Ulnar variance may be a risk factor of developing scaphoid non-union.
MethodsA review was made of the posteroanterior wrist radiographs of 95 patients who were diagnosed of scaphoid fracture. All fractures with displacement less than 1mm treated conservatively were included. The ulnar variance was measured in all patients.
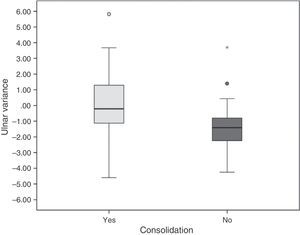
ResultsUlnar variance was measured in standard posteroanterior wrist radiographs of 95 patients. Eighteen patients (19%) developed scaphoid nonunion, with a mean value of ulnar variance of −1.34 (±0.85)mm (CI −2.25 to 0.41). Seventy seven patients (81%) healed correctly, and the mean value of ulnar variance was −0.04 (±1.85)mm (CI −0.46 to 0.38). A significant difference was observed in the distribution of ulnar variance (P<0.05). These results remained significant after adjusting for age, with an OR of 0.69 (CI 0.49 to 0.95).
The patients were categorized into two groups: ulnar variance less than −1mm, and ulnar variance greater than −1mm. It appears that patients with ulnar variance less than −1mm had an OR 4.58 (CI 1.51 to 13.89) with P<0.007.
DiscussionDesai et al. concluded that radiological features of acute scaphoid fractures cannot be used to predict the likelihood of fracture union. For this reason, the existence of other risk factors was analyzed.
According to the results of the present study, it can be concluded that patients with scaphoid fracture and ulnar variance less than −1mm have a greater risk of developing scaphoid nonunion, OR 4.58 (CI 1.51 to 13.89) with P<0.007.
Estudiar la varianza cubital como factor de riesgo en el desarrollo de seudoartrosis de escafoides.
Material y métodoAnalizamos retrospectivamente las radiografías posteroanterior de muñeca de 95 pacientes diagnosticados de fractura de escafoides. Incluimos todas las fracturas con un desplazamiento menor de 1mm tratadas de forma conservadora. Realizamos la medición de la varianza cubital en todos los pacientes.
ResultadosDieciocho pacientes (19%) desarrollaron seudoartrosis de escafoides, siendo el valor medio de la varianza cubital −1.34 (±1.85) mm (IC −2.25–0.41). Setenta y siete pacientes (81%) sanaron correctamente y su valor medio de varianza cubital fue −0.04 (±1.85) mm (IC −0.46–0.38). Se observaron diferencias significativas en la distribución de la varianza cubital (P<0.05). Este resultado se mantuvo significativo ajustando por edad, con una OR de 0.69 (IC 0,49–0,95).
Categorizamos los pacientes en 2 grupos: varianza cubital menor de −1mm y varianza cubital mayor de −1mm. Los pacientes con varianza cubital menor de −1mm presentaban una OR 4.58 (IC 1.51–1389) con P<0,007.
DiscusiónDesai et al. concluyeron que los hallazgos radiológicos en la fractura de escafoides no pueden predecir la probabilidad de unión de la fractura. Por esta razón, analizamos la existencia de otros factores de riesgo.
Según nuestros resultados, podemos concluir que los pacientes con fractura de escafoides y varianza cubital menor de −1mm tienen mayor riesgo de desarrollo de seudoartrosis de escafoides, OR 4.48 (IC 1.51–1389).
Scaphoid fractures account for between 70% and 80% of fractures affecting carpal bones in young, active patients.1,2 According to several published series, between 85% and 90% of these fractures heal with correct conservative treatment.1,3–6 However, between 10% and 15% of patients develop scaphoid non-union which may result in arthrosis, pain and functional limitation over time.3,5,7
In recent years different classifications of scaphoid fractures have been published. These classifications describe the location and configuration of the scaphoid fracture although, as noted by Compson et al., it is not easy to identify and locate the fracture plane.8 Furthermore, Desai et al.9 establish that none of them provide sufficient information regarding the consolidation rate, raising doubts about the reproducibility of these classifications.
This lack of reproducibility and the difficulty in interpreting radiological findings have led us to consider the importance of an alternative finding in simple radiology which could play a part in the detection of cases which could develop into a scaphoid non-union.
Negative ulnar variance appears to be connected to a greater frequency of scaphoid fracture due to an alteration of load distribution through the radius.10 However, despite biomechanical studies which show that the distribution of loads at radial-ulno-carpal level depend on ulnar variance, only 2 publications exist which study the relationship between this and the possibility of the development of scaphoid non-union, presenting major limitations when establishing differences between the different treatment groups.11,12
This objective of this study was therefore to evaluate the correlation of the ulnar variance with the risk of developing scaphoid non-union in scaphoid fractures and secondarily to assess the possible relationship with other radiological parameters.
Material and methodsWe carried out a retrospective analysis of all patients diagnosed with non displaced or minimally displaced scaphoid fractures (interfragmentary diastasis of <1mm) between 2002 and 2012, evaluating the initial radiological findings and comparing them with the development of the fracture either in consolidation or non-union.
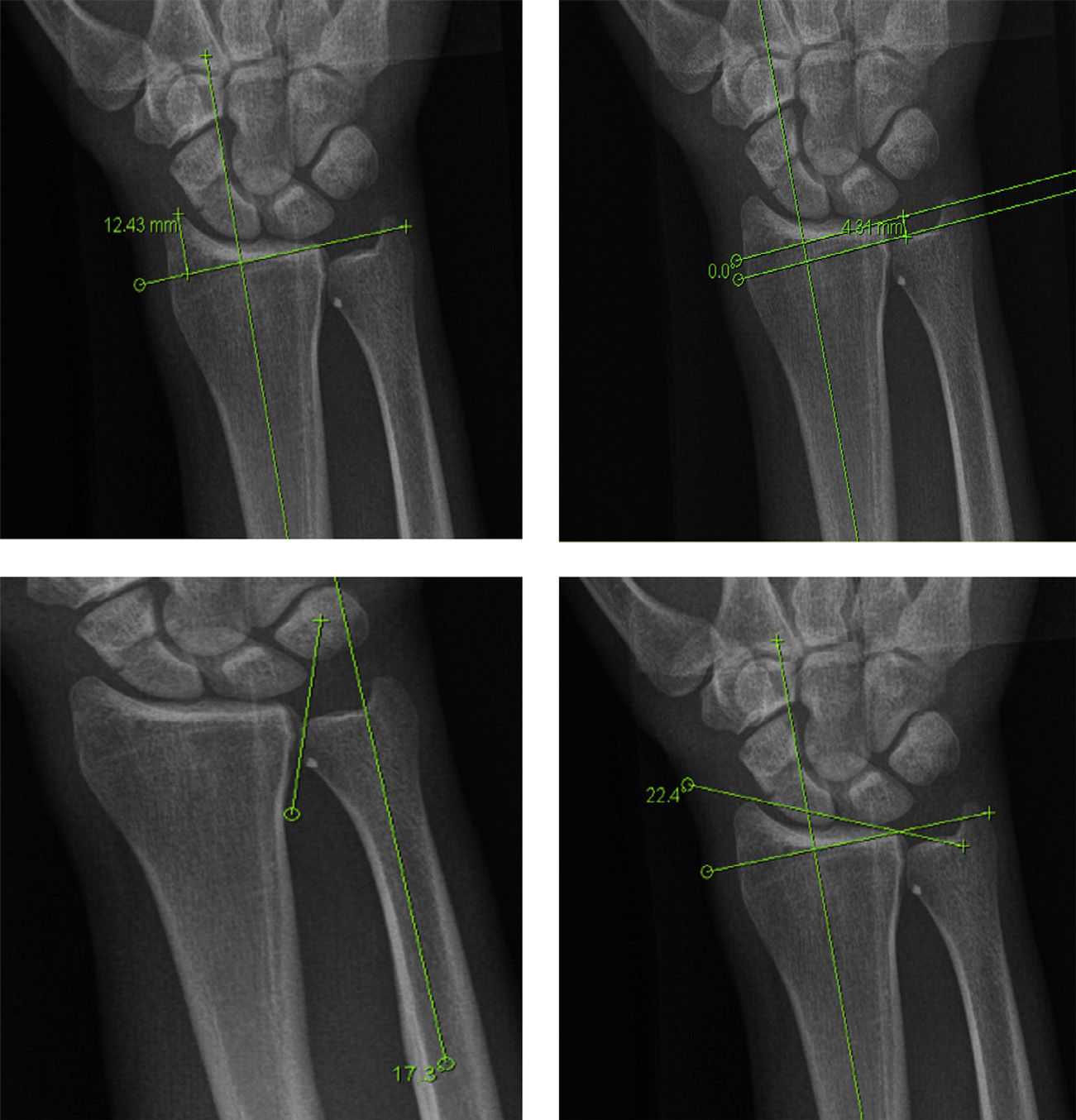
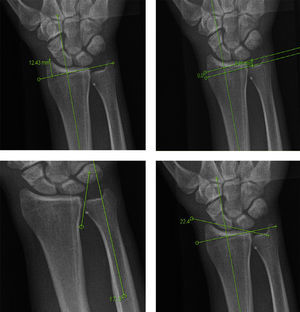
Inclusion criteria included those patients diagnosed with a stable middle-third scaphoid fracture, i.e. with displacement less than 1mm,13,14,20 treated conservatively with forearm plaster including the first finger, leaving the interphalangeal joint free,1,15 and with correct radiological follow-up until consolidation, non-union or delayed consolidation. In the latter case surgery was obligatory. Demographic analysis was performed on all patients and the radiological analysis of posteroanterior and lateral projections was performed at the time of fracture diagnosis, with particular attention being paid to the measurement of the ulnar variance as a possible prognostic factor16,17 (Fig. 1).
Patients were excluded if follow-up did not result in determining the consolidation or non-consolidation of the fracture. Also excluded were those patients with an associated distal radius or carpal bone fracture where surgical treatment was required, those where complementary radiological tests were of poor quality and the fracture and/or sequelae could not be classified.
The perpendicular method was used for measuring ulnar variance. Steyers and Blair compared 3 different methods for measuring ulnar variance and concluded that, although all 3 were highly trustworthy, the perpendicular method appears to be more precise in eliminating the interobserver and intraobserver error rate.16
Statistical analysis data are presented as mean and standard (SD) or numerical (%) deviation. Intergroup comparison and independent samples for continuous variables were analyzed using the Mann–Whitney t-test or U test and categorical variables were analyzed using the Chi-square test and the Fisher exact test. Statistical significance was considered at P<0.005. A binary logistic regression model was also used to determine the effect of the ulnar variance on consolidation, adjusted by potential confounding factors. The statistical program SPSS version 16.0 (SPSS Inc. Chicago, IL, USA) was used for this analysis.
Results167 patients diagnosed with scaphoid fracture (123 patients) or non-union (44 patients) were gathered between 2002 and 2012. By applying the previously-defined inclusion criteria, of the 123 patients diagnosed with scaphoid fracture in our center, 95 received conservative treatment. Out of the group with scaphoid fractures, 28 patients were excluded from this study. 13 of them had received surgery, 11 had not completed follow-up and 4 had invalid radiological tests. Of the patient group on whom surgery was performed, 7 had an associated radius fracture and the other 6 opted for surgery after being informed about the different treatments, their success rate, and the possible complications derived from each one.
The 95 patients included were distributed into 2 groups: group 1 comprised of 77 patients (81%) who developed consolidation of the fracture, group 2 comprised of 18 patients (19%) who developed non-union or delayed consolidation.
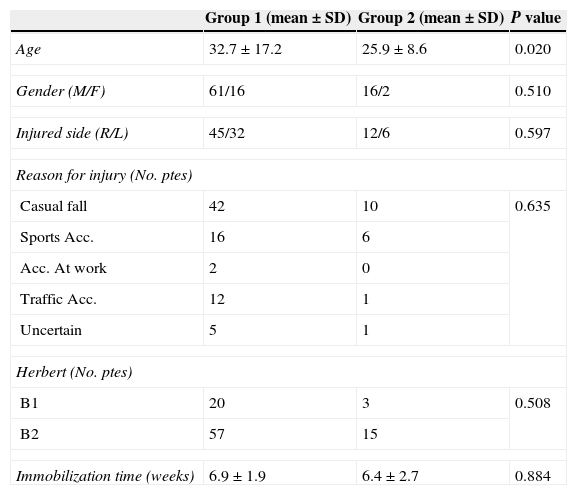
Table 1 shows the general characteristics of both groups. The mean age in group 1 was 32.7 (28.8–36.6), 61 men and 16 women. The mean age of group 2 was 25.9 (21.7–30.2), 16 men and 2 women.
Demographic data of the compared groups, expressed as mean±standard deviation (SD). Comparison of conservative treatment duration in both groups with no significant variations (P: 0.884).
| Group 1 (mean±SD) | Group 2 (mean±SD) | P value | |
|---|---|---|---|
| Age | 32.7±17.2 | 25.9±8.6 | 0.020 |
| Gender (M/F) | 61/16 | 16/2 | 0.510 |
| Injured side (R/L) | 45/32 | 12/6 | 0.597 |
| Reason for injury (No. ptes) | |||
| Casual fall | 42 | 10 | 0.635 |
| Sports Acc. | 16 | 6 | |
| Acc. At work | 2 | 0 | |
| Traffic Acc. | 12 | 1 | |
| Uncertain | 5 | 1 | |
| Herbert (No. ptes) | |||
| B1 | 20 | 3 | 0.508 |
| B2 | 57 | 15 | |
| Immobilization time (weeks) | 6.9±1.9 | 6.4±2.7 | 0.884 |
By applying Herbert's classification,18 group 1 presented 20 type B1 patients and 57 type B2; group 2 presented 3 patients with type B1 fracture and 15 patients with type B2 fracture. No significant differences were found between the two groups.
Immobilization time in group 1 was 6.9 (6.5–7.3) weeks, whilst in group 2 it was 6.4 (5.1–7.8) weeks, with no significant differences being found between the two groups (P>0.557).
Of the 18 patients in group 2, 12 underwent surgery once the scaphoid non-union was established (from 8 months onwards); one of the patients did not present for follow-up after non-union diagnosis and after being referred for surgery; another patient rejected surgery after non-union was established and after being referred for surgery; another patient rejected surgery after non-union had been established, for employment reasons and on finding themselves asymptomatic. The remaining 4 underwent surgery between 3 and 6 months following the initial trauma, and these 4 could be considered as patients with delayed consolidation.
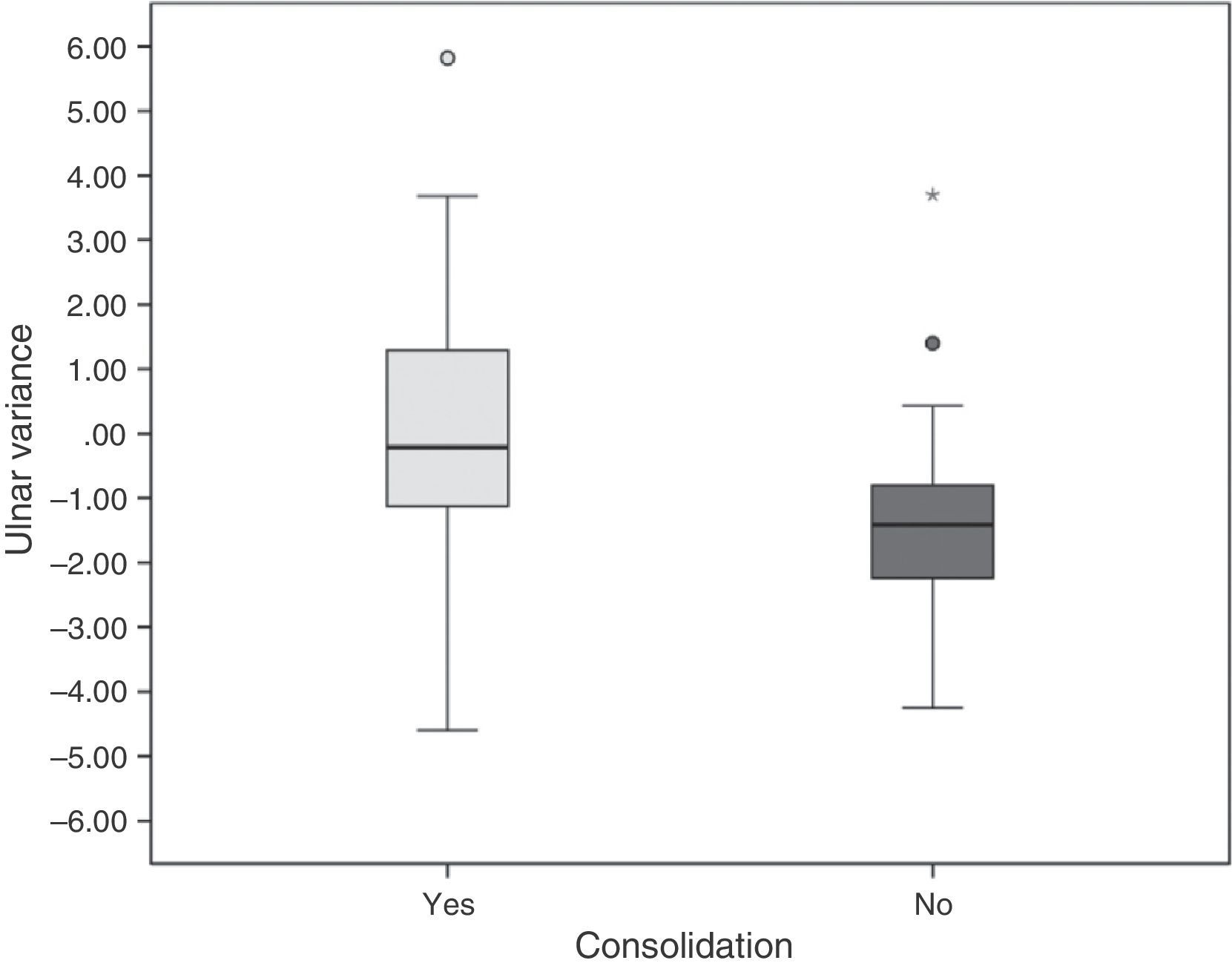
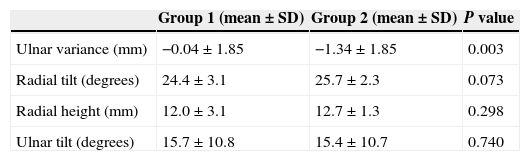
Table 2 shows the analysis of radiological findings obtained in evaluation of the initial radiograph after diagnosis of the fracture. The mean value of the ulnar variance in the 95 patients evaluated was 0.29mm with a SD of ±1.91 (CI −0.68 to 0.10). Group 1 presented a mean value of 0.04mm with an SD of ±1.85 (CI −0.46 to 0.38), whilst group 2 presented with a mean value of −1.34mm with a SD of ±1.85 (CI −2.25 to 0.41), significant differences being found between both groups (P<0.05) (Fig. 2). These results remained significant with an age-adjusted OR of 0.69 (CI 0.49–0.95).
Comparison of means and standard deviation (SD) of the radiological findings evaluated. Significant differences were observed between groups with regard to the ulnar variance (P: 0.003).
| Group 1 (mean±SD) | Group 2 (mean±SD) | P value | |
|---|---|---|---|
| Ulnar variance (mm) | −0.04±1.85 | −1.34±1.85 | 0.003 |
| Radial tilt (degrees) | 24.4±3.1 | 25.7±2.3 | 0.073 |
| Radial height (mm) | 12.0±3.1 | 12.7±1.3 | 0.298 |
| Ulnar tilt (degrees) | 15.7±10.8 | 15.4±10.7 | 0.740 |
Radiological evaluation was made of the radial tilt, radial height and ulnar tilt, as well as of the ulnar variance. Ulnar tilt was defined as the angle formed by the longitudinal axis of the ulnar and the joint surface of the ulnar with the radius, with no statistically significant differences being found between the 2 groups17,19 (Fig. 1).
On classifying the ulnar variance variable into 2 groups, less than −1mm and greater than −1mm, we observed that the patients with variance less than −1mm presented an odds ratio (OR) of 4.8 (CI 1.51–13.89) with P<0.007.
DiscussionClassical treatment of middle-third non-displaced scaphoid fractures consists of immobilization with plaster for 6–12 weeks, with a consolidation rate of 85–95%.2,15,20,21 The lack of consolidation of the fracture gives rise in little time to the degeneration of the radiocarpal and mediocarpal joint. This may lead to significant limitation and on occasions require other palliative long-term treatments.7
A systematic review of the evidence of non-displaced scaphoid fracture management assessed 8 randomized research studies, comparing conservative treatment with surgery. Two hundred and seven patients were treated with surgery and 212 received conservative treatment. The functional results were standardized and assessed in 247 patients included in 4 studies, with surgical treatment (P<0.01) being significantly endorsed. With regard to secondary parameters, the results were heterogeneous, favoring surgical treatment in terms of patient satisfaction, grip strength, consolidation time and sick leave. Conversely, there were no significant differences between the two treatments with regard to pain, range of movement, non-union rate and poor consolidation. The rate of complications was greater in the group who underwent surgery (23.7%) than the group treated conservatively (9.1%), although no statistically significant differences were found (P: .13). There was a higher rate of scaphoid-trapezium arthrosis in the group who underwent surgery (P: .05).22
Surgical treatment criteria for middle-third scaphoid fractures are currently: displacement greater than 1mm, an intrascaphoid angle greater than 35°, bone loss or communition and perilunar fracture-luxation. A relative criteria to be taken into consideration is the type of patient to be treated (manual worker, young person or athlete) and their preferences.2 Among the different criteria used to assess if significant differences exist between conservative and surgical treatment of scaphoid fractures, in none of the reviewed prospective studies is the intrascaphoid angle established as a surgical criterion.4,21 This is mainly due to the fact that the quantitative measurements of scaphoid deformity are of very limited inter and intraobserver reliability. We have therefore not used this in our work. In addition to the work published by Desai et al.9, Koh et al. studied the effect of the position of the wrist in measuring the different carpal indexes in lateral radiography, suggesting that any minimum alteration in the levels of flexion and extension of the wrist could alter the measurements made in the lateral radiograph.23
At present controversy remains as to which is the best therapeutic option for the patients with a non-displaced scaphoid fracture, which makes us question whether there may be other risk factors involved in the development of the scaphoid non-union.
A broad study has been made of the influence of ulnar variance in different wrist pathologies25 since Hulten established the terms of negative ulnar and positive ulnar in 1928, to describe the variations of length between the ulnar and radius in posteroanterior radiograph.24
Different publications have established that a relationship exists between Kienböck's26,27 disease, carpal instability,19,28,29 the ulnocarpal impaction syndrome,30–32 and scapholunate ligament tears.33,34
Furthermore, biomechanical studies have demonstrated that the distribution of physiological loads through the wrist is approximately 80% through the radius and 20% through the ulnar.35 This load distribution is subject to variations depending on the ulnar variance. A shortening of the ulnar by 2.5mm involves increased load transmission toward the radial side, reaching up to 95.7% of the total.36
Ramos-Escalona et al. reviewed 66 scaphoid fractures, in which 9.1% of patients presented with a positive ulnar, 31.8% a neutral ulnar, and 59.1% a negative ulnar. In this study it is suggested that, apart from the clinical outcome of anatomical snuffbox pain and swelling of the wrist, the negative ulnar variance should suggest a possible scaphoid fracture to us.10 Whilst distributing our 95 patients with regard to ulnar variance, we found 25 cases (26.3%) with positive variance, 36 cases (37.9%) with neutral variance and 34 cases (35.8%) with negative variance. It has not been possible to confirm the hypothesis established by Ramos-Escalona et al.10 in the references consulted.
In our study there was a total non-union rate of 18% in patients who received conservative treatment. Immobilization time in our series was 6.9 weeks (6.5–7.1 range), this is within the established range with regard to conservative treatment duration and there were no significant differences with the group of patients with consolidated fractures. However, it is lower than other series which opted to obtain up to 12 weeks immobilization.
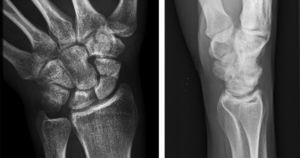
The most striking finding from the statistical analysis of our series was that the patients with an ulnar variance equal to or lower than −1mm were at a 4.6 times higher risk of presenting with non-union (Fig. 3). Ulnar variance may therefore be used as an added criterion to already existing ones and could indicate surgery of non-displaced fractures, bearing in mind that the risk is relative and in the awareness that other variables exist which could lead to the development of a non-union.
Posteroanterior and lateral projection at 3 months, after 8 weeks of conservative treatment with forearm plaster, in the same patient as appears in Fig. 1.
The main limitation of our study is that it is retrospective, and this entails a lack of control in several variables, such as the wrist radiograph technique. These radiographs are performed by experienced radiology technicians, but on occasions we found there were limitations in evaluating the different radiological measurements due to poor quality imaging. Those patients who did not comply with the necessary requisites for objective radiological assessment were withdrawn from the study.19
Statistical analysis of group 2 included 4 patients with delayed consolidation who were operated before sufficient time had elapsed to establish non-union as such.
Lastly, the size of our sample is small, but despite this, we found there were statistically significant differences between both groups.
To conclude, we believe that the results of this work provide a basis to use the ulnar variance as another criterion when deciding on the definitive treatment of a scaphoid fracture. We think it would be necessary to carry out controlled prospective studies to exhaustively analyze the role of the ulnar variance in the development of the non-union, not only in middle-third fractures but also in all scaphoid fractures.
Evidence levelEvidence level II.
Ethical disclosuresProtection of human beings and animalsThe authors declare that the procedures followed conform to the ethical regulations of the committee of responsible human experimentation and are in accordance with the World Medical Association and the Declaration of Helsinki.
Data confidentialityThe authors declare they have followed the protocols of their center of work on the publication of patient data and that all patients included in the investigation received sufficient information and gave their informed written consent to participate in said investigation.
Right to privacy and informed consentThe authors obtained the informed consent from the patients and/or subjects referred to in the article. This document is in the possession of the author of correspondence.
Conflict of interestsThe authors have no conflicts of interest to declare.
Doctor Pilar Sanchis, Doctor Silvia Tejada and Doctor Aina Yañez. University Institute of Health Sciences Research (IUNICS).
Please cite this article as: Lirola-Palmero S, Salvà-Coll G, Terrades-Cladera FJ. Análisis de la varianza cubital como factor de riesgo para el desarrollo de seudoartrosis de escafoides carpiano. Rev Esp Cir Ortop Traumatol. 2015;59:150–156.