A case is presented on a patient with a history of spondylitis ankylopoetica who suffered a neck fracture at C5–C6 level, with no neurological injury. Due to a personal history of multiple illnesses, it was decided to treat with a halo jacket. A delay in consolidation was observed after two months, so treatment with teriparatide was started at a dose of 20μg/day. Consolidation was achieved at four months (two after starting the pharmacological treatment).
Teriparatide can be an adjuvant pharmacological treatment as a stimulator of consolidation of fractures in compromised situations.
Se presenta el caso de un paciente con antecedentes de espondilitis anquilopoyética que sufrió una fractura cervical a nivel C5-C6 sin lesión neurológica. Debido a sus antecedentes personales pluripatológicos, se optó por un tratamiento con halo-chaleco. En la evolución se observó un retardo de consolidación a los dos meses, por lo que se instauró tratamiento con teriparatida a dosis de 20μg/día. La consolidación se obtuvo a los cuatro meses, dos después del comienzo con tratamiento farmacológico.
La teriparatida puede ser un tratamiento farmacológico adyuvante como estimulador de la consolidación de fracturas en situaciones comprometidas.
Spondylitis ankylopoetica (SA) is an added risk factor in injuries to the cervical spine as: (a) in the event of a fracture, the fragments are subject to the concentration of all the forces that should be dissipated in the vertebral functional units cancelled out by the disease. In these circumstances, the instability of the fracture focus increases with the consequential neurological risk and (b) patients with a long-standing condition suffer complications at the systemic level (particularly cardiorespiratory complications due to the restricted movement of the chest) and in the bones (osteoporosis).
Case reportWe present the case of a 60-year-old male with a long-standing history of SA, who suffered a chance fall with fracture and dislocation at level C5–C6 without neurological injury. Personal history: SA, secondary osteoporosis, UDB of duodenal origin requiring transfusions, acute respiratory complication during digestive endoscopy that required mechanical ventilation, septic shock by Enterococcus fecalis and Escherichia coli perhaps due to a spontaneous intestinal translocation, cholelithiasis, diverticuli in the colon, colonic polyposis with hyperplasia and dysplasia, total arthroplasty of both hips and knees with a history of infection in one case that responded without the need to remove the implant, aneurysm of the aorta remedied by an aortobifemoral prosthesis, arterial hypertension, bilateral pulmonary thromboembolism, hypersensitivity to gold salts, chronic corticoid therapy, treatment with methotrexate and with dicumarinic drugs.
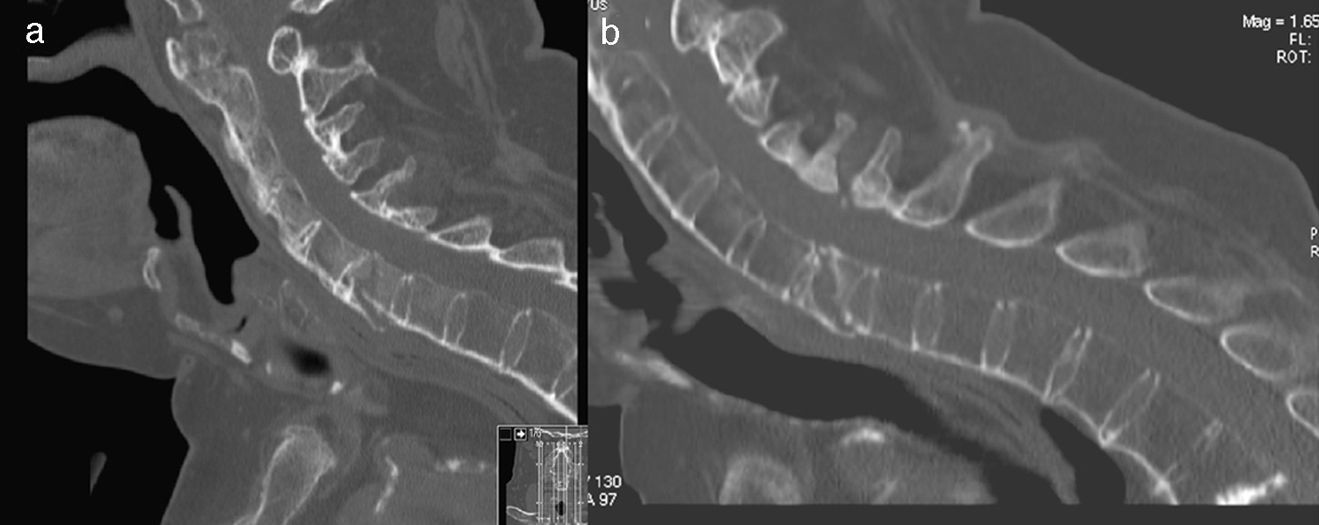
Emergency immobilization was achieved using a Philadelphia neck brace, prior to treatment with a halo jacket after 24h following consideration of the anaesthetic and surgical risk implied by his prior history. After a period of observation in hospital and retightening of the screws in the halo jacket after 48h, the patient was discharged. Two months later, he was admitted on presentation of a respiratory infection and suspected upper digestive bleeding; during admission, the dicumarinics were switched to low molecular weight heparins, the follow-up CAT scan showed a lack of consolidation of the vertebral lesion, without any sign of evolving towards consolidation with respect to the situation on admission (Fig. 1). In this situation, treatment was started with teriparatide (20μg/day), vitamin D and calcium, in addition to oral levofloxacin for the pneumonia. His respiratory condition coursed well.
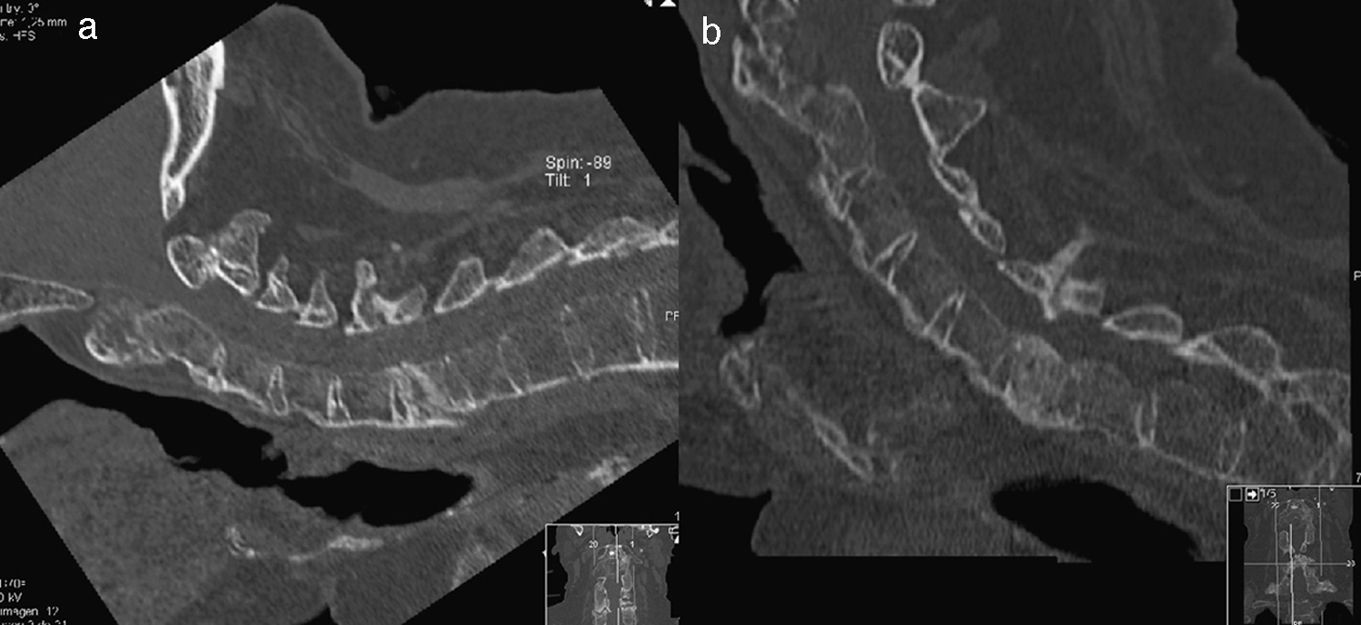
At the third month (i.e. one month after starting treatment with teriparatide), signs of consolidation were observed, with good tolerance of the halo jacket, so it was decided to retain the orthesis one month more. Three weeks later it became necessary to change the halo jacket for a Miami-type neck brace in view of the intolerance of two screws in the halo; the follow-up CAT scan ten days later showed consolidation of the vertebra, so the immobilization was gradually withdrawn over a period of 10 days (Fig. 2).
DiscussionThis lesion entails a high neurological risk, with low-energy trauma in a typical anatomical location1–4 in these SA patients, so the first aim is to immobilize the fragments to prevent medullar lesion if it has not already occurred; for this reason a halo jacket was put in place using local anaesthesia, in the operating theatre, with a final adjustment monitored via an image intensifier.
As is usual in this kind of patient, the case described here presented major comorbidities that led us to strive to avoid surgery on a patient intubated in pronus position. Some authors3,4 defend the use of surgery in these cases due to the incidence of complications in patients treated with halo jackets, but our experience, as well as that of others,5 has been different. The outcomes shown in other series might be considered biased as they probably treated conservatively those patients with a worse general status and, therefore, with a higher risk of complications with any kind of treatment, an aspect discussed with one of the authors. We also have experience with surgically treated patients, and agree with other authors in applying long posterior fixations as the best solution,2–4 versus an anterior approach.
Since morbidity was due to respiratory complications (two aspirations), it does not seem logical to attribute these to the halo jacket itself as has been proposed3; it is more probably a coincidence with regard to the choice of treatment type when faced with poor general condition.
During the course of the lesion, no signs of consolidation were observed after two months of treatment, so it was once more necessary to consider the indication of a high-risk intervention versus the need to withdraw the halo jacket shortly in view of a likely intolerance to the cranial screws. It was decided to institute treatment with teriparatide as compassionate use, following a report to the Pharmacy Department, as this was not an approved indication at the time and had a high economic cost. This report was found on experimental6 and clinical experiences in cases of delayed consolidation in fractures of the odontoid apophysis,7 proximal humerus,8 peri-prosthesis of the femur,9 radius10 and elsewhere. The exact mechanism for the action of teriparatide (fragment of amino acids 1–34 of parathormone) is not entirely defined but it is known to stimulate the osteoblasts and increases bone connectivity, the volume of bone in the spongy mass, the endostal cortical thickness and bone mineral contents.
During the clinical evolution, the formation of callus was observed, with an occasional bone bridge after one month with adjuvant pharmacological treatment and the third month with the halo in place, so it was decided to continue with it for one month more in view of the good tolerance up to that time. It became necessary to remove it three weeks later due to loosening of the screws, with a soft neck brace being used for one more week until consolidation of the fracture focus was observable using CAT.
ConclusionsTeriparatide may have a stimulant effect on the consolidation of fractures, even in high-risk patients.
Without being the ideal option in patients with spondylitis ankylopoetica, a halo jacket may be useful in high-risk surgical patients.
Level of evidenceLevel of evidence IV.
Right to privacy and informed consentThe authors declare that no patient data appears in this article.
Confidentiality of dataThe authors declare that they have followed the protocols of their work centre on the publication of patient data and that all the patients included in the study have received sufficient information and have given their informed consent in writing to participate in that study.
Protection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this investigation.
Please cite this article as: Díez Ulloa M. Paciente con espondilitis anquilopoyética y fractura cervical: retardo de consolidación en un tratamiento conservador resuelto con teriparatida. Rev esp cir ortop traumatol. 2011;55(5):378–381.