Calcific tendinopathy of the shoulder is characterised by the deposit of hydroxyapatite crystals in one or more tendons of the shoulder. Within the processes that occur in this disorder, there is the resorption phase, in which the deposits could migrate towards adjacent structures. A very rare complication is the migration towards the myotendinous junction of the corresponding tendon, which causes a significant muscular inflammatory reaction that can be seen in specific complementary tests. A clinical case is presented of a subscapular calcific tendinopathy, with subsequent migration to the myotendinous junction, causing myositis of the same.
La tendinopatía calcificada del hombro se caracteriza por el depósito de cristales de hidroxiapatita en uno o varios tendones del hombro. Dentro de los procesos que ocurren en esta entidad está la fase de reabsorción, en la que los depósitos podrían migrar hacia estructuras adyacentes. Una muy rara complicación es la migración hacia la unión miotendinosa del tendón correspondiente, la cual provoca una importante reacción inflamatoria muscular que puede objetivarse en pruebas complementarias específicas. Presentamos un caso clínico de una tendinopatía calcificante del subescapular, con posterior migración hacia la unión miotendinosa causando una miositis del mismo.
Calcific tendinopathy of the shoulder is a disease with a high prevalence, and without a completely clear pathogenesis.1 One of its complications could be the migration of the calcification towards the myotendinous junction of the corresponding tendon, which is quite unusual in this disease.2
We present a new clinical case and make a review of those previously published.
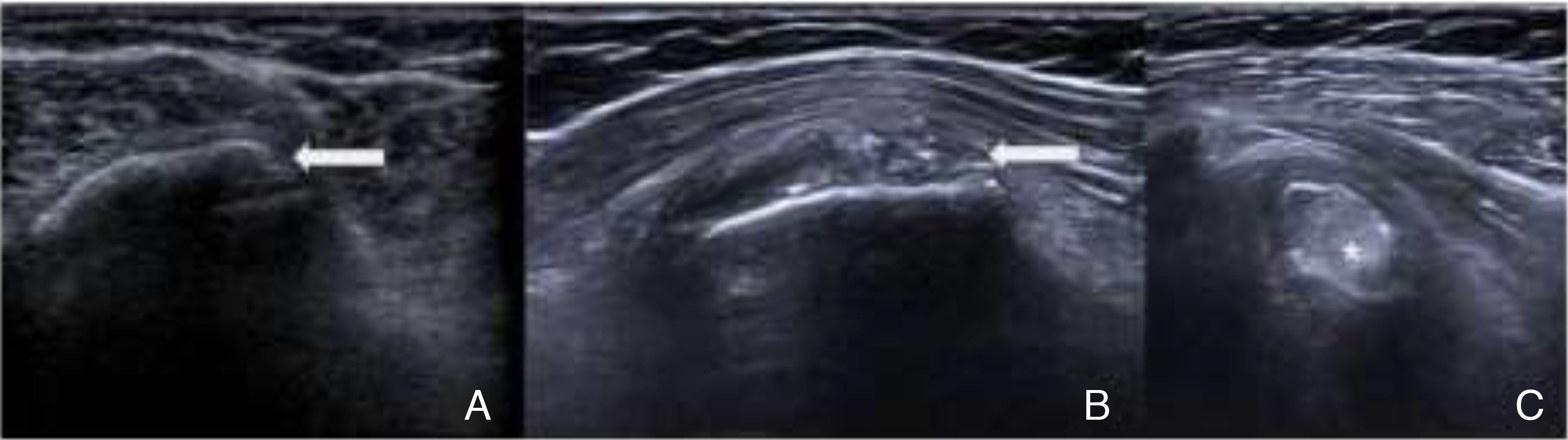
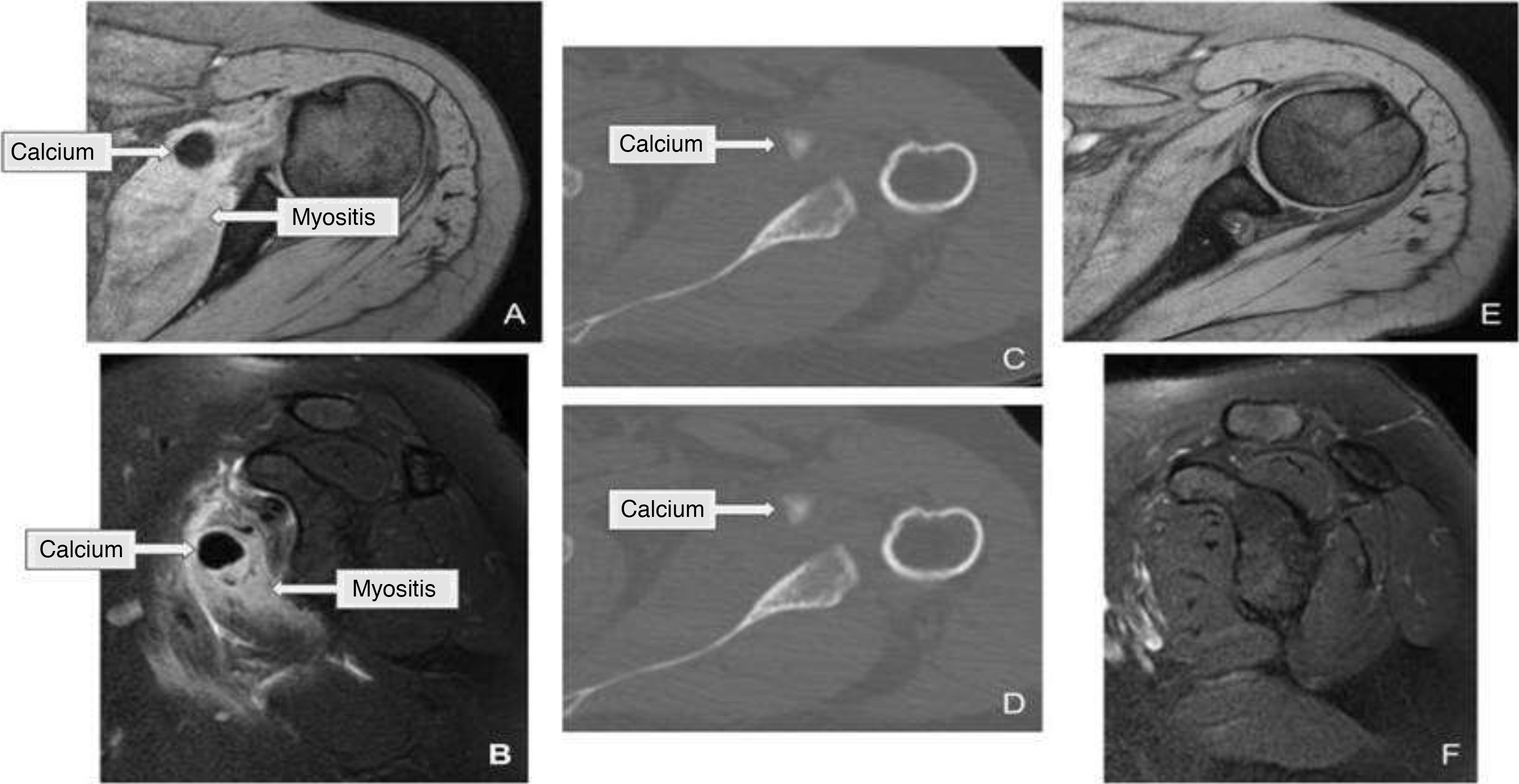
Clinical caseA 49-year-old woman with a history of right omalgia of 2 years of evolution, with functional limitation and a diagnosis of subscapular calcific tendinopathy by ultrasound (Fig. 1A). It started with a high intensity pain in the right shoulder, with limited mobility. On physical examination she presented pain that can be localized with the fingertip in the right greater tuberosity, impossibility of abduction and of anterior and posterior antepulsion, with positive Jobe and Neer provocation maneuvers. Given the history of calcific tendinopathy, calcium resorption was suspected, an ultrasound scan was performed (Fig. 1B and C) and a magnetic resonance imaging (MRI) was requested. Severe myositis in the subscapular muscle was observed in the MRI, with images of migrated calcifications inside (Fig. 2A and B), in the context of the subscapular calcific tendinopathy. The study was completed with a computed tomography (CT) for confirmation (Fig. 2C and D). The patient received analgesic and anti-inflammatory treatment, and an ultrasound-guided infiltration with betamethasone was performed. After 6 months, with the patient asymptomatic, a control MRI was performed, which was normal (Fig. 2E and F).
(A) Ultrasound scan taken 2 years ago. Arrow: calcification in the subscapularis near the insertion of the tendon; (B) Ultrasound taken in the acute moment. Arrow: the same location as in A, with some residual millimetric calcifications; (C) ultrasound in the acute moment. Asterisk: intramuscular coarse calcification, calcium in Fig. 2 images A–D.
Intratendinous deposition of hydroxyapatite crystals is a disease widely described in the literature. Louwerens et al. report a prevalence of 7.8% in asymptomatic patients and of 42.8% in patients with clinical symptoms.3
According to Uhthoff and Loehr there are 4 different phases: precalcification, formation, resting and resorption.4 In the resorption phase, the deposited calcium can migrate towards the subacromial bursa or to the bone surface of the humerus,2 being exceptional the migration towards the myotendinous junction.
Clinically, it is usually a patient with long-standing chronic omalgia who presents an atraumatic hyperalgic syndrome with great functional limitation of two weeks of evolution, with subsequent progressive improvement in most cases.
Focusing on the migration to the myotendinous junction, there is hardly any literature on this complication. In total we have found 21 cases,1,5–8 being a series of 11 patients obtained after a 7-year follow-up in different centers, published by Pereira et al. in 2016, the most extensive.1 A distinctive characteristic of our patient is the affected muscle. Of the cases that we know, only in 2 of them the affected muscle is the subscapularis.
Regarding the diagnosis, a history of calcific tendinopathy and a plain X-ray can guide us. However, to evaluate the migration towards the myotendinous junction we need more specific tests such as ultrasound, computed tomography or MRI, which allow us to visualize a more exact location of the deposits. Becciolini et al. comment on the usefulness of ultrasound for the localization of the deposits, especially taking into account the cost-benefit, in addition to the help of Power-Doppler to identify the secondary myositis.7 Pereira et al. refer that MRI is the most suitable method for the evaluation of muscle involvement, with which we can objectify the muscle edema secondary to the inflammatory response.1
Its low frequency can make us confuse it with other entities, so we must take it into account within the differential diagnosis with tumors, infections, and denervations, among others. Mileto et al., present a differential diagnosis with the Parsonage-Turner syndrome, in which the negative electromyography study and the absence of edema on the MRI at the level of other muscles innervated by the brachial plexus, ruled out such diagnosis.8
Finally, of the 21 cases that we have collected in the bibliographic references,1,5–8 14 had a subsequent follow-up, of these, 8 were successfully non-surgically treated and 6 underwent surgery due to poor clinical evolution. In 2 of the patients with nonsurgical treatment, ultrasound-guided puncture and calcium lavage were successfully performed, so we could consider it a good alternative to arthroscopy in patients with poor evolution, due to the lower risk it entails and the less associated damage in the rest of the structures.
ConclusionIntramuscular migration of hydroxyapatite is a very infrequent entity, probably related to its underdiagnosis. Future studies and research are necessary to determine the imaging test of choice, especially in terms of the corresponding cost-benefit, although according to the articles published so far, ultrasound and MRI could currently be the most accurate. Finally, regarding the treatment, we suggest that ultrasound-guided puncture can be very useful, especially in those patients with a torpid evolution.
Conflict of interestThe authors declare that they have no conflict of interest.
Please cite this article as: Mateos Rodríguez JJ, Fernández Jara J, Castro Corredor D, Gutiérrez San José B. Miositis del subescapular. Una evolución infrecuente en la tendinopatía calcificada. Estudio de un caso. Rev Colomb Reumatol. 2021;28:218–220.