Trigger finger (TF) is a frequent pathology depending on several factors. The objective of this study was to assess the relationship between multiple TF and systemic or musculoskeletal disorders in a sample of young patients.
Material and methodA retrospective study was performed of all patients with TF operated in our hospital between 2011 and 2015. Multiple or single TF diagnosis and pathologies such as diabetes mellitus (DM), thyroid dysfunction, carpal tunnel syndrome (CTS), epicondylalgia or DeQuervain's disease were collected. Statistical results included a bivariate analysis and a multiple logistic regression.
ResultsTwo hundred and seventy-nine patients with a mean age of 48.45years were included. The dominant hand was affected in 217 cases. There were 59 patients with multiple TF, 21 DM, 55 STC, 16 epicondylalgia and 14 DeQuervains. Prevalence of CTS was 19.7%, significantly higher than the general population (2%–4%). No statistical differences were found in age, sex, hypothyroidism, epicondylalgia or DeQuervain in the multiple TF group. Bivariate analysis detected that DM and CTS patients in the multiple TF group was significantly higher than in the single TF group (p=0.007, p<0.01). Multiple TF was also more frequent on the dominant side (p<0.01). Multivariate logistic regression confirmed these findings, showing a statistically significant association between the multiple TF group and DM (OR: 4.98, p<0.01), STC (OR: 2.09, p=0.037) and dominant side (OR: 3.76, p=0.016).
ConclusionsDiabetes, CTS and dominant side are independently associated with multiple TF in young patients.
El dedo en resorte (DR) es una patología frecuente de etiología multifactorial. El objetivo de este estudio fue valorar la relación entre la aparición de DR múltiple y patologías sistémicas o musculoesqueléticas en una muestra de pacientes jóvenes en edad laboral.
Material y métodoSe analizaron retrospectivamente todos los pacientes con DR intervenidos en nuestro hospital entre 2011 y 2015. Se recogió la existencia de DR múltiple o único y patologías como diabetes mellitus (DM), disfuncionalidad tiroidea, síndrome del túnel carpiano (STC), epicondilalgia o enfermedad de DeQuervain. Los resultados estadísticos incluyen un análisis bivariante y una regresión logística multivariante.
ResultadosSe incluyeron 279 pacientes, con una edad media de 48,45±9,01años. La mano dominante estuvo afectada en 217 casos. Hubo 59 pacientes con DR múltiple, 21 con DM, 55 STC, 16 epicondilalgia y 14 DeQuervain. La prevalencia de STC fue del 19,7%, significativamente superior a la media poblacional (2-4%). No se hallaron diferencias en cuanto a edad media, sexo, hipotiroidismo, epincondilitis o DeQuervain en DR único o múltiple. El análisis bivariante detectó que la proporción de DM (20,3%) y STC (32,2%) en el grupo de DR múltiple fue significativamente mayor que en el grupo de DR único (DM: 4,1%, p=0,007; STC: 16,4%, p<0,01). El DR múltiple también fue más frecuente en mano dominante (93,2%; p<0,01). La regresión logística multivariante confirmó los hallazgos, mostrando asociación estadísticamente significativa entre el grupo de DR múltiple y DM (OR: 4,98, p<0,01), STC (OR: 2,09, p=0,037) y la mano dominante (OR: 3,76, p=0,016).
ConclusionesLa DM, el STC y la mano dominante se relacionan de forma independiente con la aparición de DR múltiples en pacientes jóvenes en edad laboral.
The trigger finger (TF) is a common medical condition with multiple factors1–5 that, according to different studies, is related to diabetes mellitus (DM),6–10 carpal tunnel syndrome (CTS),11–21 and hypothyroidism.13,14 It has been found that the risk of TF appearing in diabetic patients increases proportionally with HBA1c levels,8 whereas in patients who suffer from CTS, the likelihood of TF is higher than in the healthy population, as well as after surgical exoneurolysis.9
However, no studies have been found that analyse exclusively the relation between the existence of multiple trigger fingers and these parameters, particularly as regards hand dominance and previous trauma in a sample of young people of working age.
The objective of this study was to appraise the relationship between the appearance of multiple TF, different systemic diseases, and potential precipitating factors, as well as with common diseases or syndromes of the musculoskeletal system in a sample of young patients of working age. Furthermore, this study compared the prevalence of the most common associated disease in our sample with those shown in the references.
Material and methodA cross-sectional cohort study was carried out by reviewing a sample of patients admitted to our hospital with a diagnosis of TF and who underwent surgery between the years 2011 and 2015.
Surgical treatment was indicated in cases that were refractory to conservative treatment when the symptoms prevented patients from conducting the normal activities of daily living.
Antibiotic prophylaxis was not necessary prior to the intervention. The surgical incision was longitudinal or transversal, depending upon the lead surgeon's preferences.
Subjects with an incomplete history or lost to follow up were excluded, as well as cases corresponding to revision surgeries.
The age and gender of the entire sample was recorded. Furthermore, the following variables were dichotomised: prior trauma of said finger, dominance of the hand involved, existence of multiple TF (two or more) or single TF, bilateral involvement, postoperative relapse, and the presence of diseases such as DM, hypo- and hyperthyroidism, CTS, epicondylalgia, DeQuervain syndrome or Dupuytren's contracture, and rheumatoid arthritis.
Theoretical population prevalences of DM, CTS, and hypothyroidism were obtained in our sample and compared based on the approximation obtained with normal (pz) and binomial distributions.
Statistical analysisFirst of all, a bivariate analysis was conducted of the pathologies and factors that are potentially related with the appearance of multiple TF. Student's t test was used for quantitative variables and the Pearson's chi-squared test (χ2) for categorical variables, applying Fisher's exact test when the frequency in a field was less than 5. Afterwards, a multivariate logistic regression analysis was performed, including multiple TF as the dependent variable and all those variables with statistically significant differences in the bivariate analysis as independent variables. Age and gender were considered potential confounding factors. p values of less than 0.05 (p<0.05) were deemed statistically significant. The software programme used for the process was the IBM SPSS, version 21.0.0.0.
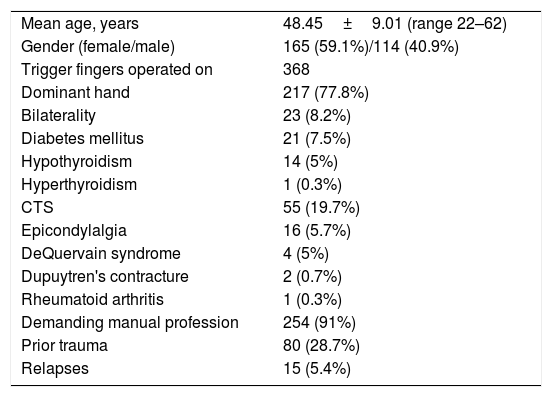
ResultsA total of 298 patients were detected with a diagnosis of TF who underwent surgery during the study period. Nineteen (19) cases were excluded due to incomplete histories and loss to follow up. Ultimately, 279 individuals (165 males and 114 females) were included with 368 trigger fingers and a mean age of 48.45±9.01 years. There were 21 cases of DM and 55 subjects suffered from CTS. In addition, 254 patients carried out demanding professional activities and 80 individuals reported having suffered a previous precipitating trauma. General data are summarised in Table 1.
General characteristics of the sample of patients with trigger finger who underwent surgery at our centre (n=298).
| Mean age, years | 48.45±9.01 (range 22–62) |
| Gender (female/male) | 165 (59.1%)/114 (40.9%) |
| Trigger fingers operated on | 368 |
| Dominant hand | 217 (77.8%) |
| Bilaterality | 23 (8.2%) |
| Diabetes mellitus | 21 (7.5%) |
| Hypothyroidism | 14 (5%) |
| Hyperthyroidism | 1 (0.3%) |
| CTS | 55 (19.7%) |
| Epicondylalgia | 16 (5.7%) |
| DeQuervain syndrome | 4 (5%) |
| Dupuytren's contracture | 2 (0.7%) |
| Rheumatoid arthritis | 1 (0.3%) |
| Demanding manual profession | 254 (91%) |
| Prior trauma | 80 (28.7%) |
| Relapses | 15 (5.4%) |
CTS: carpal tunnel syndrome.
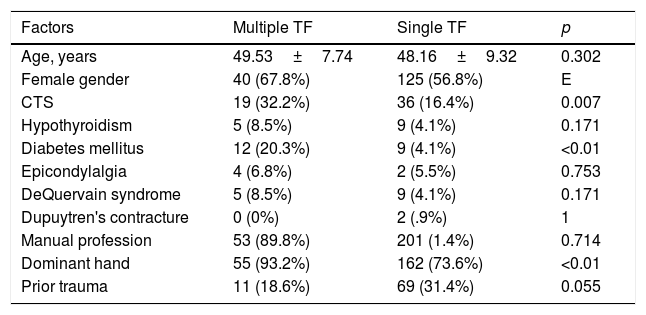
The mean age of the group of patients with multiple trigger fingers was 49.53±7.74 years, with a predominance of females (67.8%), compared to the group with a single trigger finger whose mean age was 48.16±9.32 years (56.8% women), with no significant differences being detected (p=0.302 and p=0.128, respectively). In the first group, the frequency of hypothyroidism (8.5%), epicondylalgia (6.8%), or DeQuervain syndrome (8.5%) did not differ significantly with the presence of these pathologies in the group with a single finger affected.
The prevalence of CTS and DM in patients with two or more trigger fingers was 32.2 and 20.3%, respectively, as opposed to 16.4 and 4.1% in the group with a single TF. These differences were statistically significant (CTS: p=0.007; DM: p<0.01). Moreover, the involvement of multiple fingers was also significantly related with the dominant hand in 93.2% of the cases (p<0.01) (Table 2).
Differences in demographic characteristics and potentially correlated factors among patients with one or multiple trigger fingers.
| Factors | Multiple TF | Single TF | p |
|---|---|---|---|
| Age, years | 49.53±7.74 | 48.16±9.32 | 0.302 |
| Female gender | 40 (67.8%) | 125 (56.8%) | E |
| CTS | 19 (32.2%) | 36 (16.4%) | 0.007 |
| Hypothyroidism | 5 (8.5%) | 9 (4.1%) | 0.171 |
| Diabetes mellitus | 12 (20.3%) | 9 (4.1%) | <0.01 |
| Epicondylalgia | 4 (6.8%) | 2 (5.5%) | 0.753 |
| DeQuervain syndrome | 5 (8.5%) | 9 (4.1%) | 0.171 |
| Dupuytren's contracture | 0 (0%) | 2 (.9%) | 1 |
| Manual profession | 53 (89.8%) | 201 (1.4%) | 0.714 |
| Dominant hand | 55 (93.2%) | 162 (73.6%) | <0.01 |
| Prior trauma | 11 (18.6%) | 69 (31.4%) | 0.055 |
TF: trigger finger; CTS: carpal tunnel syndrome.
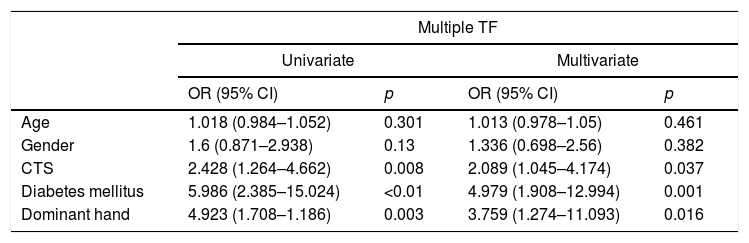
The multivariate analysis corroborated these findings, confirming that DM, CTS, and the dominant hand are significantly and independently related with the appearance of multiple TF; DM displayed the highest degree of association (OR: 4.979) (Table 3).
Multivariate logistic regression analysis of the potential factors of association and the existence of multiple trigger fingers.
| Multiple TF | ||||
|---|---|---|---|---|
| Univariate | Multivariate | |||
| OR (95% CI) | p | OR (95% CI) | p | |
| Age | 1.018 (0.984–1.052) | 0.301 | 1.013 (0.978–1.05) | 0.461 |
| Gender | 1.6 (0.871–2.938) | 0.13 | 1.336 (0.698–2.56) | 0.382 |
| CTS | 2.428 (1.264–4.662) | 0.008 | 2.089 (1.045–4.174) | 0.037 |
| Diabetes mellitus | 5.986 (2.385–15.024) | <0.01 | 4.979 (1.908–12.994) | 0.001 |
| Dominant hand | 4.923 (1.708–1.186) | 0.003 | 3.759 (1.274–11.093) | 0.016 |
TF: trigger finger; CTS: carpal tunnel syndrome.
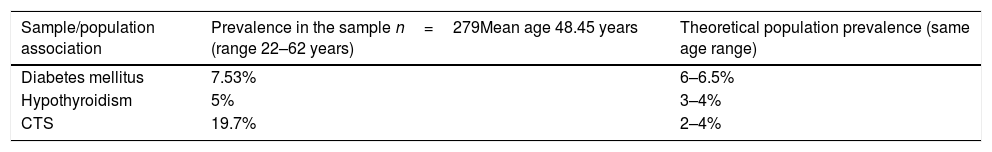
In contrast, this sample exhibited a 19.7% prevalence rate of CTS, which was significantly higher than the population mean in patients of the same age range (2–4%) (p<0.024); such was not the case with DM or hypothyroidism22 (Table 4).
Comparison of prevalences of diabetes mellitus, hypothyroidism, and carpal tunnel syndrome in the sample of patients with trigger finger and the theoretical population prevalences.
| Sample/population association | Prevalence in the sample n=279Mean age 48.45 years (range 22–62 years) | Theoretical population prevalence (same age range) |
|---|---|---|
| Diabetes mellitus | 7.53% | 6–6.5% |
| Hypothyroidism | 5% | 3–4% |
| CTS | 19.7% | 2–4% |
CTS: carpal tunnel syndrome.
Among the 279 patients recruited, 21% (59 patients) had multiple TF. Despite the fact that no differences were encountered between groups insofar as the existence of thyroid disease, epicondylalgia, and DeQuervain syndrome, among others, differences were discovered as regards the number of patients with DM, CTS, and involvement of the dominant hand, even after adjusting for the variables of age and gender as confounding factors. Likewise, it is worth noting that the prevalence of CTS (19.7%) in patients with TF was significantly higher than that of the population mean (2–4%), which can open new lines of research.
TF or stenosing tendinopathy of the finger is characterised by the feeling that the finger is stuck and may be accompanied by pain. It is a condition that is both highly prevalent and widely studied by authors such as Strom,10 who, in 1977, hypothesised that TF had an incidence rate of 28 cases per 100,000 person years. However, the bibliography that addresses its correlation with systemic illnesses or other musculoskeletal disorders is relatively scant, and the literature that does exist in this regard, reports on small, heterogeneous samples with disparate results.23
The association that is repeated most often in the literature is that of TF with DM and, specifically, with increased HbA1c levels.9 However, some, such as Grandizio et al.,21 while they failed to detect an association with HbA1c levels in a sample of patients who had undergone surgery for CTS, did identify a higher incidence of TF in the group of diabetic patients as compared to controls at 6 and 12months of follow up following surgery (3% in the control group and 8% in the DM group at 6months; 4% in the control group and 10% in the DM group at 12months). Authors, such as Pandey et al.,6 have reported TF as a common complication of DM, and is thought to share the same pathogenesis as cheiroarthropathy (a kind of limitation of joint mobility in diabetic patients). This concept has been endorsed by works such as the one by Yosipovitch et al.,8 who also related the duration of DM and TF (p<0.001), although they warn that said correlation was not identified for pharmacological control of DM. In our sample, we have not identified subjects who adequately controlled their DM and, although the proportion of patients with this disease was not very high (21 cases [7.5%]), we have found a statistically significant relation in the group of multiple TF compared to single TF (p=0.007), confirming its independent effect following multivariate logistic regression (p<0.01). In fact, of the variables included in the analysis, DM has been the one to exhibit the highest degree of association with multiple TF (OR: 4.98).
In contrast, the connection between TF and the incidence of CTS due to probable endocrine, metabolic, and even biomechanical disorders following release surgery has also been addressed.6,15–20 In this regard, Wessel et al.11 found a threefold increase in the risk of developing CTS in individuals treated for multiple TF, compared to patients diagnosed with a single TF. Others, such as Garti et al.,20 for instance, in an interesting study in which they analysed the latency of the median nerve in a sample of 62 patients with clinical signs of TF but without symptomatology of CTS, found that, indeed, 39 of them displayed an increased nerve impulse conduction time. In our study, while median nerve latency was not detailed, the proportion of patients with an associated clinical diagnosis of CTS was 19.7% (55 cases). It is difficult to compare this rate with the one published in the references, given that most studies assess the incidence of TF in CTS patient samples, unlike what we have done, which, in turn, confers greater relevance to our study. Furthermore, we have also found a significant, independent association with the multiple TF group, considering these two conditions to be related. It must be pointed out that surgical exoneurolysis of the median nerve in most cases does not guarantee that TF will be prevented, since, as some authors attest to, there is also a greater likelihood of developing said condition following surgery,16–18 which could imply that the existing correlation between these two disorders is due to more complex etiopathogenic mechanisms.
There are many works that subscribe to the theory that TF is more prevalent in the dominant hand.24,25 Nevertheless, authors such as Akhtar et al.26 qualify this by stating that the dominant hand is mostly affected in individuals with ages between 40 and 60 years, but in children under the age of 8 years, it can appear indiscriminately in either hand. Our results not only corroborate the theories presented, with greater involvement of the dominant hand (77.8%) in a group of patients with a mean age of 48 years, but, in addition, the dominant hand was observed to be significantly associated with the existence of multiple TF (93.2%; OR: 3.75; p=0.01).
Other publications also correlate the appearance of TF with disorders of the thyroid gland. Radu et al.,13 in an extensive review of the literature, revealed the relation between hypothyroidism and the appearance of different rheumatological disorders, including TF. For their part, Cakir et al.,14 in a sample of 137 patients with thyroid disease found that antiperoxidase antibody positivity was directly related with the appearance of TF (p=0.03). However, in our analysis, we have not found a statistically significant correlation between thyroid disorders and the prevalence of TF (p=0.17). Nonetheless, we must point out that we have only identified 14 cases of hypothyroidism and one case of hyperthyroidism, which can render the sample insufficient to draw definitive conclusions; despite our results, we still believe that these kinds of diseases may play a prominent role in the aetiology of TF.
The main disadvantage of the present work is its retrospective nature, with the limitations inherent in this type of study. Furthermore, the temporal relationship between the different conditions was not analysed; consequently, it is not known whether the disorders studied were previous, concomitant, or subsequent to the appearance of the TF. Among the strengths of this study, we include the large study sample, the fact that several diseases and syndromes were studied, as well as the inclusion solely of patients who underwent surgery decreases the possibility of incorrect diagnoses.27–30
Thanks to this work, a previously unreported relation has been found between multiple TF and certain conditions. The study of specific musculoskeletal syndromes or disorders and their association with TF helps us to delve deeper and gain greater insight into its epidemiology, considering that the information may be particularly useful for specialists and leaving the door open to new lines of research into the subject matter.
ConclusionsOur results suggest that the existence of DM, CTS, and dominant hand are independently related with the appearance of multiple TF in young patients of working age. Furthermore, the prevalence of CTS in individuals with TF is higher than that of the general population.
Level of evidenceLevel of evidence IV.
Ethical responsibilitiesProtection of human and animal subjectsThe authors state that, for the purposes of this research, no experiments have been carried out in people or in animals.
Confidentiality of dataThe authors state that they have abided by the protocols of their workplace as regards the publication of patient data.
Right to privacy and informed consentThe authors state that no patient data appear in this article.
FundingThis research has not received any specific grants from public or commercial sector agencies or from non-profit bodies.
Conflict of interestsThe authors have no conflict of interests to declare.
Please cite this article as: Berlanga-de-Mingo D, Lobo-Escolar L, López-Moreno I, Bosch-Aguilá M. Asociación entre dedos en resorte múltiples, enfermedades sistémicas y síndrome del túnel carpiano: análisis multivariante. Rev Esp Cir Ortop Traumatol. 2019;63:307–312.