To evaluate the results of arthroscopic reconstruction for the treatment of unstable scaphoid non-union with cancellous bone autograft.
Methods13 patients were treated with a mean age of 26 (18–45) years. The average time from injury until surgery was 14 (6–48) months. Preoperative and postoperative clinical and radiological parameters were evaluated. Mean follow-up was 16.8 (12–36) months.
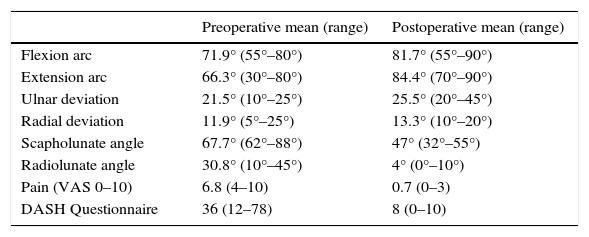
ResultsConsolidation was achieved in all cases at 7 (4–10 weeks), no patient had complications or reoperations. Range of motion, pain, functional assessment (DASH questionnaire) and radiological measurements improved compared to preoperative measurements. The average range of flexion improved: flexion 71.9° (55°–80°) to 81.7° (55°–90°), extension 66.3° (30°–80°) to 84.4° (70°–90°), ulnar deviation 21.5 (10°–25°) to 25.5° (20°–45°) and radial deviation 11.9° (5°–25°) to 13.3° (10th–20th). Pain (VAS 0–10) improved from 6.8 (4–10) to 0.7 (0–3). DASH functional scale improved from 36 (12–78) to 8 (0–10).
The Scapho-Lunate Angle improved from 67.7° (62°–88°) to 47° (32°–55°), and the Radio-Lunate Angle improved from 30.8° (10°–45°) to 4(0°–10°).
ConclusionTreatment of unstable scaphoid non-union with cancellous bone graft assisted by arthroscopy presents good clinical results with a short period of consolidation and recovery.
Evaluar los resultados de la reconstrucción artroscópica para el tratamiento de la seudoartrosis de escafoides inestable con autoinjerto de hueso esponjoso.
MétodoSe trató a 13 pacientes con una edad media de 26 (18-45) años. El tiempo medio desde la fractura hasta la intervención fue de 14 (6-48) meses. Se evaluaron parámetros clínicos y radiológicos preoperatorios y postoperatorios. El seguimiento medio fue de 16,8 (12-36) meses.
ResultadosLa consolidación se obtuvo en todos los casos a las 7 (4-10 semanas), ningún paciente presentó complicaciones ni precisó nuevas reintervenciones. El arco de movilidad, la dolor, la valoración funcional (cuestionario DASH) y las mediciones radiológicas mejoraron respecto al preoperatorio. El rango de movimiento promedio de flexión mejoró de 71,9° (55°-80°) a 81,7° (55°-90°), extensión de 66,3° (30°-80°) a 84,4° (70°-90°), desviación ulnar 21,5° (10°-25°) a 25,5° (20°-45°) y desviación radial 11,9° (5°-25°) a 13,3° (10°-20°). El dolor (EVA 0-10) mejoró de 6,8 (4-10) a 0,7 (0-3). Y la escala funcional DASH mejoró de 36 (12-78) a 8 (0-10).
El ángulo escafolunar mejoró de 67,7° (62°-88°) a 47° (32°-55°) y el ángulo radiolunar mejoró de 30,8° (10°-45°) a 4° (0°-10°).
ConclusiónEl tratamiento de seudoartrosis de escafoides inestables con injerto esponjoso asistido por artroscopia presenta buenos resultados clínicos, con un corto tiempo de consolidación y recuperación.
The lack of unstable scaphoid non-union is a common cause of posttraumatic arthrosis at the wrist level, and results in an advanced collapse of the carpus or, as it is also called, a SNAC (scaphoid non-union advanced collapse) wrist.1
To prevent this degenerative pattern, scaphoid pseudarthrosis must be treated using debridement, bone graft and stable internal fixation. Depending on the type of lack of consolidation, the bone supply varies: cancellous for stable injuries with minimal deformity,2 wedge-shaped corticocancellous for unstable injuries with humpback deformity,3,4 and vascularised bone graft for proximal pole ischaemic injuries.5–9 These techniques make it possible to correct the deformity at the expense of increased morbidity; this is because the approach required damages ligamentous structures and capsule, apart from the injuring vascular and proprioceptive microstructures of the carpus.
Several studies have proven the advantages of arthroscopy as a minimally-invasive procedure for the treatment of fractures and lack of scaphoid consolidation.10–13 It has lower morbidity, makes it possible to treat associated injuries, and causes less joint rigidity, which increases the functional results. In addition, it preserves the essential ligaments and the joint capsule, maintaining the proprioceptive functions of the wrist and normal carpal kinematics.
Arthroscopy is indicated in nonunions in the initial stage, stable or fibrous. However, it is limited in reconstructing unstable injuries with interspersed dorsal defects or the presence of the humpback deformity, when the standard treatment uses open tricortical bone grafts. Good results have recently been described in unstable scaphoid nonunion treated without open structural grafts. Cohen et al.14 presented the results of treating scaphoid pseudarthrosis with carpal collapse using open cancellous graft; in 12 patients, they obtained 100% consolidation with a mean follow-up of 2 years.
Simultaneous use of both techniques, non-structural graft and arthroscopic surgery, has only been mentioned superficially in recently published article.12
The objective of this article is to present our experience in the treatment of pseudarthrosis of the carpal scaphoid with humpback deformity using the combination of both techniques: placement of cancellous graft assisted by arthroscopy and stable percutaneous fixation.
Materials and methodsPatientsThis is a retrospective study of a series of patients diagnosed with unstable scaphoid pseudarthrosis treated using arthroscopy-assisted reconstruction. Criteria for inclusion were nonunion with sclerosis,1 cystic change and/or displacement greater than 2mm2; radiolunate angle (RLA) greater than 10°3; scapholunate angle (SLA) greater than 60° in simple radiological views4 and a minimum of 6 months since the initial trauma. Criteria for exclusion were less than 6 months of evolution since the trauma, stable fibrous consolidation, degenerative changes in the radiocarpal joint and ischaemic injuries and/or injuries compatible with avascular necrosis of the proximal pole of the scaphoid.
The same surgeon (PJD) operated on all the cases, after informed patient consent was given.
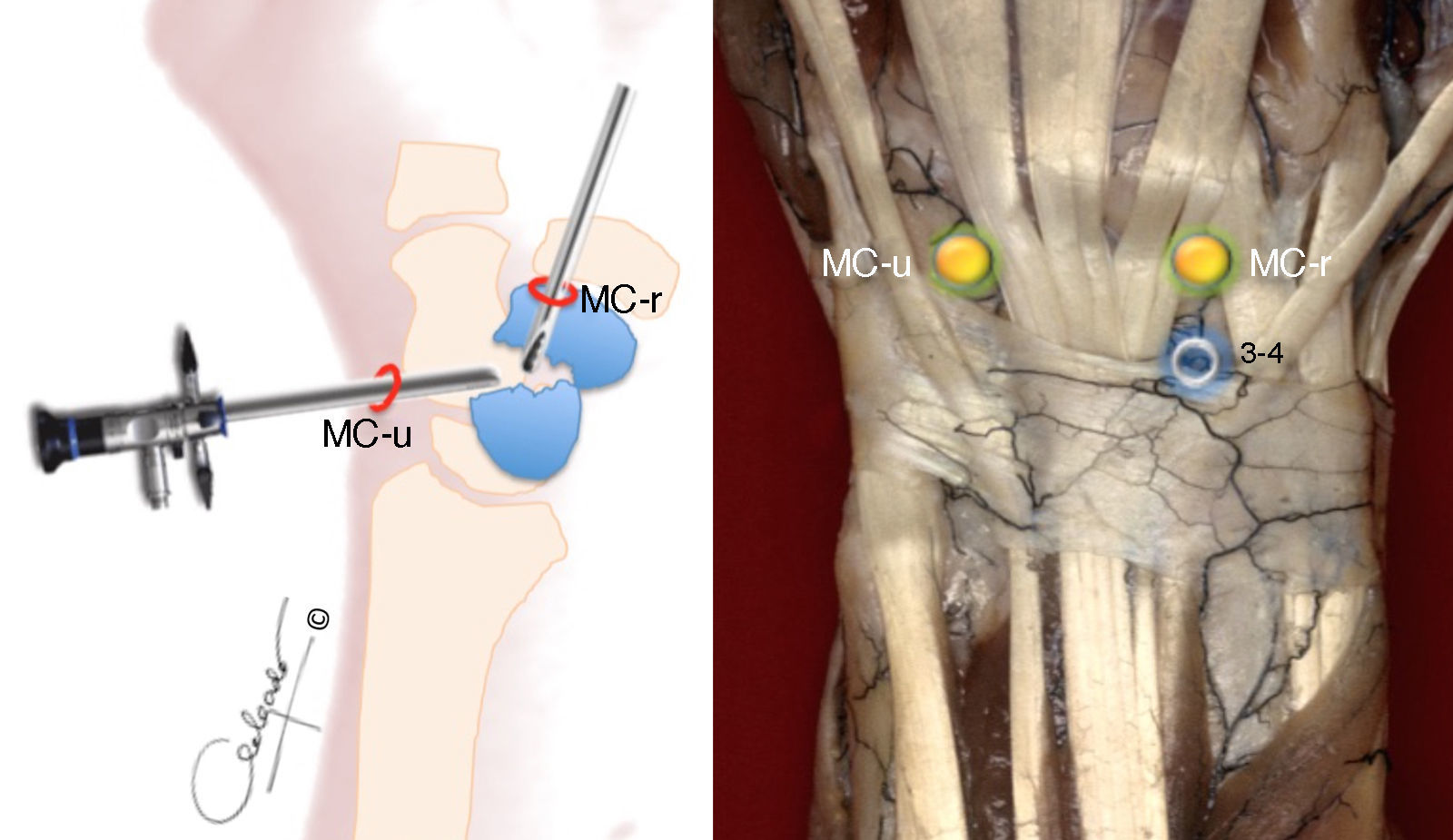
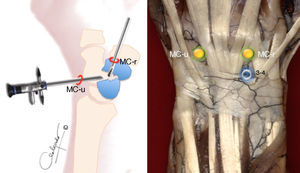
Surgical techniqueWrist arthroscopy was performed under general anaesthesia, with preventative ischaemia in the arm and cenital axial traction table (TractionTower ConMed Linvatec®, New York, USA) with 4.5kg of traction on the 2nd–5th fingers. Dry arthroscopy15 and the standard radiocarpal and midcarpal portals were used in all the cases (Fig. 1).
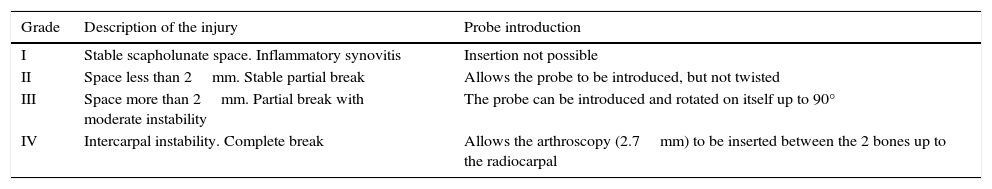
The first step was inspecting the radio- and midcarpal joints, assessing the state of the joint cartilage, intrinsic ligaments and triangular fibrocartilage complex. The scapholunate ligament was evaluated using the classification described by Geissler et al.16 (Table 1).
Arthroscopic scapholunate ligament injury classification by Geissler et al.
| Grade | Description of the injury | Probe introduction |
|---|---|---|
| I | Stable scapholunate space. Inflammatory synovitis | Insertion not possible |
| II | Space less than 2mm. Stable partial break | Allows the probe to be introduced, but not twisted |
| III | Space more than 2mm. Partial break with moderate instability | The probe can be introduced and rotated on itself up to 90° |
| IV | Intercarpal instability. Complete break | Allows the arthroscopy (2.7mm) to be inserted between the 2 bones up to the radiocarpal |
Taken from Geissler et al.16
The focus of pseudarthrosis was initially debrided with a fine 3-mm wide periostome, followed by a 2.7-mm bit, and completed with a spoon of 2–3mm to resect all the fibrous and devitalised tissue down to healthy bone. This manoeuvre was performed placing the optics in the ulnar midcarpal (MC-u) portal and the working tools through the radial midcarpal (MC-r) portal.
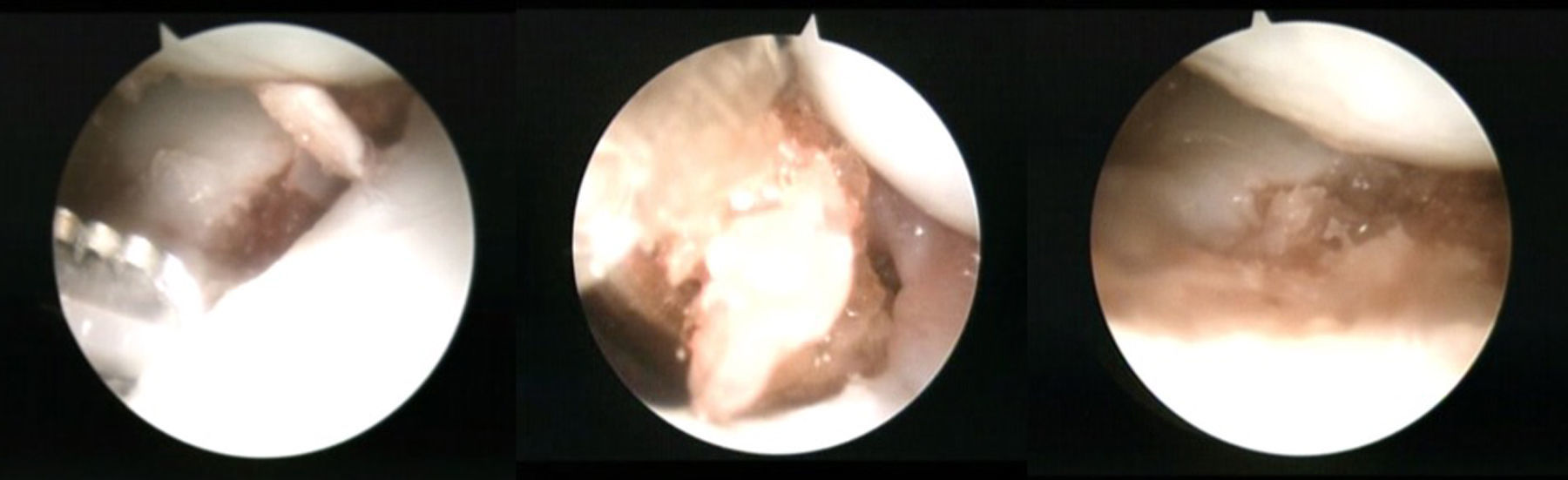
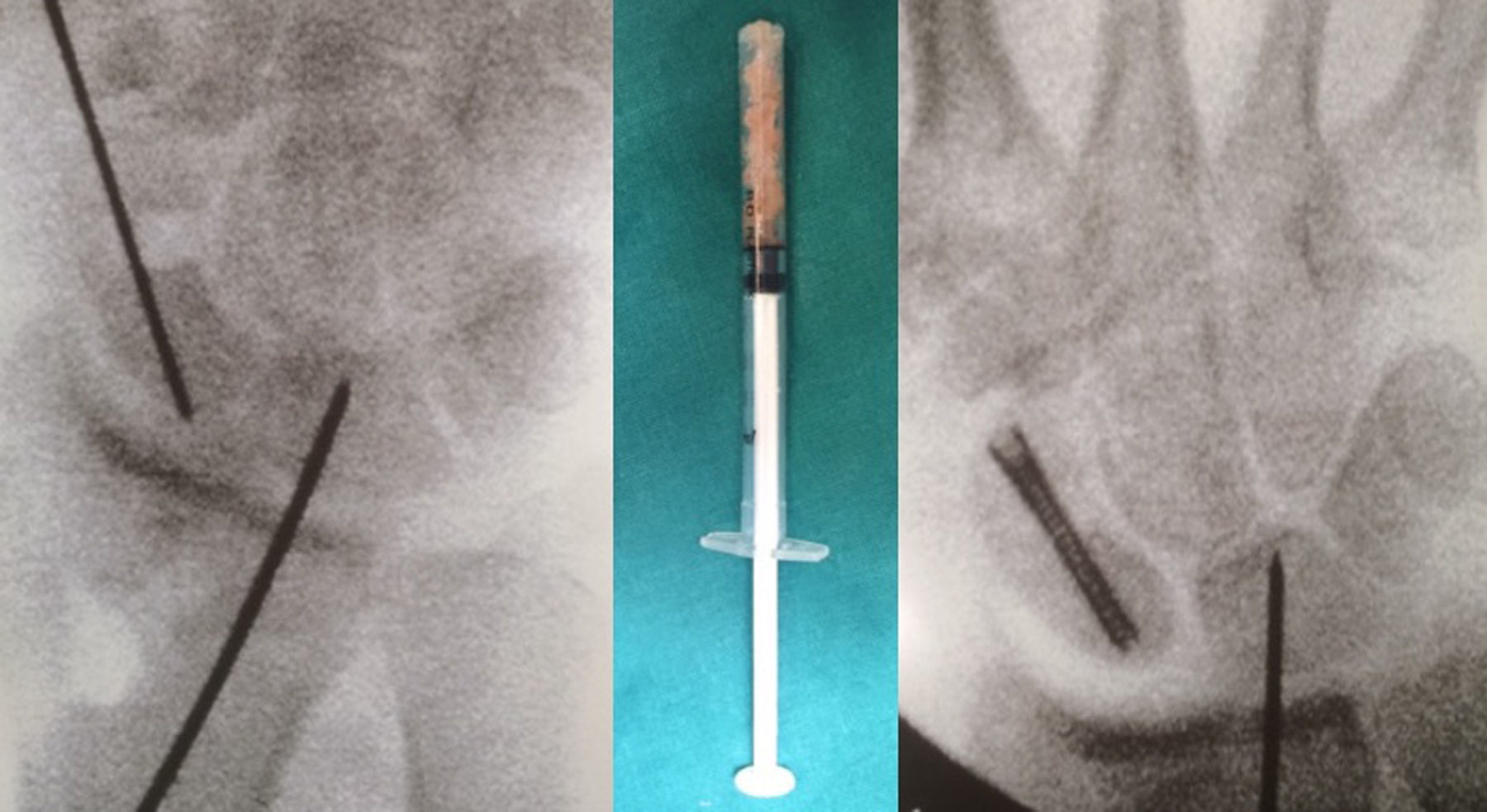
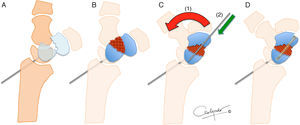
Next, the dorsal scapholunate deformity of dorsal intercalated segment instability (DISI) was reduced and fixed with a percutaneous 1.4-mm Kirschner wire from the radial to the scapholunate. In this way, the proximal pole was reduced to its natural location. Then, before reducing the distal pole, the cancellous bone graft was introduced through the MC-r portal, from the iliac crest or the bottom of the radial extensor 3rd compartment. To facilitate its placement, it was introduced through the body of an insulin syringe cut at the distal end. (The MC-r portal should be widened a few millimetres so the syringe can be introduced more easily.) With the help of the blunt trocar of the arthroscopy cannula, the graft is pushed and deposited where the nonunion exists. It is then impacted with the help of a spoon or the small dissector used previously, using its most curved part (Fig. 2).
Arthroscopically-assisted scaphoid reconstruction technique. After drilling the borders, the scapholunate is attached to the radiolunate to reduce the proximal pole (A). The graft is placed in the space created (B) and the wrist is reduced in maximum extension (C) to place the distal pole in its most anatomic situation (1) and provide length. It is fixed in placed with a 1.2-mm Kirschner wire (2) and both segments are fixed with the graft using headless cannulated screw (D).
The arthroscope was then removed and the fingers released from traction, leaving the wrist free. The wrist is placed palm up, forcing the maximum extension. This manoeuvre reduced the distal pole and gained bone length. Next, both segments are fixated with a 1.2-mm wire, the alignment is verified using fluoroscopy and the fixation was carried out using a headless cannulated screw, as in a conventional distal percutaneous fixation (Fig. 3). Internal fixation was with either an Acutrak Mini screw (Acumed, Hillsbrorough, Oregon, USA) (62% of the cases) or HCS (DePuy Synthes®, Johnson & Johnson, Oberdorf, Switzerland) (in 38%).
In the postoperative period, the wrist was immobilised with free-thumb volar splint for 2 weeks, which was changed to a removable one for 2–4 weeks, followed by physiotherapy. The percutaneous wire fixation of the radial to the scapholunate was removed at 4 weeks.
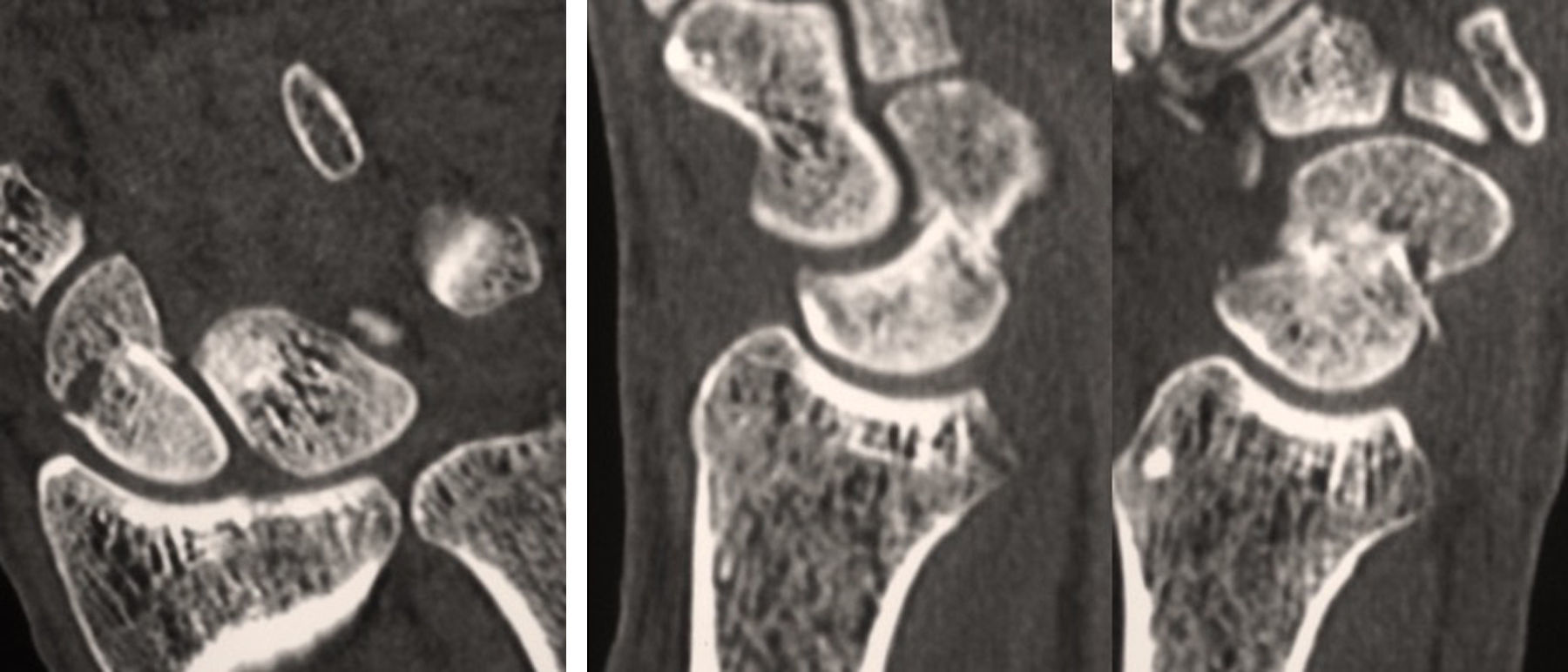
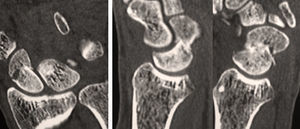
Clinical and radiological evaluationPreoperative radiological evaluation consisted of 4 scaphoid radiological views, as well as computed tomography (CT) and magnetic resonance scans, to assess the vascular state of the fragments. In the postoperative period, radiological studies in lateral, posteroanterior and oblique views in 45° wrist pronation were carried out every 2 weeks until consolidation. No study with CT scans were routinely carried out, except in cases with uncertain consolidation.
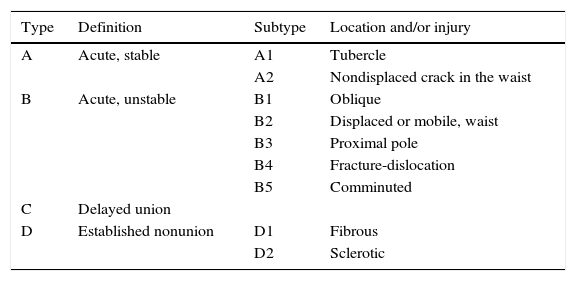
The Herbert and Fisher17 classification (Table 2) of scaphoid fractures and the classification suggested later by Herbert18 for nonunions (Table 3) were used to establish pseudarthrosis type and location. The radiological angles used were the scapholunate (SLA) and the radiolunate (RLA). The images used the measurement tools of viewer of the PACS (Picture Archiving and Communication System®, TerchHeim, Seoul, Republic of Korea),19 which incorporates a system of computerised case histories of the entity.
Classification of scaphoid fractures by Herbert and Fisher.
| Type | Definition | Subtype | Location and/or injury |
|---|---|---|---|
| A | Acute, stable | A1 | Tubercle |
| A2 | Nondisplaced crack in the waist | ||
| B | Acute, unstable | B1 | Oblique |
| B2 | Displaced or mobile, waist | ||
| B3 | Proximal pole | ||
| B4 | Fracture-dislocation | ||
| B5 | Comminuted | ||
| C | Delayed union | ||
| D | Established nonunion | D1 | Fibrous |
| D2 | Sclerotic |
Taken from Herbert and Fisher.17
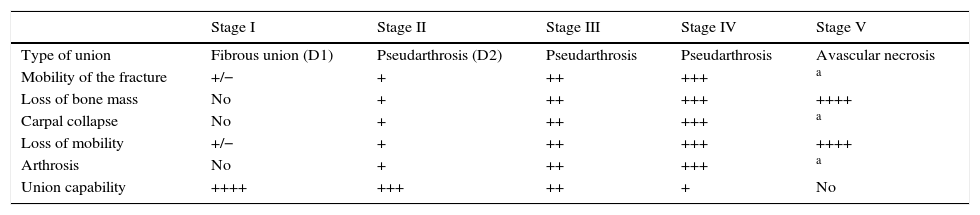
Stages of scaphoid nonunion according to Herbert.
| Stage I | Stage II | Stage III | Stage IV | Stage V | |
|---|---|---|---|---|---|
| Type of union | Fibrous union (D1) | Pseudarthrosis (D2) | Pseudarthrosis | Pseudarthrosis | Avascular necrosis |
| Mobility of the fracture | +/− | + | ++ | +++ | a |
| Loss of bone mass | No | + | ++ | +++ | ++++ |
| Carpal collapse | No | + | ++ | +++ | a |
| Loss of mobility | +/− | + | ++ | +++ | ++++ |
| Arthrosis | No | + | ++ | +++ | a |
| Union capability | ++++ | +++ | ++ | + | No |
Taken from Herbert.18
The arc of movement or mobility was evaluated with a standard goniometer and function was assessed with the Disabilities of the Arm, Shoulder and Hand (DASH) questionnaire validated for Spanish population.20 These evaluations were performed in the preoperative period, at 3 months following surgery and at the end of follow-up.
Bone consolidation was established when the patient felt no pain in the anatomical snuffbox and bone continuation or osseous bridge was seen between the two ends of the pseudarthrosis in all the X-ray views or in at least 2 CT scan images evaluated by 2 observers.21,22
ResultsThirteen patients (11 males and 2 females) were operated on using this technique. Mean age was 26 (18–45) years and 76% of the patients performed high-demand sport activities or work. Mean time from fracture to operation was 14 (6–48) months.
As for fracture pattern, all were Type D2 in the Herbert and Fisher classification. With respect to nonunion type, 76% were Stage ii and 24% were Stage iii in the classification proposed by Herbert. During the arthroscopy, 2 cases of scapholunate ligament injury were found: 1 case of Grade i and 1 of Grade ii in the classification by Geissler et al.16 In the radiological evaluation before surgery, 76% of the patients presented humpback deformity.
Consolidation was obtained in all cases at 7 (4–10) weeks. There were no complications or reoperations (Figs. 4–6).
Mean follow-up was 16.8 (12–36) months. The arc of movement, pain and functional assessment (DASH questionnaire) and radiological measurements all improved compared with preoperative status (Table 4).
Clinical and radiological results after arthroscopic reconstruction in chronic unstable scaphoid nonunion (13 patients).
| Preoperative mean (range) | Postoperative mean (range) | |
|---|---|---|
| Flexion arc | 71.9° (55°–80°) | 81.7° (55°–90°) |
| Extension arc | 66.3° (30°–80°) | 84.4° (70°–90°) |
| Ulnar deviation | 21.5° (10°–25°) | 25.5° (20°–45°) |
| Radial deviation | 11.9° (5°–25°) | 13.3° (10°–20°) |
| Scapholunate angle | 67.7° (62°–88°) | 47° (32°–55°) |
| Radiolunate angle | 30.8° (10°–45°) | 4° (0°–10°) |
| Pain (VAS 0–10) | 6.8 (4–10) | 0.7 (0–3) |
| DASH Questionnaire | 36 (12–78) | 8 (0–10) |
DASH, disabilities of the arm, shoulder and hand; VAS, visual analogue scale.
The degenerative pattern of the SNAC wrist evolves over 3 phases: (1) degenerative changes between the radial styloid and the distal scaphoid pole; (2) progressive involvement towards the joint between the scaphoid and the capitate bones, and (3) involvement of the joint between the semilunar and capitate bones, with due regard to the radio-semilunar joint. Pseudarthroses of the proximal and middle thirds show the first degenerative changes at the level of the radio-scaphoid joint, while these changes in the distal third are only seen in the space between the semilunar and capitate bones.23 The DISI instability gradually increases over time in the pseudarthroses of the distal pole and middle third, but those of the proximal pole rarely develop instability. Restoring the form of the scaphoid lessens the progression of the degenerative changes.
Wrist arthroscopy is a minimally-invasive technique that preserves vascularisation and proprioception in the carpal bones, but it is not free from risks.24 This is an especially important aspect, as the studies by Hagert et al. reflect.25 Wrist proprioception arises from the afferent signals provoked by the end sensory organs (mechanoreceptor) in ligaments and joint capsules that cause spinal reflexes for immediate joint stability. Scapholunate ligament proprioception in flexion, radial inclination and cubital movements has been shown to depend on the function of the posterior interosseous nerve, which can be injured with certain ease using the normal dorsal approaches.26,27
In chronic unstable pseudarthrosis, using corticocancellous grafts (whether vascularised or not) is the technique that offers the best guarantees to restore normal wrist anatomy and scaphoid consolidation. However, among the potential complications of open techniques are injuries to the stabilising and proprioceptive wrist elements, as well as graft protrusion, partial graft union, infections and problems with the osteosynthesis material. Another aspect to be considered is the time required to obtain complete union, which ranges from 12 to 19 weeks.6,28–30
There are several studies that describe good results applying cancellous bone grafts in unstable pseudarthrosis. Cohen et al.14 obtained full union in 12 patients treated with cancellous graft and cannulated screw fixation, with an excellent functional result at 2 years. Park et al.21 treated a total of 61 scaphoid pseudarthrosis cases (52% stable and 48% unstable) with cancellous grafts and Kirschner wire fixations. They obtained complete consolidation of the scaphoid bones in 88.2% of the stable pseudarthrosis cases and 83.9% of the unstable cases, with no statistically significant differences between the 2 groups.
Combining wrist arthroscopy with cancellous bone graft supply in unstable scaphoid pseudarthrosis is a demanding technique, but it provides the advantages of both techniques: it maintains proprioception and intrinsic vascularisation and, based on our results, could improve the consolidation obtained using structural grafts. In our experience, the short time until union is achieved (mean of 7 weeks) is notable; this is much lower than that presented in open series, whether using vascularised or non-vascularised grafts. Kim et al.,22 in their experience with arthroscopically-assisted treatment of scaphoid pseudarthrosis, treated 36 patients, of which 16 required cancellous grafts. They obtained complete consolidation in 86% of the cases at 11 weeks. This is the sole study similar to ours found in the literature.
One of the limitations of our work is that neither the final length or the final shape of the scaphoid bone has been measured. This could influence the radiological angles. A 9.3° correction of the intrascaphoid angle produces a 7.7° SLA correction.31 Nevertheless, these changes have not been shown to affect the final functional result. Jiranek et al.32 obtained a deformity of 45° or more in the intrascaphoid angle in 50% of their cases treated with trapezoidal-type corticocancellous grafts and found no influence on the final clinical result. In the series by Kim et al.,22 the radiological parameters of the scaphoid bone and wrist alignment in the cases in which full union was achieved did not correlate with changes in clinical wrist function. These authors concluded that, although the technique is limited for restoring normal carpal bone alignment, it does indeed present positive effects in the improvement of wrist function.
ConclusionsWrist arthroscopy is a valid alternative in the treatment of carpal scaphoid injuries. It yields good clinical results and consolidation results, even in cases of humpback deformities, with a shorter recovery time. The technique is probably limited to restoring the normal alignment of the carpus, but it is beneficial and improves the recovery times for these injuries. The results presented are comparable to other open techniques, but with lower associated morbidity. However, there is a need for longer series with greater follow-up and prospective comparative studies to confirm these results.
Level of evidenceLevel of evidence IV, therapeutic, case series.
Ethical disclosuresProtection of person and animalsThe authors declare that no experiments have been carried out on human beings or animals for the purpose of this research.
Confidentiality of dataThe authors declare that they have followed the protocols of their work centre about the publication of patient data.
Right to privacy and informed consentThe authors have obtained informed consent from the patients and/or subjects indicated in this article. This document is held by the corresponding author.
Conflict of interestsThe authors have no conflicts of interest to declare.
Please cite this article as: Delgado-Serrano PJ, Jiménez-Jiménez I, Nikolaev M, Figueredo-Ojeda FA, de Rozas-López MG. Reconstrucción artroscópica de la seudoartrosis inestable del escafoides carpiano. Rev Esp Cir Ortop Traumatol. 2017;61:216–223.