Polyarteritis nodosa is part of the primary systemic vasculitis that specifically compromises vessels of medium caliber, and can affect virtually any organ. The diagnosis of this disease is based on clinical criteria, such as pain and weakness in the lower limbs, as well as laboratory results and the histology report that shows necrotizing, segmental and focal inflammation of the vessels involved. The case is presented of a 42 year-old woman with a previous diagnosis of polyarteritis nodosa, who, 12 years later, presented with an episode of activation of the disease associated with venous thrombosis and multifocal myopathy in the lower limbs. This is a rare presentation that should be suspected in this type of patients.
La poliarteritis nodosa hace parte de las vasculitis sistémicas primarias, específicamente compromete vasos de mediano calibre pudiendo afectar virtualmente a cualquier órgano. El diagnóstico de esta enfermedad se basa en criterios clínicos, como el dolor y la debilidad en los miembros inferiores, además de reportes paraclínicos y el compromiso histológico, que evidencia inflamación necrosante, segmentaria y focal de los vasos involucrados. A continuación, presentamos el caso clínico de una mujer de 42 años, con diagnóstico previo de poliarteritis nodosa, que presenta, 12 años después, un episodio de activación de la enfermedad asociado a trombosis venosa y miopatía multifocal en miembros inferiores, una presentación poco frecuente pero que debe sospecharse en este tipo de pacientes.
Polyarteritis nodosa (PAN) is a necrotizing primary systemic vasculitis that affects the medium-sized arteries. There may be compromise of small arteries, but small vessels such as arterioles, capillaries and venules are not affected.1,2 The exact frequency of the disease is unknown, being an uncommon condition, with multiple clinical manifestations according to the vessels involved.3
PAN may be idiopathic or associated with different agents, among which hepatitis B virus infection has been described as a frequent trigger. The pathogenesis of this disease is not very clear yet, but various immunological mechanisms involved in the development of the vasculitis have been described.3,4
The most frequent symptoms at the onset of the disease are fever, weight loss, peripheral neuropathy, arthralgias, abdominal pain, skin lesions and myalgias.5,6 Regarding the muscle involvement by the disease, it has been described that 19% of patients have myopathy associated with the vascular involvement, and musculoskeletal commitment has been histologically documented in up to 48% of cases.7,8 Below we present a case of a patient with a diagnosis of PAN and involvement by multifocal myopathy in the lower limbs adjacent to the cutaneous lesions due to the disease, highlighting the role of diagnostic images, specifically of the simple magnetic resonance imaging (MRI).
Clinical caseA 42-year-old woman from Bogota, business administrator, who consulted to the University Hospital of the Fundación Santa Fe de Bogota due to a clinical picture of 45 days of evolution, which started with skin lesions, initially violaceous, flat and nodular in the lateral side of the left leg. It was associated with edema and intense pain in lower limbs, which limit walking. Twelve years before, the patient presented a similar picture, having a histological diagnosis of PAN, for which she received immunosuppressive treatment with adequate response and remission of the disease.
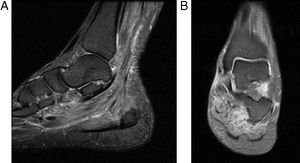
In the physical examination of admission are evident flat, nodular, violaceous and indurated skin lesions, painful to palpation and with irregular surface, located in the inner portion of the lower limbs, associated with perimalleolar edema (Fig. 1). The paraclinical tests on admission showed leukocytosis, neutrophilia, and elevation of acute phase reactants (erythrocyte sedimentation rate: 22 and C-reactive protein: 4.447). The rheumatologic autoimmune profile (antinuclear antibodies, antimyeloperoxidase, anti-proteinase 3 and rheumatoid factor) and the antibodies for hepatitis B and C were negative.
A venous Doppler ultrasound of lower limbs was performed, which showed areas with increased echogenicity of the skin and subcutaneous cellular tissue corresponding to nodular areas of PAN, one of which conditions segmental thrombosis of the right greater saphenous vein in the proximal third of the thigh and another nodular area which conditions thrombosis of the left greater saphenous vein in the middle third of the left leg. Taking into account these findings, anticoagulation with low molecular weight heparin was initiated and the analgesic management was optimized.
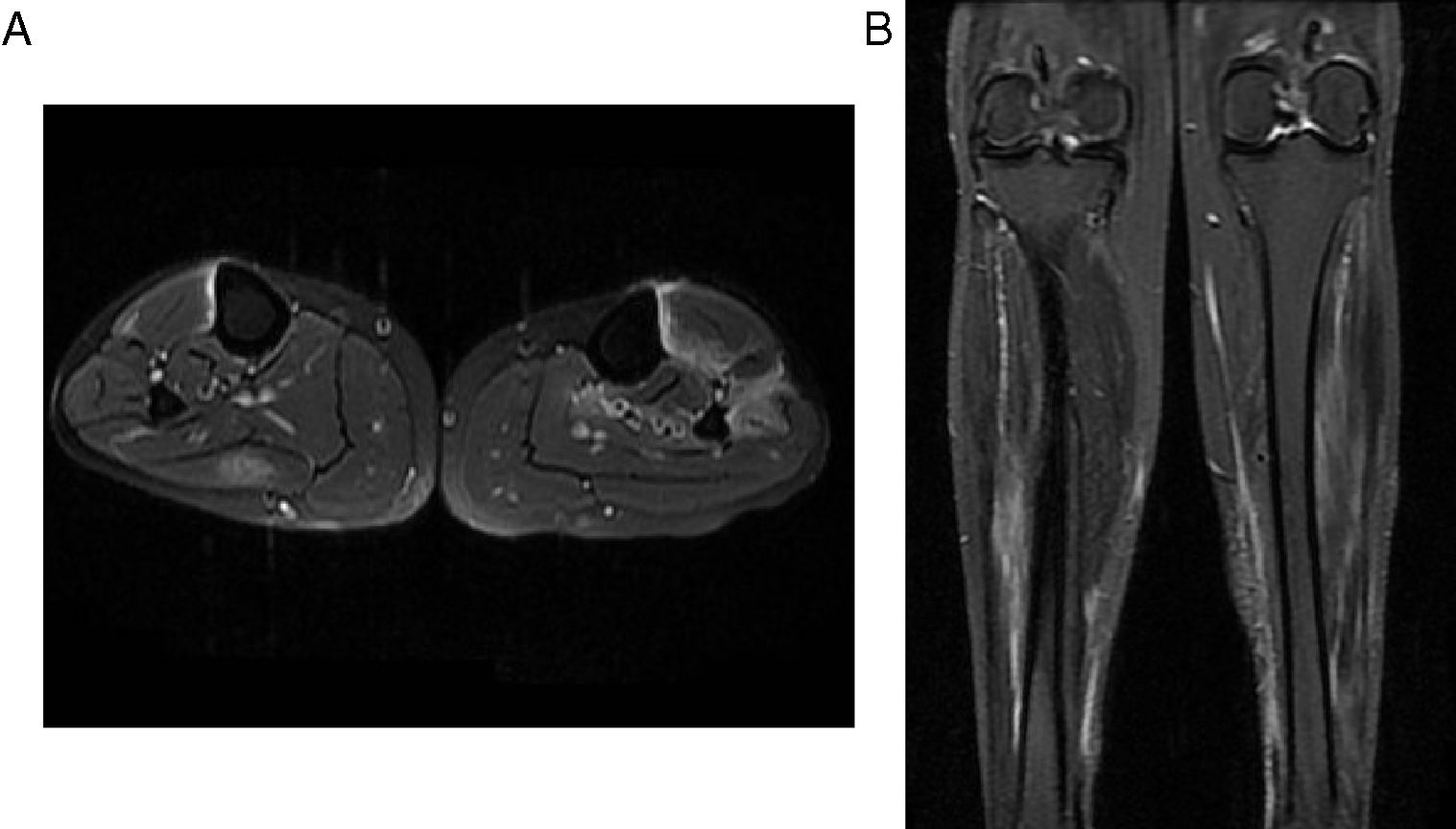
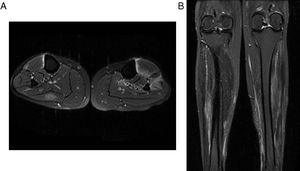
Despite the high doses of analgesics, the patient persisted with intense pain in the lower limbs and limitation of the secondary gait; it was requested a comparative MRI of lower limbs that showed multiple areas of muscle edema distributed in patches and involving the different muscle groups in both calves (Figs. 2 and 3); the findings represent a multifocal myopathy consistent with the clinical context of the patient. There was no evidence of fatty infiltration due to associated muscular atrophy.
Comparative MR images of the neck of the legs. (A) Axial PD with fat saturation. (B) Coronal PD with fat saturation. They show edema of the muscles in the posterior compartment of the right calf and of the muscles in the anterior compartment of the left calf. It should be highlighted the important degree of edema and changes of fasciitis.
With the findings in the images of the lower limbs, it was decided to progressively increase the dose of corticosteroid to 1.5mg/kg/day of prednisone associated with colchicine 0.5mg every 12h and methotrexate 15mg weekly. Additional studies were performed, including a chest X-ray, tuberculin test and Quantiferon TB Gold, which were negative and allowed to rule out the presence of tuberculosis and Bazin's indurated erythema, considered as a differential diagnosis, since at that time we had an extra-institutional inconclusive skin biopsy and not finding the characteristic lesions of a nodular vasculitis at the histological level.
The patient was discharged to complete treatment with full anticoagulation for 42 days and integral physical rehabilitation. During the follow-up by rheumatology, at 3 months after discharge the patient has not presented new skin lesions and is under management with methotrexate 15mg weekly, prednisolone 25mg daily and colchicine 0.5mg daily.
DiscussionPAN is one of the vasculitis that involves medium-sized vessels and it can affect virtually any organ, but the skin, the peripheral nervous system, the muscles, the kidneys and the gastrointestinal system are those which are usually involved.2,3,9
PAN may be idiopathic or associated with different agents, among which the infections by hepatitis B and C viruses and by the human immunodeficiency virus have been described as triggers of this vasculitis. The pathogenesis is not very clear yet, but several immunological mechanisms have been described, which explains its response to immunosuppressive treatment.3,4
Histologically, the PAN is characterized by the presence of segmental and focal necrotizing inflammation of the arteries of small and medium caliber, without glomerulonephritis and without commitment of arterioles, capillaries or venules. The inflammation of the vessels can result in the formation of microaneurysms and thrombosis. The presence of vascular compromise at different stages of the inflammatory process is typical of this disease.3,10
Regarding the diagnosis, in 1990 the American College of Rheumatology proposed some criteria that include weight loss, livedo reticularis, myalgias, weakness or pain in lower limbs, mononeuropathy or polyneuropathy, among other clinical features, in addition to laboratory parameters, such as the elevation in creatinine or urea nitrogen, alterations in the arteriography and histological changes such as those previously described.4,11
In the case we are presenting, the patient reported pain in the lower limbs and limitation for secondary gait, associated with skin lesions and malleolar edema. In addition to the diagnosis of PAN, which was made by biopsy in the first episode of the disease, commitment by multifocal myopathy in both legs was documented by magnetic resonance imaging (MRI), whose association with PAN has been described in several individual cases, but this is the first case described in our country.7,8,12–17
With respect to the radiological findings, in the MRI images it has been described increased intensity in patches or diffusely of the involved muscles in T2 or STIR sequences, which occurs secondary to edema that increases the free intracellular or extracellular water.16–18 The pathophysiology of the musculoskeletal involvement in patients with PAN may be secondary to ischemia resulting from occlusion of blood vessels, involvement of muscle fibers due to inflammation around the vessels and muscle atrophy due to damage of the peripheral nerves.8,17
The role of MRI in the determination of muscle commitment in PAN and its usefulness for follow-up is still discussed; however, it is indicated that this imaging study may be useful to assess the muscle commitment secondary to the disease and rule out other conditions that explain the muscle involvement in case that they are associated with atrophy or other concomitant alterations.14–17 In the case of our patient, as shown in the MRI images, the increased enhancement of the muscle fascia and the muscle edema were not associated with chronic alterations, such as the presence of muscular atrophy or fatty infiltration that would indicate other differential diagnoses in this patient.
The main restriction of MRI in the diagnosis of PAN is that the histopathological changes of this disease can be found in other entities, such as inflammatory myopathies, myositis, infections and compartment syndrome. This is why the diagnosis of this vascular involvement should not be based only on the imaging findings, but it requires confirmation by biopsy.17
Regarding the usefulness of MRI in the follow-up of patients with PAN in its active phase, it is useful given that the imaging characteristics correlate with the clinical evolution of the patient, taking into account that with treatment not only should be observed a decrease in edema, pain and skin involvement, but also a decrease in the commitment of the fascia and muscle that allows the patient to improve his functionality that was compromised by the activity of the disease.14,16,19
Taking into account the information of the cases reported in this type of muscle compromise secondary to PAN and in cases of other vasculitis, the performance of images such as MRI allows to select the best site for taking the biopsy sample that will confirm the diagnostic suspicion and, therefore, increases the diagnostic performance by taking into consideration the findings of involvement of muscle and soft tissue in the T2 and STIR sequence of this imaging study.8,14,16,17,19,20 In addition, MRI can be useful to monitor the therapeutic response in inflammatory diseases, and not only in PAN.20,21
ConclusionsPAN is an autoimmune condition, rare in our environment, which mainly involves medium-sized vessels with evidence of cutaneous, nervous, renal, and gastrointestinal involvement and, in some cases, is accompanied by focal or diffuse myopathy in the context of a systemic disease. The diagnosis of muscular involvement by means of images such as MRI allows to rule out other associated conditions and could be useful to improve the diagnostic performance of the biopsies necessary for diagnostic confirmation and for the follow-up of the disease activity and the response to treatment.
Conflict of interestNone.
Please cite this article as: Prada LP, García FA, Páez HD, Méndez PA, Quintana G, Coral PX. Miopatía multifocal en paciente con poliarteritis nodosa: utilidad de la resonancia nuclear magnética como prueba diagnóstica. Rev Colomb Reumatol. 2019;26:63–67.