor (3 cases) or with harpoon suture anchor (2 cases) | Good (with no differences with respect to calcific tendinopathy without intraosseous extension) |
| Flemming et al.4 | 2003 | 11 (50) | – | – | Not described | X-ray, MRI, CT. Cortical erosion. Osteolytic lesion. Perilesional oedema | Not described | Not described |
| Chagnaud et al.11 | 1998 | 1 | 58 | 100 | Pain and functional limitation of 3 weeks duration | X-ray. CT with contrast. MRI. Uptake focus in the greater tuberosity | NSAIDs | Resolution of the lesion |
NSAIDs: non-steroidal anti-inflammatory drugs; ULTRA: ultrasound; MRI: magnetic resonance image; X-ray: plain X-ray; CT: computerised axial tomography.
The total number of subjects studied in the study is noted in brackets, which also includes lesions with another site or patients without intraosseous extension.
Porcellini et al.1 report osteolysis of the greater tuberosity, without specifying whether or not there is intraosseous expansion.
If there is a suspected differential diagnosis of a tumour lesion, before undertaking any invasive therapy, in the event of doubt and when a certain diagnosis has not been reached, the patient should be assessed by a unit specialising in musculoskeletal tumours. Once a tumour lesion has been ruled out and a diagnosis of calcific tendinopathy with intraosseous extension has been confirmed, treatment of the lesion should be considered. Although it has been described that conservative treatment with rest and non-steroidal anti-inflammatory drugs accompanied or otherwise by various rehabilitation techniques may be sufficient,1,4,6,11–13 in many cases symptoms do not subside. Although treatment with ultrasound-guided needle-aspiration may be effective for the treatment of calcific tendinopathy of the shoulder, it has been described that in cases with intraosseous extension of the lesion this technique loses efficacy,2 while shoulder arthroscopy provides an adequate approach to the lesion, with results similar to those obtained in the treatment of lesions without intraosseous extension.9 Debridement of the intratendinous calcification and aggressive debridement of the intraosseous lesion should be performed.1,9 If after debridement of the lesion there is a defect in the supraspinatus insertion, a suture should be made with reinsertion in the greater tuberosity according to the usual technique chosen according to the size and shape of the defect, just as good results having been shown with the arthroscopic debridement technique as in calcific tendinopathy without intraosseous extension,9 and in accordance with other authors, we consider that in cases with intraosseous expansion using an implant for reinsertion of the tendon in the greater tuberosity could be necessary.1 The 2 patients made good progress; in our experience, coinciding with Seyahi and Derminhan,9 their progress was as good as that of patients with no intraosseous extension, although other authors have described poorer outcomes when there is bone involvement.1
In conclusion, in the presence of an osteolytic lesion in the greater tuberosity of the humerus, a differential diagnosis with calcifying shoulder tendinitis with intraosseous extension should be considered in order to avoid invasive diagnostic procedures or unnecessary treatments. Once a diagnosis of calcific tendinopathy with intraosseous extension has been established, arthroscopic treatment is an effective option with outcomes comparable to those obtained in the treatment of calcific tendinopathy without intraosseous extension.
Level of evidenceLevel of evidence IV.
Conflict of interestsThe authors have no conflict of interests to declare.
*Please cite this article as: Miranda I, Sánchez-Alepuz E, Díaz-Martínez JV, Collado-Sánchez A, Peregrín-Nevado I. Tendinitis calcificante de hombro con extensión intraósea: experiencia con el tratamiento artroscópico y revisión de la literatura. Rev Esp Cir Ortop Traumatol. 2020;64:13–21.