COVID 19 infection also affects obstetric patients. Regular obstetric care has continued despite the pandemic. Case series of obstetric patients have been published. Neuroaxial techniques appear to be safe and it is important to obtain the highest possible rate of success of the blocks before a cesarean section. For this reason, it is recommended that the blocks be carried out by senior anesthesiologists. The protection and safety of professionals is a key point and in case of general anesthesia, so it is also recommended to call to the most expert anesthesiologist. Seriously ill patients should be recognized quickly and early, in order to provide them with the appropriate treatment as soon as possible. Susceptibility to thrombosis makes prophylactic anticoagulation a priority.
La infección por COVID 19 afecta también a las pacientes obstétricas. La atención obstétrica habitual ha continuado a pesar de la pandemia. Existen series de casos de pacientes obstétricas. Parece que las técnicas neuroaxiales son seguras y es importante asegurarse que los bloqueos funcionen correctamente antes de una cesárea. Es por esto, que se recomienda que los bloqueos sean realizados por anestesiólogos expertos. La protección y seguridad de los profesionales es un punto fundamental y en caso de anestesia general, también se recomienda acudir al anestesiólogo más experto. Las pacientes gravemente enfermas, deben reconocerse rápida y precozmente, para poder suministrarles el tratamiento adecuado lo antes posible. La susceptibilidad a las trombosis hace que la anticoagulación profiláctica sea prioritaria.
In the past few months, a public health emergency, the COVID-19 pandemic that has affected all our hospital, has led to an unprecedented event: the suspension of all scheduled surgeries. However, obstetric service have not been interrupted, since childbirth is difficult to programme and often requires the participation of an anaesthesiologist in certain situations, such as: labour analgesia, caesarean section or surgical delivery, postpartum or postoperative care, and care for pregnant or puerperal patients with severe COVID-19.
Pregnant women are less tolerant of hypoxia and more susceptible to viral infections due to the physiological changes brought about by pregnancy. Changes in cytokine regulation and the complement cascade can affect the development and maturation of some foetal systems.
Pregnant women with different viral respiratory diseases appear to have a high risk of developing obstetric complications and adverse perinatal outcomes compared to non-pregnant women, due to changes in their immune responses. We could also assume that pregnant women may be at risk of developing severe disease and greater morbidity and mortality compared to the general population. This has been observed in other coronavirus infections contracted during pregnancy (including severe acute respiratory syndrome coronavirus [SARS-CoV] and Middle East respiratory syndrome coronavirus [MERS-CoV]) and other viral respiratory infections, such as influenza. With more than two and a half million people affected by the SARS-CoV-2 pandemic worldwide, we currently have enough data to identify and protect vulnerable population groups.1,2
There are as yet few data from published series of pregnant women with COVID-19 infection. There does not appear to be any evidence to date of a higher incidence of severe disease in pregnant patients compared to the non-pregnant population.
A series of 147 pregnant women revealed that 8% suffered from a serious respiratory disease and 1% were considered critical patients.3
The most frequent clinical presentation is fever (68%) and cough (34%). The most frequent laboratory abnormalities are: lymphopenia (59%) and elevated C reactive protein (70%). Nearly all (91%) of cases were resolved obstetrically by caesarean section, usually due to the risk of loss of foetal well-being. In this series, 3 patients required admission to the ICU and no maternal deaths were recorded. One intrauterine foetal and one neonatal death were documented. The authors recommend close surveillance during pregnancy and measures to prevent neonatal infection; vertical transmission could not be ruled out.4,5
In another recent series of 45 caesarean sections in a single hospital, most interventions were performed with spinal anaesthesia. When the anaesthesiologist wore level 3 personal protective equipment (mask with FFP2-3 filter, fluid-resistant long-sleeved surgical gown and 2 sets of gloves) and worked in a negative air pressure room, the number of infections was significantly reduced (p < 0.01).6
In recent weeks, we have been inundated with protocols and recommendations on the management of pregnant woman in terms of anaesthesia and labour analgesia. All experts recommend using regional techniques, provided the obstetric patient is not hypoxemic, tolerates decubitus (SpO2 < 93%), and the platelet count remains within acceptable ranges (>70,000–80,000/µL).5,7
Transmission to the infant can be vertical or horizontal. There is little evidence of vertical transmission (before, during, or after delivery through breastfeeding) in women who acquire the infection during the third trimester of pregnancy. The risk of horizontal transmission (droplets or contact), usually through an infected close relative, is the same as in the general population. So far, few cases in whom the presenting complaint was fever have been described.8
In the current transpandemic or transitional phase of the pandemic the entire community must be protected in view of the fact that according to available data a high percentage of pregnant women testing positive for COVID-19 are asymptomatic. In a study in 215 patients, 13.5% of pregnant women with COVID-19 were asymptomatic compared to 1.9% who exhibited mild symptoms.9 Patients should be screened by means of a clinical-epidemiological questionnaire administered over the phone and a PCR test with nasopharyngeal swab smears as soon as possible before admission to hospital.1
The aim of this review is to establish some recommendations based on the best evidence available so far (22 June 2020) for anaesthesiologists who have to provide high quality care and while guaranteeing their own safety.
We will discuss the safety of the anaesthesiologist, the organization of care, analgesia during delivery, caesarean section, postoperative care, and some specific aspects related to the pregnant or postpartum patient with severe COVID-19. As new evidence appears almost daily, the guidelines are continually evolving and may have to change in the coming months.
Personal protective equipment (PPE)These are the specialized garments used by anaesthesiologists (and other health professionals) to protect themselves and prevent the spread of infection. They constitute the first barrier against the disease, and include gloves, gowns, aprons, goggles and face shields, and face masks.
The use of PPE does not guarantee total protection, since it must be donned and doffed correctly, and rigorous hand hygiene must be performed.10,11 It is advisable to follow the recommendations of the local occupational medicine/occupational risk protection and/or preventive medicine services, if available. Otherwise, the recommendations of the Ministry of Health and scientific societies must be followed,12 and training workshops or simulation sessions should be held to train staff, drawing up a self-help checklist for donning and doffing and finally, if possible, arrange for supervised doffing.
The technical aspects of each mask and PPE component are beyond the scope of this review.
We suggest taking precautionary measures and using the highest level of protection when administering general anaesthesia and whenever neuraxial block is likely to be converted to general anaesthesia. We also recommend drawing up an algorithm for dealing with a failed nerve block in both COVID and non-COVID positive patients.
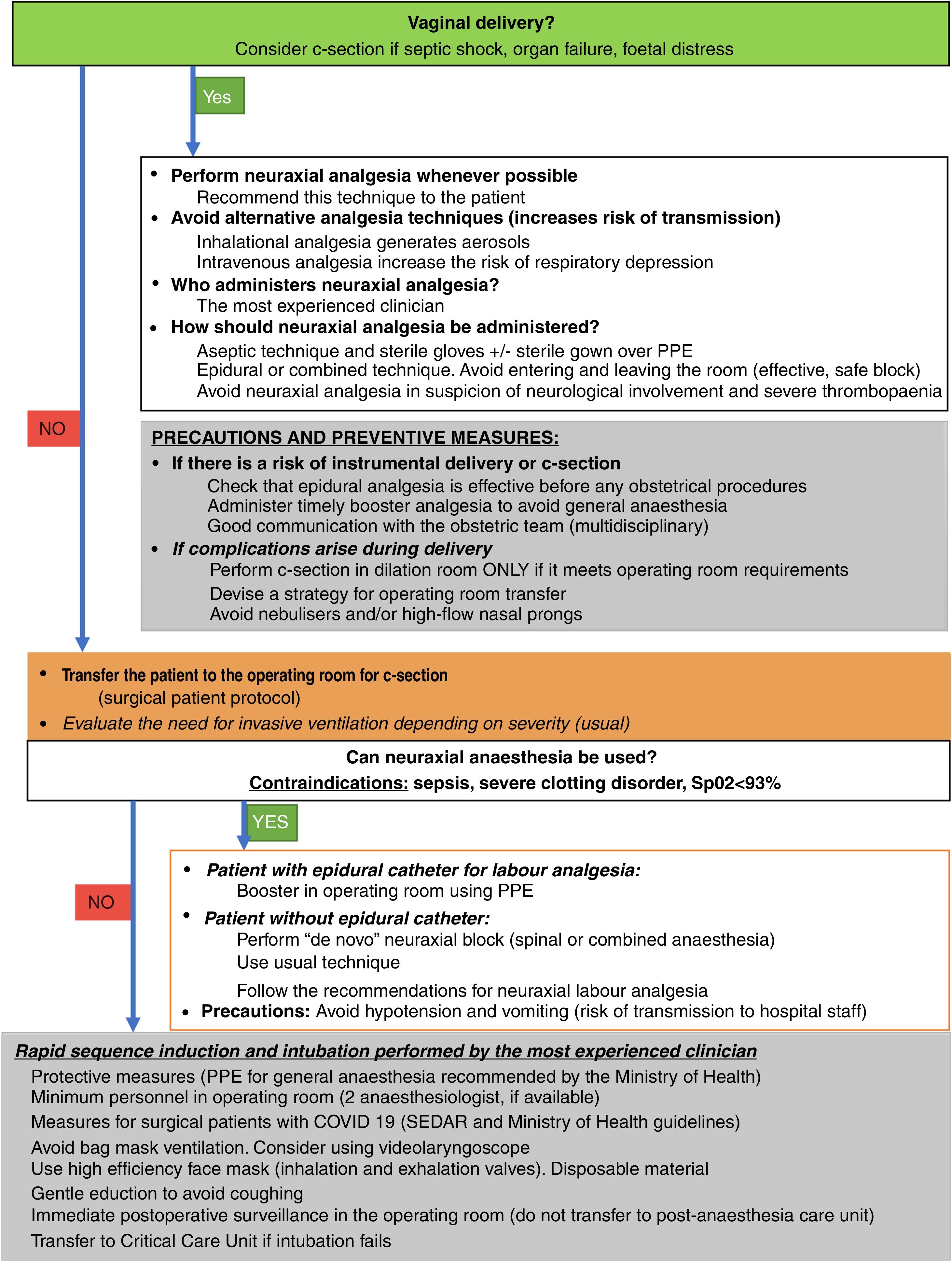
Pregnant woman with COVID-19: mild, moderate or severe illnessPatients may need to be sent to different services and receive different treatment, depending on the severity of their symptoms. Anaesthesiologists are part of the multidisciplinary team involved in assessing the severity of these patients, their follow-up and their perioperative care. Therefore, a detailed assessment of the pregnant patient at admission using algorithms such as the one presented in Fig. 1 will maximise the efficiency of the care provided:
- •
Diagnose patients with severe disease with pneumonia immediately in the preliminary examination if there are signs of respiratory failure (SaO2 < 90% room air, 93% in pregnant women) or respiratory rate ≥ 30 RPM, or failure of one or more organs, or need for vasopressors.13
- •
In the case of moderate disease (uncomplicated pneumonia), conventional oxygen therapy at different concentrations is the first therapeutic step in patients with hypoxaemia (SpO2 < 90% and < 93% in the case of pregnant women, breathing room air).
- •
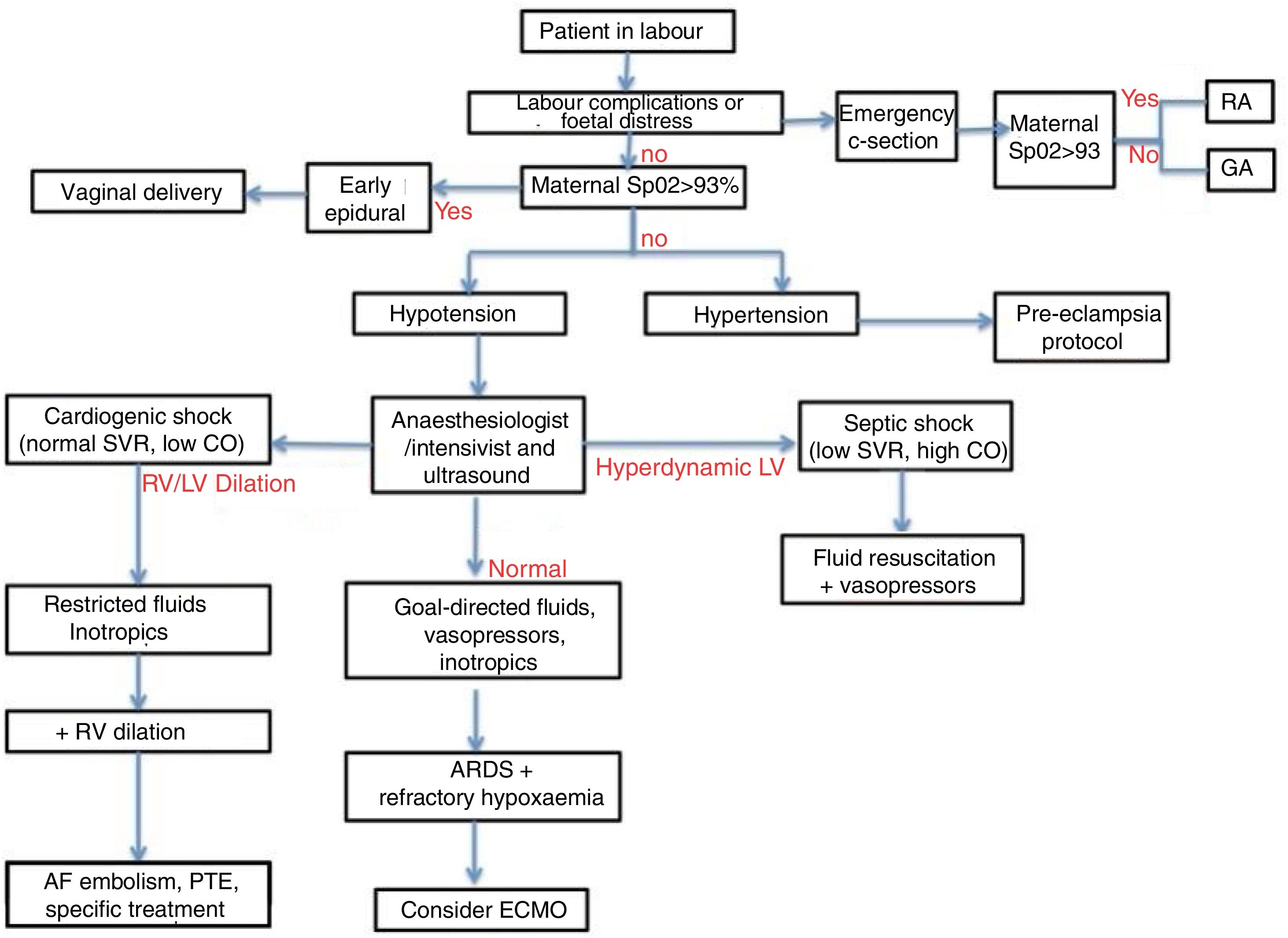
The aim should be to adjust FiO2 (by means of oxygen therapy with nasal goggles or a Venturi mask) to 0.4 or 40% to maintain an adequate level of oxygenation, considered SpO2 > 91% and > 93% in pregnant women. Oxygen administration is a low-risk aerosol-generating procedure, and is therefore suitable for COVID-19 patients.
All staff involved must coordinate efforts to ensure the protection and care of patients and healthcare professionals and to avoid nosocomial transmission of the new coronavirus infection (Fig. 2).
Diagnostic-therapeutic algorithm for SARS-CoV2 infection in the parturient. AF: amniotic fluid; ARDS: respiratory distress; CO: cardiac output; ECMO: extracorporeal oxygenation; GA: general anaesthesia; LV: left ventricle; PTE: pulmonary thromboembolism; RA: regional anaesthesia; RV: right ventricle; SVR: systemic vascular resistance.
In a patient with COVID-19, professionals are at the greatest risk of viral transmission when they are exposed to direct contact with droplets from the airway during manipulation, particularly during tracheal intubation and extubation.14
The proper use of PPE and proper hand hygiene are factors that can significantly help reduce transmission of the virus.
Don and doff PPE following a strict, previously rehearsed protocol and, in the case of neuraxial analgesia for delivery, it must be donned outside the patient’s room.
The following recommendations have been published since the beginning of the pandemic1:
- •
Pregnant women with SARS-CoV-2 infection should receive the same isolation measures used for infected non-pregnant patients.
- •
The patient must remain under the same isolation conditions during dilation and/or delivery and postpartum recovery.
- •
Surgical procedures in obstetric patients should be planned and coordinated by a multidisciplinary team as far in advance as possible.
- •
Do not send women to a ward shared with other post-anaesthesia recovery patients in order to avoid infecting other patients and/or healthcare professionals.
- •
Evidence regarding neonatal safety is sparse. It is essential to coordinate with the paediatric team in order to plan the care of the infant from birth.
Personal protection (PPE) is a priority: FFP2 or FFP3 masks are mandatory during airway management, together with gloves, a fluid-resistant long-sleeved surgical gown and waterproof goggles, in accordance with the recommendations of the WHO, the Ministry of Health, and other national and international organizations and societies.
Staff must receive training and practice correct donning and doffing of PPE.
The treating anaesthesiologist must take level 3 precautions when performing general anaesthesia, or when there is a high risk of conversion from regional to general anaesthesia.14
Recommendations for labour analgesia in obstetric patients with COVID-19Very little data have been published so far, but the number of cases and series is growing steadily.
Neuraxial analgesia is recommended for women with suspected or confirmed COVID-19 infection. There is no evidence that this is contraindicated, and the use of these techniques may avoid the need for general anaesthesia in an emergency.5,6,15
However, mild thrombocytopaenia has been described in hospitalised non-pregnant patients with COVID-19. In patients with a higher severity level, thrombocytopaenia may be more severe, although platelet counts below 100,000/µL are rare.16
The effectiveness of the block should be closely monitored to avoid the risk of a failed block if caesarean section is needed. Protocols for dealing with nerve block failure should be drawn up in each hospital.17
The minimum PPE required for an epidural block is: cap, googles, surgical mask, fluid-resistant long-sleeved surgical gown and sterile gloves.18
Epidural analgesia is often associated with intrapartum fever. If the patient is also COVID-19 positive, the fever should be monitored even more closely since it can have a negative effect of the feotus.19
The following are the recommendations for performing anaesthesia1:
- 1
Neuraxial blockade:
- •
Administer neuraxial blockade (epidural or combined) early to avoid the possibility of an urgent caesarean section under general anaesthesia.
- •
Make sure a recent platelet count is available given the possibility of mild thrombocytopaenia associated with COVID-19 infection.
- •
There is no evidence that any particular neuraxial technique is more risky than any other, so the decision will depend on the anaesthesiologist (epidural, spinal, or combined) and local practice.
- •
- 2
Regarding alternatives to neuraxial analgesia:
- •
Do not administer inhalational analgesia due to the high risk of aerosol generation and airborne spread of the virus.
- •
Intravenous analgesic techniques with remifentanil require close, direct monitoring by the anaesthesiologist, and may increase the risk of transmission to personnel, in addition to increasing the risk of hypoxia in a patient with pneumonia.
- •
Do not administer remifentanil in women with COVID-19 and SpO2 < 95%, with or without supplemental oxygen.
- •
It is important to insist that the obstetric environment is a setting in which communication and multidisciplinary work are fundamental. The very nature of the procedures performed in this setting means that quick decisions frequently have to be made, and these must be made on a multidisciplinary and protocolized basis whenever possible.
Patients with suspected COVID-19 or confirmed cases should be carefully evaluated for possible specific complications or for signs of severity.
During the anamnesis, which can be performed online, patients should be asked about their signs and symptoms, the most common being fever, cough, and taste and smell alterations. Patients can also be asked about signs of respiratory failure and, at present, a PCR test is recommended for all pregnant women before admission. Basic labs and a complete metabolic panel are advisable, and arterial blood gas can also be measured, depending on the patient’s clinical status. In patients with respiratory involvement, radiological studies can be ordered, based on severity and diagnostic suspicion, and whenever possible the patient should be fully informed and consent to all procedures and tests.5
The risks and/or benefits of tocolysis, corticosteroids for foetal maturation, magnesium sulphate for foetal neuroprotection, etc., have yet to be fully established in the COVID-19 patient.20
Before taking the patient to the operating room for a caesarean section, a plan should be discussed and agreed upon regarding: transfer to the operating room, prior donning of the recommended PPE, the drugs and procedures required, the post-anaesthetic care setting, and the destination in the hospital ward. Careful planning of the COVID-19 patient circuit is essential to ensure the safety of the entire team.
Before administering neuraxial block, it is advisable to have a recent platelet count, not necessarily from the same day, to check for thrombocytopaenia. Thrombocytopaenia described in COVID-19 cases has so far been mild, and never below what is considered the safe threshold of 80,000 µL.
Obstetric patients diagnosed with COVID-19 are frequently treated with low molecular weight heparin as a prophylactic or therapeutic measure. It is important to respect the safety windows of these drugs in order to avoid potentially serious complications.
Standard monitoring can be used, with particularly attention to pulse oximetry, where the goal is to maintain SpO2 above 95% (with or without oxygen).5 Tools such as modified early obstetric warning systems (MEOWS) can be helpful.21
Women with SpO2 < 95% or who require supplemental oxygen to maintain this level of saturation should undergo a blood gas analysis as soon as possible, and should be monitored for signs of requiring mechanical ventilation. The progressive need for oxygen is a marker of deterioration.22
Once placed on mechanical ventilation, it is important to remember that physiological PaCO2 in pregnant women is between 28 and 32 mmHg, taking into account the increased supply of oxygen to the foetus, although the priority is to maintain maternal oxygenation.
Caesarean section in a COVID-19 patient (suspected or confirmed)There are a number of key considerations to take into account to ensure success and increase the safety of the staff and, therefore, of the mother14:
- •
Arrange adequate transport from the dilation room or ward to the operating room. A synchronized and safe transfer must be guaranteed.
- •
Minimise the number of people in the operating room.
- •
Draw up a list of drugs needed in the COVID operating room (a specific "check list" together with additional drugs needed for the specific needs of the patient).
- •
Record intraoperative events, vital signs, and the anaesthesia procedure (electronic or printed).
- •
Agree on a strategy for postoperative care.
Whenever possible, a specific COVID operating room and circuit will be designed, separate from the non-COVID circuit. If this is not possible in the operating room, the COVID patient will be scheduled last, to facilitate cleaning.
Neuraxial anaesthesia performed by an expert anaesthesiologist with adequate protective equipment is recommended to avoid delays and/or accidents if the procedure needs to be converted to general anaesthesia.
Spanish recommendations for caesarean section in COVID-19 patient are as follows1:
Before caesarean section: prepare the operating room and the necessary medication, plan the procedure, and don PPE. Assign a postoperative recovery room by consensus, based on the patient's condition and her needs, and plan the transfer (operating room, PACU, ICU).
Regarding the caesarean section: general anaesthesia is a high-risk procedure and therefore is not recommended as the first option for caesarean section.
General anaesthesia is recommended if the COVID-19 patient has SpO2 < 93% (despite supplemental oxygen). Intubation will be performed by the most experienced clinician. Standard protocols for pregnant women will be followed in terms of pre-oxygenation and rapid sequence induction (local protocol is recommended), etc.5
If intubation is difficult, the use of a second-generation video laryngoscope and/or supraglottic devices is suggested as an initial option, provided the anaesthesiologist is experienced in their use.
Check the tube position using capnography, not auscultation.
Minimise the number of people in the operating room.
Extubation is a risky procedure. Avoid emergent coughing - plastic shields can be used to protect staff from aerosols.
Neuraxial anaesthesia (spinal, epidural, or combined), if not contraindicated, is the recommended technique.
Prevent arterial hypotension with the appropriate use of vasopressors. This strategy will also help prevent intraoperative vomiting. The use of routine additional antiemetic prophylaxis, but not dexamethasone, is recommended.5,23
Use local algorithms for dealing with blockade failure in order to minimize the possibility of general anaesthesia due to insufficient block.
Urgent caesareanNeuraxial anaesthesia is still the recommended technique to avoid the risks associated with aerosolization.6,23
If there is a risk of conversion to general anaesthesia, anaesthesia personnel should use level 3 personal protective measures.24
If general anaesthesia is required, a «check list» for general anaesthesia can be adapted to caesarean section.25 Follow standard precautions and measures for general anaesthesia for caesarean section in COVID-19 cases.26
Take particular care to avoid accidental disconnection of the breathing circuit to avoid accidental viral contamination.
Physiological changes caused by pregnancy and COVID infection make the obstetric patient more susceptible to hypoxia, so pre-oxygenation is important, although the use of high-flow nasal prongs is generally not recommended.
Double gloving is best for intubation, given the possibility of contamination by secretions.
To avoid emergent coughing, use dexmedetomidine, remifentanil, fentanyl, or IV or tracheal lidocaine.27
The benefit of these strategies in the COVID patient has not yet been established, and evidence may appear in the coming months.
In the pregnant patient undergoing urgent or non-delayable non-obstetric surgery, the usual recommendations for each case plus current prevention measures for patients with suspected or confirmed COVID-19 infection might be applicable.
Postoperative careAfter surgery, isolate the patient and transfer her to a COVID area.
Extubated patients should wear a surgical mask during transfer.5,14 If they are transferred with supplemental oxygen, place the mask over the delivery system.
There is no data to indicate that non-steroidal anti-inflammatory drugs should not be used for the treatment of postoperative pain in patients with COVID-19.28
With regard to deciding whether to separate the mother from the infant or not, the Spanish Ministry of Health has published recommendations in this regard,1 and other guidelines are also available on mother-infant separation and breastfeeding.29
There is increasing evidence regarding hypercoagulability, given that several factors combine in these patients (hospitalization, infection and pregnancy), together with isolation. Health authorities in the UK recommend giving LMWH to any pregnant woman hospitalized with suspected or confirmed COVID-19, unless the birth is expected within 12 h.24
Standards of care for obstetric patients must be maintained despite the pandemic, and hospitals must make every effort to provide and maintain those standards.14
National recommendations are as follows1:
Pregnant women with SARS-CoV-2 infection should receive the same isolation measures used for infected non-pregnant patients. Keep the patient under the same isolation conditions during dilation and/or delivery and postpartum recovery.
There is evidence of hypercoagulability in pregnancy and in patients with COVID-19. We suggest applying the SEDAR guidelines and recommendations for anticoagulation in COVID-positive pregnant women. Health authorities in the UK recommend giving prophylaxis with LMWH to any pregnant woman hospitalized with suspected or confirmed COVID-19, unless the birth is expected within 12 h.24
Do not send women to a ward shared with other post-anaesthesia recovery patients in order to avoid transmission to other patients and/or healthcare professionals.
There are no data on the safety of blood patches in post-dural puncture headache (no cases have been described so far). Sphenopalatine ganglion block can generate aerosols, and should therefore be avoided as a therapeutic option for post-dural puncture headache.
Personal protection is a priority: FFP2 or FFP3 masks are mandatory during airway management, together with gloves, a fluid-resistant long-sleeved surgical gown and waterproof goggles, in accordance with the recommendations of the WHO, the Ministry of Health, and other national and international organizations and societies. The treating anaesthesiologist must take level 3 precautions when performing general anaesthesia, or when there is a high risk of conversion from regional to general anaesthesia.14
It is important to promptly examine pregnant women with severe COVID-19 infection and perform differential diagnosis with other conditions. The inclusion of specialists in critical care (anaesthesiologist or intensivist) and the performance of ultrasound studies will help decide the most appropriate treatment (Fig. 2).
ConclusionsAlthough obstetric patients may have a higher susceptibility to COVID-19 infection, this does not appear to be the case at present.
Multidisciplinary teamwork is fundamental in these patients, since the safety of many people is at stake.
Neuraxial anaesthesia and analgesia techniques appear to be safe in the obstetric patient.
Consider administering routine anticoagulation.
It is important to practice donning and doffing PPE for the safety of all concerned.
There are more uncertainties than certainties, but common sense and a few tips can help.
Conflicts of interestThe authors declare that they have no conflicts of interest.
Please cite this article as: Guasch E, Brogly N, Manrique S. Recomendaciones prácticas en la paciente obstétrica con infección por COVID-19. Rev Esp Anestesiol Reanim. 2020;67:438–445.