Septic sacroiliitis is an unusual condition, and due to its non-specific symptoms, the diagnosis is often delayed. It should be suspected in cases in which inflammatory back pain and systemic inflammatory signs co-exist, especially in people with risk factors, such as postpartum. The case is presented of a woman, who in the late postpartum, presented with sacroiliitis and severe sepsis due to Escherichia coli. This is the second report of a case of septic sacroiliitis due to E. coli associated with pregnancy.
La sacroiliitis séptica es una condición inusual, a menudo el diagnóstico se hace de forma tardía debido a la poca especificidad de los síntomas. Debe ser sospechada en casos donde coexista dolor lumbar inflamatorio y signos de respuesta inflamatoria sistémica, especialmente en personas con factores de riesgo tales como el puerperio. En este artículo reportamos el caso de una mujer quien durante el puerperio tardío presentó sacroiliitis por Escherichia coli y sepsis grave secundaria, siendo este el segundo caso reportado de sacroiliitis séptica por Escherichia coli asociada al embarazo.
Septic sacroiliitis is an unusual condition that accounts for about 1–2% of all cases of septic arthritis.1,2 It occurs most frequently in children and young adults,3 being rarely associated with pregnancy during the periods of gestation and early postpartum (<10 days).4–9 Its diagnosis is often delayed due to the non-specificity of its symptoms and its poor localization, simulating other common conditions such as lumbar disc disease, septic arthritis of the hip, iliac osteitis, muscle spasm or visceral pain.4,10–15
This article presents the case of a woman who during the late postpartum developed sacroiliitis due to Escherichia coli (E. coli) and secondary severe sepsis; it also discusses the evidence through a systematic review of the literature and the recommendations which should be followed in similar cases.
Case reportIt is a 26-year old woman who consulted by a clinical picture of 3 days of intense pain in the lower back pain and in the right buttock, exacerbated by movements and that did not improve with rest, radiating to the right lower limb and associated with fever (38.5°C). The previous day she had consulted to the Emergency Department with a picture of similar characteristics, which was approached as a sciatic neuropathy. Seven weeks earlier, the patient had a cesarean delivery without any complications at 40 weeks of pregnancy. Two days later she underwent the implantation of an intrauterine device, without complications.
The physical examination showed an axillary temperature of 39°C, a heart rate of 95 beats per minute, a respiratory rate of 18 breaths per minute, intense pain on palpation of the right sacroiliac joint, limitation of lumbar flexoextension and positive right Lasègue's sign.
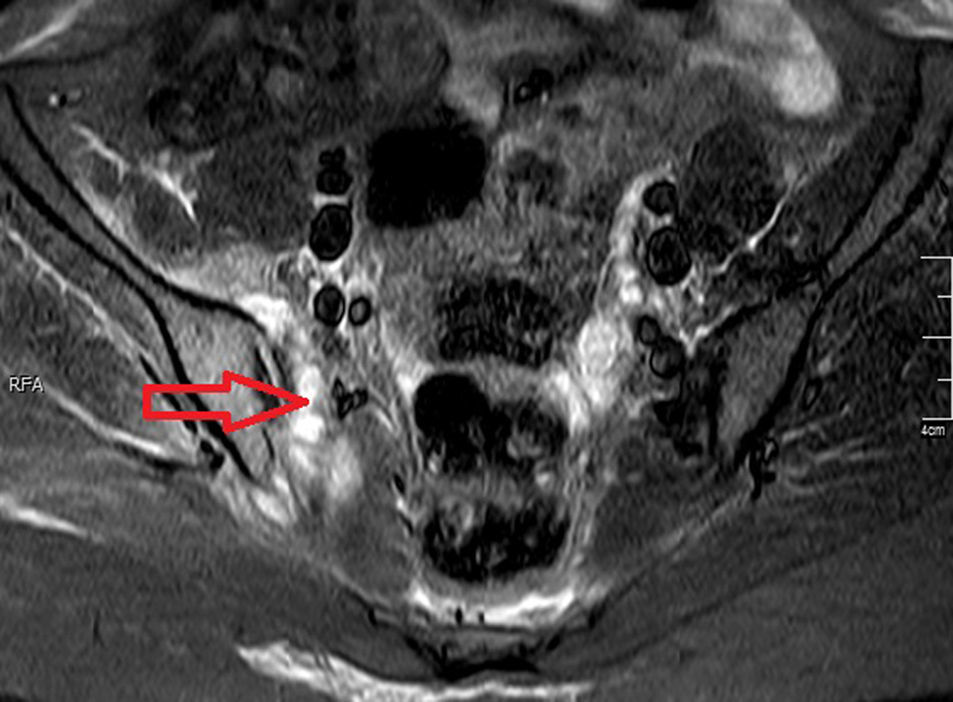
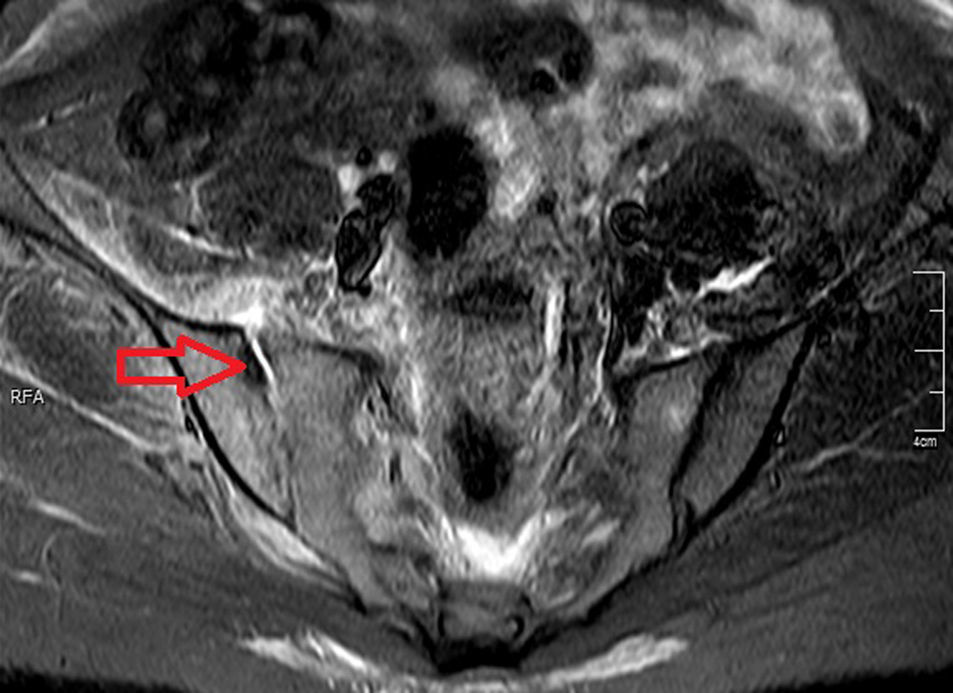
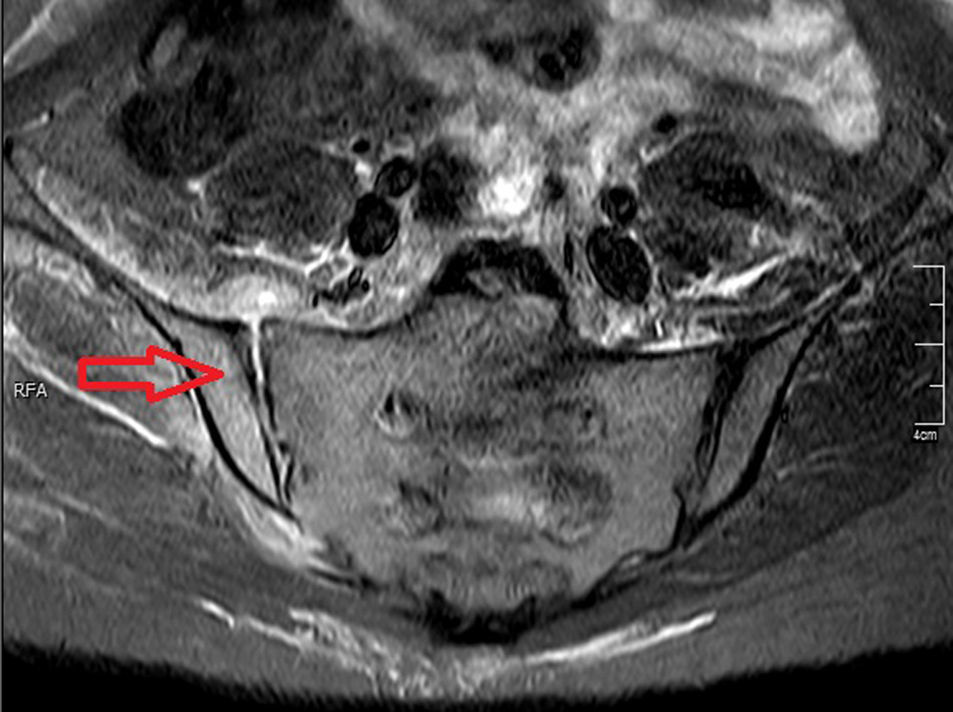
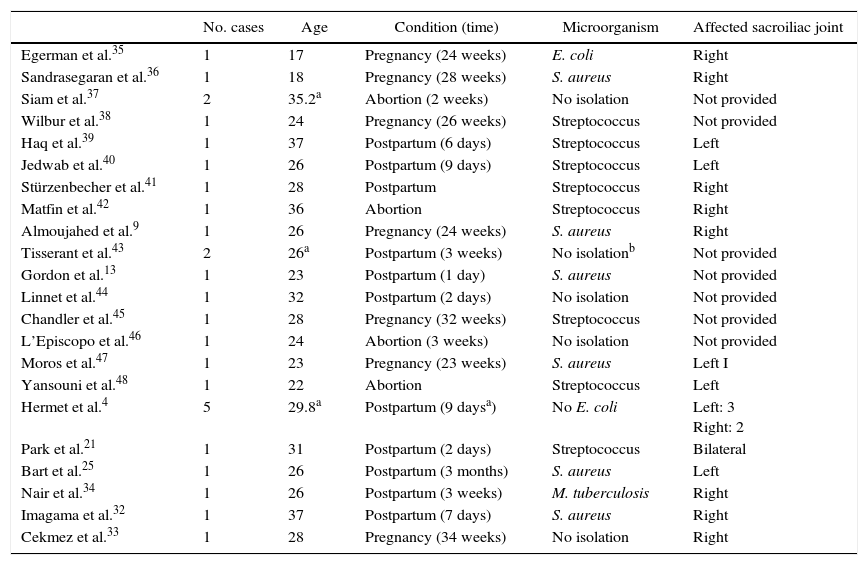
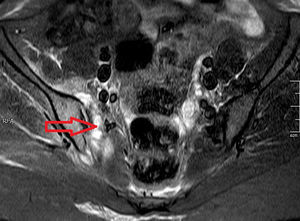
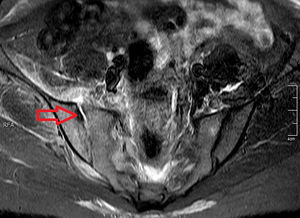
The paraclinical tests showed a blood count with leukocytosis (13,000) and neutrophilia (91%), elevation of acute phase reactants (ESR: 93mm/h, CRP: 12.5mg/dl) and a urinalysis not suggestive of infection. The antinuclear antibodies, the rheumatoid factor and HLA-B27 were negative. The bone scintigraphy with technetium 99 showed hypercaptation in the right sacroiliac joint; the nuclear magnetic resonance of sacroiliac joints revealed inflammatory changes in the periarticular soft tissues, as well as increased joint fluid, and bone marrow edema in the right iliac and sacral bones (Figs. 1–3).
With all the above, it was concluded that the patient presented a right septic sacroiliitis. Empirical intravenous antibiotic treatment with oxacillin 2g IV every 4h, was started after taking the blood cultures. The patient remained febrile and with significant pain despite the established management. Later on, the antibiotic scheme was changed to ceftriaxone because of the result of a blood culture with growth of Gram-negative bacilli.
The evolution was not favorable, since she presented a significant elevation of transaminases and developed respiratory distress, and for this reason she was transferred to the intensive care unit with a diagnosis of severe sepsis secondary to the sacroiliitis, requiring surgical drainage and debridement of the right sacroiliac joint.
Five days later the blood cultures were positive for E. coli sensitive to ciprofloxacin; whereas the synovial fluid and urine cultures where negative. Then, the antibiotic regimen for the patient was changed to ciprofloxacin 400mg IV every 12h, for 3 weeks, showing improvement of the pain, the fever and the breathing difficulty. The transaminases and acute phase reactants were gradually decreasing until they were normal. The patient was discharged to complete treatment with oral ciprofloxacin for 3 more weeks. At the end of the treatment the patient was able to walk by herself and perform her activities of daily living.
MethodologyUntil 2012, several works have grouped the largest number of clinical cases of septic sacroiliitis (excluding Mycobacteria and brucellosis) reported in the literature.2,4,5,15 In that year Hermet et al., described the largest series of cases (39 patients) on this entity.4 The above-mentioned has allowed the demographic, clinical and therapeutic characterization of this population. In order to update this series, it was conducted a systematic review of the literature of the cases of septic sacroiliitis in adults, reported between January 2012 and June 2015. The systematic search was conducted in the following databases: PubMed, SciELO and LILACS (BVS). The following MeSH terms were used: “septic sacroiliitis”, “pyogenic sacroiliitis” and “septic arthritis AND Sacroiliac Joint” without limitations of languages, populations or etiologic agents; in addition, each of the MeSH terms was translated using the Health Sciences Descriptor, a tool that contains the structured and trilingual vocabulary used in the indexing of articles in Spanish, English and Portuguese, for the purposes of the search in the BVS database. Finally, it was carried out the review of the full text of the articles found; and the references which had not been found through this search, but that might have been relevant for the study, were searched manually. The inclusion criteria for the systematic search were the following: any type of article that would contemplate septic sacroiliitis and its relationship with pregnancy and postpartum. Those articles which did not include a sacroiliitis as an outcome or that did not describe the relationship with pregnancy or postpartum, as well as the cases in the pediatric population, were excluded; as well as those articles that included the same information published by another study. Abstracts and full texts were reviewed searching for eligible articles. Two reviewers performed the search independently applying the same selection criteria, based on the PRISMA statement.16 For articles in languages other than English or Spanish, the translation of the abstract or the full text was done in order to determine their eligibility. For the extraction of data from the selected articles, the following variables were considered: average age, sex, relationship with pregnancy, affected sacroiliac joint and isolated microorganisms. Finally, the quality rating of the publications was performed using the levels established by the “Oxford Center for Evidence-based Medicine”, 2001.17
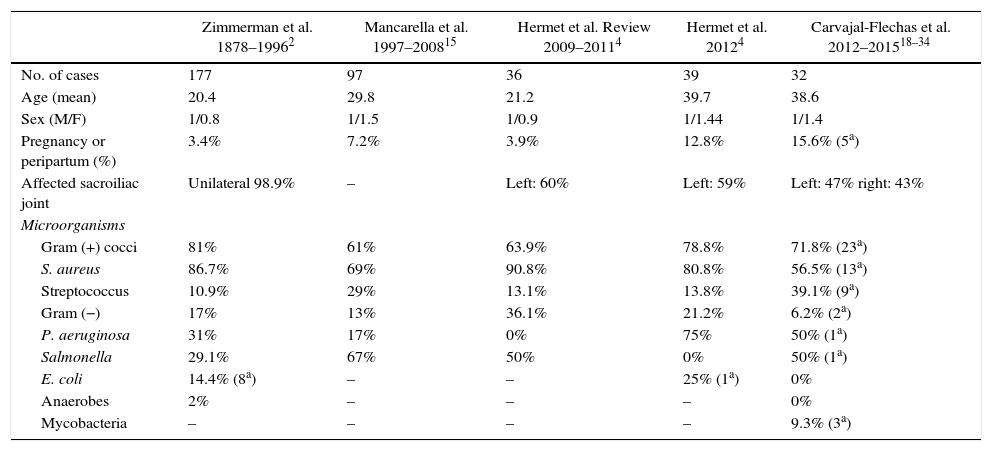
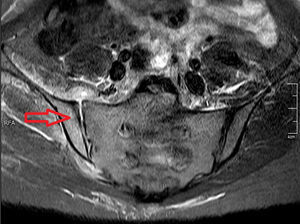
ResultsThrough the search strategy, 359 articles were identified, 341 from the Pubmed database and 18 from the BVS; of them, after applying the inclusion and exclusion criteria, 17 articles were obtained, of which 32 cases were extracted.18–34 (Table 1) In addition to all cases reported to date, those in which the infection was associated with pregnancy were extracted and analyzed (Table 2).4,9,13,21,25,32–48 All articles included were classified according to the “Oxford Center for Evidence-based Medicine” at levels 4 or 5.
Review of case reports of septic sacroiliitis.
| Zimmerman et al. 1878–19962 | Mancarella et al. 1997–200815 | Hermet et al. Review 2009–20114 | Hermet et al. 20124 | Carvajal-Flechas et al. 2012–201518–34 | |
|---|---|---|---|---|---|
| No. of cases | 177 | 97 | 36 | 39 | 32 |
| Age (mean) | 20.4 | 29.8 | 21.2 | 39.7 | 38.6 |
| Sex (M/F) | 1/0.8 | 1/1.5 | 1/0.9 | 1/1.44 | 1/1.4 |
| Pregnancy or peripartum (%) | 3.4% | 7.2% | 3.9% | 12.8% | 15.6% (5a) |
| Affected sacroiliac joint | Unilateral 98.9% | – | Left: 60% | Left: 59% | Left: 47% right: 43% |
| Microorganisms | |||||
| Gram (+) cocci | 81% | 61% | 63.9% | 78.8% | 71.8% (23a) |
| S. aureus | 86.7% | 69% | 90.8% | 80.8% | 56.5% (13a) |
| Streptococcus | 10.9% | 29% | 13.1% | 13.8% | 39.1% (9a) |
| Gram (−) | 17% | 13% | 36.1% | 21.2% | 6.2% (2a) |
| P. aeruginosa | 31% | 17% | 0% | 75% | 50% (1a) |
| Salmonella | 29.1% | 67% | 50% | 0% | 50% (1a) |
| E. coli | 14.4% (8a) | – | – | 25% (1a) | 0% |
| Anaerobes | 2% | – | – | – | 0% |
| Mycobacteria | – | – | – | – | 9.3% (3a) |
Review of case reports of septic sacroiliitis associated with pregnancy.
| No. cases | Age | Condition (time) | Microorganism | Affected sacroiliac joint | |
|---|---|---|---|---|---|
| Egerman et al.35 | 1 | 17 | Pregnancy (24 weeks) | E. coli | Right |
| Sandrasegaran et al.36 | 1 | 18 | Pregnancy (28 weeks) | S. aureus | Right |
| Siam et al.37 | 2 | 35.2a | Abortion (2 weeks) | No isolation | Not provided |
| Wilbur et al.38 | 1 | 24 | Pregnancy (26 weeks) | Streptococcus | Not provided |
| Haq et al.39 | 1 | 37 | Postpartum (6 days) | Streptococcus | Left |
| Jedwab et al.40 | 1 | 26 | Postpartum (9 days) | Streptococcus | Left |
| Stürzenbecher et al.41 | 1 | 28 | Postpartum | Streptococcus | Right |
| Matfin et al.42 | 1 | 36 | Abortion | Streptococcus | Right |
| Almoujahed et al.9 | 1 | 26 | Pregnancy (24 weeks) | S. aureus | Right |
| Tisserant et al.43 | 2 | 26a | Postpartum (3 weeks) | No isolationb | Not provided |
| Gordon et al.13 | 1 | 23 | Postpartum (1 day) | S. aureus | Not provided |
| Linnet et al.44 | 1 | 32 | Postpartum (2 days) | No isolation | Not provided |
| Chandler et al.45 | 1 | 28 | Pregnancy (32 weeks) | Streptococcus | Not provided |
| L’Episcopo et al.46 | 1 | 24 | Abortion (3 weeks) | No isolation | Not provided |
| Moros et al.47 | 1 | 23 | Pregnancy (23 weeks) | S. aureus | Left I |
| Yansouni et al.48 | 1 | 22 | Abortion | Streptococcus | Left |
| Hermet et al.4 | 5 | 29.8a | Postpartum (9 daysa) | No E. coli | Left: 3 Right: 2 |
| Park et al.21 | 1 | 31 | Postpartum (2 days) | Streptococcus | Bilateral |
| Bart et al.25 | 1 | 26 | Postpartum (3 months) | S. aureus | Left |
| Nair et al.34 | 1 | 26 | Postpartum (3 weeks) | M. tuberculosis | Right |
| Imagama et al.32 | 1 | 37 | Postpartum (7 days) | S. aureus | Right |
| Cekmez et al.33 | 1 | 28 | Pregnancy (34 weeks) | No isolation | Right |
Based on the data from this series it was found that this condition is more common in women (ratio of 1/1.4) with an average age of 39 years, being linked in 15% of cases with the status of pregnancy or peripartum. The most affected sacroiliac joint is the left (47%) and in few cases it may be bilateral. Unlike the rest of the population affected by septic sacroiliitis where Staphylococcus aureus was the most commonly isolated microorganism, in pregnancy appears to be more common the infection by Streptococcus species (27.6%). E. coli as a causal agent of septic sacroiliitis is very rare, being this the second case reported in a condition associated with pregnancy.35
As a result of the extraction of cases that occur during pregnancy, is denoted that the period most associated with the development of septic sacroiliitis is the postpartum, corresponding to 59.2% of cases, and most of them occurred in the early puerperium; with an average of 9 days postpartum in the series of Hermet et al.4
DiscussionSeptic sacroiliitis is an entity of difficult diagnosis, which is often made late, worsening its prognosis and increasing the complications rates. It usually occurs with fever of acute onset, intense pain both lumbar and gluteal, which is continuous and exacerbated with the movements. A subgroup of patients may experience a more gradual onset of the symptoms, less pain and low grade fever or absence of it.5 In most of the reported cases of septic sacroiliitis, it involves unilaterally the left sacroiliac joint (60%), but occasionally it can occur bilaterally.4,6
The infection of the sacroiliac joints seems to occur secondarily to hematogenous dissemination. The conditions that predispose to the development of a septic sacroiliitis include trauma, pregnancy, use of intravenous drugs of abuse and infections in other systems such as the skin, the genitourinary tract and the heart.2,6,47 However, in approximately 40% of cases the primary site of infection cannot be determined.2,49–51
In pregnancy the hormonal changes favor the relaxation of the pelvic joints. The sacroiliac joint capsule and ligaments are susceptible to stretching and even to tearing during childbirth; these microscopic tears could lead to synovitis or bleeding in the sacroiliac joint, resulting in intense pain. All this makes the diagnosis of septic sacroiliitis in the peripartum to be a real challenge, since this condition might be confused with physiological pelvic pain or sciatic neuropathy, which are common situations during this periods.1,6,52
Early diagnosis and treatment leads to a good prognosis, but a delayed diagnosis increases morbidity and the need for surgical interventions due to a high risk of formation of abscesses, contiguous osteomyelitis or necrotic bone sequestration.2,6
Nuclear magnetic resonance is the most appropriate imaging technique to assess the pathology of the sacroiliac joints. It can identify an increase of fluid in the joint, bone marrow edema and abscesses in the soft tissues that may extend into the pelvic cavity.53,54
Blood cultures are positive in 23–69% of cases2–5,7,15 and the cultures of the joint fluid, taken by surgical exploration or percutaneous arthrocentesis guided by axial computed tomography, are positive in 50–88% of cases.3,55
In those cases where the cause is identified, S. aureus is the most frequently isolated microorganism, followed by other Gram-positive bacteria such as Streptococcus species.1,4Pseudomona aeruginosa is the most common Gram-negative bacteria and is associated with the use of intravenous drugs, primary or secondary immunodeficiencies, chronic diseases, previous use of broad-spectrum antibiotics and invasive procedures.4,56 Other bacteria have been cultured less frequently: Salmonella, Klebsiella, E. coli, Neisseria gonorrhoeae and anaerobes.4
From the data that we extracted and analyzed in the systematic review we can deduce that streptococci are the main etiologic agent of septic sacroiliitis associated with pregnancy or peripartum. An interesting aspect of this case was the isolated germ, being this the second reported case of septic sacroiliitis caused by E. coli in a condition associated with pregnancy; as well as the development of the infectious process during the late postpartum, since in the majority of cases associated with the puerperium, it occurs in the early postpartum.
ConclusionSeptic sacroiliitis is an unusual cause of septic arthritis, even more during the period of pregnancy. In the present case we highlight that this pathology is a cause of significant morbidity, even leading the patient to sepsis; and also we support through a systematic review of the literature the main findings of the disease in the periods of pregnancy and postpartum. Although it is an infrequent form of septic arthritis, the main epidemiological, clinical and paraclinical aspects, as well as the characterization of the germ, must be taken into account for the purpose of identifying and treating these patients early and successfully.
Ethical responsibilitiesProtection of people and animalsThe authors declare that no experiments were performed on human beings or animals for this research.
Data confidentialityThe authors declare that they have followed the protocols of their workplace on the publication of patient data.
Right to privacy and informed consentThe authors have obtained the informed consent from patients and/or subjects referred in the article. This document is held in the possession of the corresponding author.
Conflict of interestThe authors declare that they have no conflict of interest.
Please cite this article as: Carvajal-Flechas F, Sarmiento-Monroy JC, Rojas-Villarraga A, Mantilla Hernández R-D. Sacroiliitis séptica por Escherichia coli en el puerperio tardío. Rev Colomb Reumatol. 2016;23:131–136.