During the last decades, benzodiazepines (BZD) and antidepressants (ADP) have been among the most prescribed therapies in all developed countries. They have side effects, and BZD carry a risk of abuse and dependence disorders. The purpose of this study was to evaluate the prevalence of BZD and ADP among patients who attend a Rheumatology clinic, as well as the indication for these drugs.
MethodsThe study included patients who were referred for the first time to the Rheumatology clinic. Demographical data, reason for referral, and final diagnosis were recorded. The indication for ADP and/or BZD was recorded, as well as the duration of treatment. Sample size was estimated for a 0.05% alpha risk. Univariate and multivariate analyses were performed in order to study the relationships with the demographical or clinical characteristics.
ResultsA total of 350 patients were included (women 77.1%, men 22.9%). Most of them (73.4%) had been referred for musculoskeletal pain. More than a third (36.6%) of patients were on BZD and/or ADP. The most frequent reasons for their prescription were anxiety, depression, and insomnia. The final diagnosis in the clinic was a non-inflammatory condition in 82%, and an inflammatory one in 18%. In the univariate analyses, the use of BZD/ADP was associated with female gender (p<.001), unemployment (p<.001) and non-inflammatory final diagnosis (p<.001). In the multivariate analyses, the use of BZD and/or ADP was associated with female sex (p=.002 [OR 3.4, 95% CI; 1.6–7.4]), and a non-inflammatory final diagnosis, specifically fibromyalgia (p=.007 [OR 16.1, 95% CI; 2.2–120.7]).
ConclusionUse of BZD and ADP is high and associated with non-inflammatory disease.
Durante las últimas décadas, las benzodiacepinas (BZD) y los antidepresivos (ADP) han estado entre las terapias más prescritas en todos los países desarrollados. Estos fármacos tienen efectos secundarios y las BZD pueden ocasionar abuso y problemas de dependencia. El objetivo de este estudio fue evaluar la prevalencia de consumo de BZD y ADP entre los pacientes que acuden a una consulta de reumatología por primera vez, así como la indicación para ellos.
MétodosSe incluyeron pacientes remitidos por primera vez a la consulta de reumatología. Se registraron los datos demográficos, el motivo de la derivación y el diagnóstico final. Con respecto al tratamiento con ADP y/o BZD, se registraron su duración y la indicación de la prescripción. El tamaño de la muestra se estimó para un riesgo alfa de 0,05%. Se realizaron análisis univariantes y multivariantes para estudiar las asociaciones con características demográficas o clínicas.
ResultadosSe incluyeron 350 pacientes (mujeres 77,1%, hombres 22,9%). La mayoría de ellos habían sido remitidos por dolor musculoesquelético (73,4%). Más de un tercio (36,6%) de los pacientes estaban en tratamiento con BZD y/o ADP. Las causas más frecuentes para su prescripción fueron ansiedad, depresión e insomnio. El diagnóstico final fue patología no inflamatoria en el 82% de los casos e inflamatoria en el 18% de estos. En el análisis univariante, el uso de BZD y/o ADP se asoció con el sexo femenino (p<0,001), el desempleo (p<0,001) y el diagnóstico de patología no inflamatoria (p<0,001). En el análisis multivariante, el uso de BZD y/o ADP se asoció con el sexo femenino (p=0,002 [OR 3,4; IC 95% 1,6-7,4]) y el diagnóstico de patología no inflamatoria, específicamente con la fibromialgia (p=0,007 [OR 16,1; IC 95% 2,2-120,7]).
ConclusiónEl consumo de BZD y ADP es frecuente y está asociado con patología no inflamatoria.
Benzodiazepines (BZD) are a group of psychotropic drugs with mainly anxiolytic effect. Their mechanism of action is based on their indirect gamma-aminobutyric acid (GABA) agonist effect. Nowadays they are one of the most prescribed groups of drugs in medical practice.1,2 According to a study carried out in 2004,3 the use of anxiolytics and hypnotics in Spain experienced a growth of 56% from 1995 to 2002, with an average annual increase of 2.78 DDD (Defined Daily Dose) per 100 inhabitants per day.
On the other hand, antidepressants (ADP)4 are the drugs to treat the symptoms of depression. There are four main types: SSRIs (Selective Serotonin Reuptake Inhibitors); IRSNs (Selective Serotonin and Norepinephrine Reuptake Inhibitors); Tricyclic; MAOIs (Monoamine oxidase inhibitors). ADPs can be used to treat other conditions such as: moderate to severe depression (also mild depression depending on individual profiles), severe anxiety and panic attacks, obsessive compulsive disorder; chronic pain; eating disorders and post-traumatic stress disorder. The use of ADP5 has tripled in Spain between 2000 and 2013, going from 26.5 to 79.5 doses per 1000 inhabitants.
Our objective was to evaluate the prevalence of BDZ and/or ADP use among those patients who were referred for the first time to a Rheumatology consult for evaluation, as well as the indication. We also aimed to study the association of these drugs to any clinical or sociodemographic characteristic of the patients.
Materials and methodsPatientsDescriptive cross-sectional study carried out in five hospitals in the province of Alicante (Southeast of Spain). Patients referred for the first time to the Rheumatology clinic were consecutively included between January 1 and April 1, 2019. The inclusion criteria were age (adults over 18 years old) and acceptance to participate by signing the informed consent.
All the data were collected at this first visit. Sociodemographic date included: age, job situation (active, unemployed, student, retired, and pensioner/disabled) and partner/marital status (single, married/partner, widow, divorced). Clinical data included: the initial clinical suspicion for referral to Rheumatology; the specialist referring; the use of ADP and/or BZD, its indication (pain, anxiety, depression, insomnia, others), duration and prescriber; and the final diagnosis according to the Rheumatologist (inflammatory/autoimmune condition; fibromyalgia; bone disorder-like osteoporosis or Paget's disease-; and other non-inflammatory conditions such as osteoarthritis or soft tissue disorders).
The study was approved by the ethical committee for scientific research of the Hospital General Universitario de Elche with the code AAC-BZD-2018-01 and was carried out following the precepts of the Declaration of Helsinki.
Statistical studyAssuming an alpha risk of 0.05%, a sample size of 350 patients was calculated. A descriptive statistical analysis was performed in which the quantitative variables are presented as means and standard deviations and the qualitative ones as frequencies and percentages. The independent variable was the use of BZD and/or ADT; its association with socio-demographic variables and clinical variables was studied, first by simple logistic regression, establishing the significance level at p<0.05. Then, ANOVA multivariate analysis was performed and the odds ratio (OR) calculated, for which a 95% confidence interval (CI) was estimated. Secondly, the same association study was carried out for the use of BZD and ADT separately. For the association study, two models were used. First, with any of the individual dependent variables described. Second, reclassifying the employment situation and the final diagnosis. The employment situation was reclassified into “active” and “not active” (retired, unemployed, pensioner/disabled). The final diagnosis was reclassified into “inflammatory” and “non-inflammatory” (bone disorders, fibromyalgia, osteoarthritis, soft tissue disorders and others). The data were analysed using the statistical program “SPSS”, version 25 (IBM).
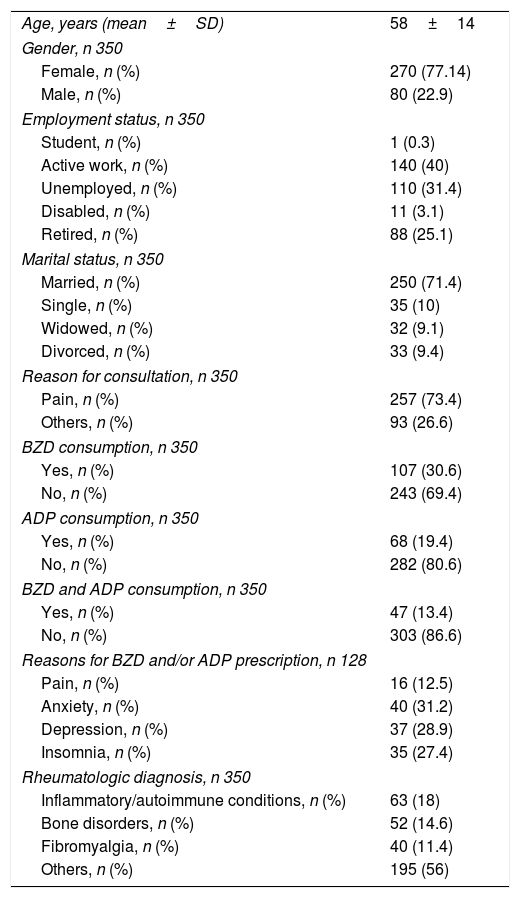
ResultsDescriptive studyWe included 350 patients, 270 women and 80 men, with a mean age of 58 years old. Concerning job status, 40% had active work and 31.4% were unemployed. 250 patients were married or lived as a couple (71.4%). The main reason for referral to the Rheumatology clinic was the presence of musculoskeletal pain (73.4%), others (26.6%) causes of consultation were a compendium of less frequent complaints including: loss of strength, asthenia, inflammation, Raynaud's phenomenon, constitutional syndrome and also osteoporosis. A total of 128 patients (36.6%) were on BZD and/or ADP treatment at the time of the visit: 107 patients were taking BZD (30.6%), 68 ADP (19.4%), and 47 (13.4%) both treatments. The most frequent reasons for BZD and/or ADP prescription were anxiety (31.2%), depression (28.9%) and insomnia (27.4%), with much less frequent indication for musculoskeletal pain (12.5%). Most of the BZD and/or ADP prescriptions had been made by the family doctor (68%). The final diagnosis according to the Rheumatologist were: inflammatory/autoimmune conditions 18%; bone disorders 14.6%; fibromyalgia 11.4%; others (like soft tissue disorders or osteoarthritis) 56%. Results are shown in Tables 1 and 2.
Characteristics of the study subjects.
| Age, years (mean±SD) | 58±14 |
| Gender, n 350 | |
| Female, n (%) | 270 (77.14) |
| Male, n (%) | 80 (22.9) |
| Employment status, n 350 | |
| Student, n (%) | 1 (0.3) |
| Active work, n (%) | 140 (40) |
| Unemployed, n (%) | 110 (31.4) |
| Disabled, n (%) | 11 (3.1) |
| Retired, n (%) | 88 (25.1) |
| Marital status, n 350 | |
| Married, n (%) | 250 (71.4) |
| Single, n (%) | 35 (10) |
| Widowed, n (%) | 32 (9.1) |
| Divorced, n (%) | 33 (9.4) |
| Reason for consultation, n 350 | |
| Pain, n (%) | 257 (73.4) |
| Others, n (%) | 93 (26.6) |
| BZD consumption, n 350 | |
| Yes, n (%) | 107 (30.6) |
| No, n (%) | 243 (69.4) |
| ADP consumption, n 350 | |
| Yes, n (%) | 68 (19.4) |
| No, n (%) | 282 (80.6) |
| BZD and ADP consumption, n 350 | |
| Yes, n (%) | 47 (13.4) |
| No, n (%) | 303 (86.6) |
| Reasons for BZD and/or ADP prescription, n 128 | |
| Pain, n (%) | 16 (12.5) |
| Anxiety, n (%) | 40 (31.2) |
| Depression, n (%) | 37 (28.9) |
| Insomnia, n (%) | 35 (27.4) |
| Rheumatologic diagnosis, n 350 | |
| Inflammatory/autoimmune conditions, n (%) | 63 (18) |
| Bone disorders, n (%) | 52 (14.6) |
| Fibromyalgia, n (%) | 40 (11.4) |
| Others, n (%) | 195 (56) |
SD: standard deviation, BZD: Benzodiazepines, ADP: antidepressants.
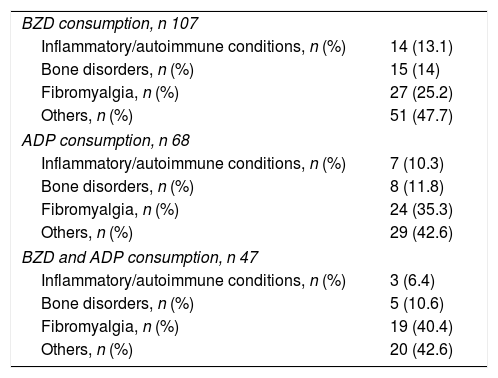
Consumption of BZD and/or ADP according with the Rheumatologic diagnosis.
| BZD consumption, n 107 | |
| Inflammatory/autoimmune conditions, n (%) | 14 (13.1) |
| Bone disorders, n (%) | 15 (14) |
| Fibromyalgia, n (%) | 27 (25.2) |
| Others, n (%) | 51 (47.7) |
| ADP consumption, n 68 | |
| Inflammatory/autoimmune conditions, n (%) | 7 (10.3) |
| Bone disorders, n (%) | 8 (11.8) |
| Fibromyalgia, n (%) | 24 (35.3) |
| Others, n (%) | 29 (42.6) |
| BZD and ADP consumption, n 47 | |
| Inflammatory/autoimmune conditions, n (%) | 3 (6.4) |
| Bone disorders, n (%) | 5 (10.6) |
| Fibromyalgia, n (%) | 19 (40.4) |
| Others, n (%) | 20 (42.6) |
BZD: Benzodiazepines, ADP: antidepressants.
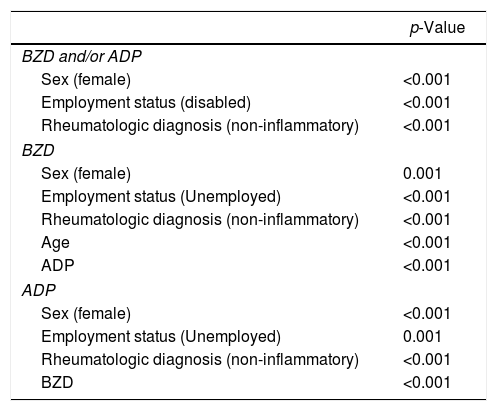
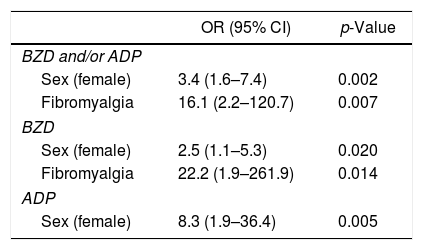
In the univariate analysis the use of BZD and/or ADP was associated with female sex (p<0.001), employment status “disabled” (p<0.001) and final diagnosis “non-inflammatory” (p<0.001). Results are shown in Table 3. In the multivariate analysis (Table 4), the association with female sex was confirmed [p=0.002; OR 3.4 (95% CI 1.6–7.4)] and an association was found with the final diagnosis of fibromyalgia [p=0.007; OR 16.1 (95% CI 2.2–120.7)] (Table 4). No association was found between the consumption of psychotropic drugs and age.
Univariate analysis.
| p-Value | |
|---|---|
| BZD and/or ADP | |
| Sex (female) | <0.001 |
| Employment status (disabled) | <0.001 |
| Rheumatologic diagnosis (non-inflammatory) | <0.001 |
| BZD | |
| Sex (female) | 0.001 |
| Employment status (Unemployed) | <0.001 |
| Rheumatologic diagnosis (non-inflammatory) | <0.001 |
| Age | <0.001 |
| ADP | <0.001 |
| ADP | |
| Sex (female) | <0.001 |
| Employment status (Unemployed) | 0.001 |
| Rheumatologic diagnosis (non-inflammatory) | <0.001 |
| BZD | <0.001 |
BZD: Benzodiazepines, ADP: antidepressants.
Multivariate analysis.
| OR (95% CI) | p-Value | |
|---|---|---|
| BZD and/or ADP | ||
| Sex (female) | 3.4 (1.6–7.4) | 0.002 |
| Fibromyalgia | 16.1 (2.2–120.7) | 0.007 |
| BZD | ||
| Sex (female) | 2.5 (1.1–5.3) | 0.020 |
| Fibromyalgia | 22.2 (1.9–261.9) | 0.014 |
| ADP | ||
| Sex (female) | 8.3 (1.9–36.4) | 0.005 |
OR: Odds Ratio, BZD: Benzodiazepines, ADP: antidepressants.
In the univariate analysis, the use of BZD was associated with older age (p<0.001), female sex (p=0.001), employment status “not active” (p<0.001), the use of ADT (p<0.001) and at the final “non-inflammatory” diagnosis (p<0.001) (Table 3). In the multivariate analysis, only association with female sex was found [p=0.02; OR 2.5 (95% CI 1.1–5.3)] and fibromyalgia diagnosis [p=0.014; OR 22.2 (95% CI 1.9–261.9)] (Table 4).
Use of ADP aloneIn the univariate analysis, the use of ADT was associated with female sex (p<0.001), “not active” employment status (p=0.001), BDZ use (p<0.001) and final “non-inflammatory” diagnosis (p<0.001) (Table 3). In the multivariate analysis, only association with female sex was found [p 0.005 (OR 8.3, 95% CI 1.9–36.4)] (Table 4).
Any treatment, alone or combined, was associated with the civil status.
DiscussionOur results show that more than a third of the patients who come to the Rheumatology clinic for the first time were on BZD and/or ADP. The BZD prescription among these patients was higher than that observed in the Spanish general population (30.6% vs 18.7%).6 Similarly, the ADP prescription was also higher comparing with the general population (19.4% vs 8.5%).7 They had been both prescribed mostly by de general practitioner, and musculoskeletal pain accounted for a small part of the indications.
The use of psychotropic drugs was in all our analyses consistent and associated with the female sex and the diagnosis of non-inflammatory conditions. The use of BZD was also associated with older age in the univariate study, which has already been reported in other international works.8,9 The use of BZD was shown to increase from 2.6% at 18–35 years old, to 8.7% at 65–80 years old in the American population.8 In a systematic review, prolonged use of BZD was also associated with older patient age.10 We also found an association with the “not active” employment situation. In an Italian population survey, unemployment was associated with a higher consumption of BZD.11 In a series of German patients, clear association between unemployment and a longer use of BZD was found.12 On the other hand, in our series, patients who consumed BZD had also higher probability of using ADP in the univariate study. Previous studies have already described an association between ADP consumption and increased use of BZD.13,14 However, in our series, the use of BZD was not associated with unemployment, age, or ADP consumption in the multivariate analyses. This could be explained by an insufficient sample size. We only found association with the female sex and with the diagnosis of non-inflammatory pathology. The higher prevalence of BZD consumption in the female sex has been corroborated in other studies,15,16 as well as the association with non-inflammatory pathology, especially with fibromyalgia, an entity characterized by the presence of pain.
Concerning the use of ADP in our patients, in the univariate analysis we observed association with age, unemployment, consumption of BZD and with the diagnosis of fibromyalgia. Other studies17 have also communicated an increased use of ADP in older people. However, in the multivariate analysis, we found only an association with female sex, which has also been described in previous works.18 On the other hand, ADPs may be helpful as adjuvant therapy to the treatment of different rheumatic conditions, mainly those with chronic pain, because they enhance the effect of opioids or non-steroidal anti-inflammatory drugs.19 They can be used in chronic sever rheumatic conditions with sequelae, but overall in fibromyalgia.20 Among them, duloxetine and amitriptyline are the most frequently recommended antidepressants. Prevalence of musculoskeletal pain varies with age and sex. It has been communicated that neck, shoulders, knees and back pain are 1.5 times more common in women, while fibromyalgia is up to 4 times more frequent in women.21 In our study, more than two thirds were women, which may have influenced the association results by a selection bias.
Nevertheless, it is remarkable that in our series of patients who attend a Rheumatology consult for the first time, the use of psychotropic drugs is frequent; it is mostly prescribed in the primary care setting for psychiatric needs over all and these patients are finally diagnosed with non-inflammatory conditions. That is to say, patients on psychotropic drugs who attend a Rheumatology consult are more probably being finally diagnosed with a non-inflammatory condition. Nevertheless, we need to remember that most of the patients were referred to Rheumatology because of pain which may be a frequent symptom in conditions such as depression22 or anxiety. The main limitation of this study is its cross-sectional design, so we cannot make conclusions about the definite association between the use of BZD and/or ADP and a final Rheumatology diagnosis.
In conclusion, the use of BZD and ADP is frequent among the patients who attend a Rheumatology consult for the first time, and they are associated to a final non-inflammatory condition diagnosis.
Conflicts of interestThe authors declare that they have no conflict of interest.