Anti-N-methyl-d-Aspartate receptor (NMDAr) encephalitis is a recently described clinical entity with an increasing number of reported cases. Psychiatric symptoms in the early stages of the disease constitute a diagnostic challenge for the treating physician. We present two clinical cases: clinical case 1, a 26-year-old man, and clinical case 2, an 18-year-old man; both presented with a first episode of psychosis and were hospitalized as psychiatric disorders. Subsequently, both cases were diagnosed as anti-NMDAr encephalitis. The high prevalence of psychiatric symptoms in anti-NMDAr encephalitis forces psychiatrists and neurologists to have a high degree of suspicion in the presence of atypical symptoms in patients evaluated for the first episode of psychosis.
La encefalitis asociada a anticuerpos contra el receptor de N-metil-D-Aspartato (NMDAr) es una entidad clínica recientemente descrita con un número creciente de casos reportados. Los síntomas psiquiátricos en etapas tempranas de la enfermedad conforman un reto diagnóstico para el médico tratante. Presentamos dos casos clínicos: el caso clínico 1, un hombre de 26 años y el caso clínico 2, un joven de 18 años, ambos abordados como primer episodio de psicosis y hospitalizados en instituciones psiquiátricas. Posteriormente, ambos casos fueron diagnosticados como encefalitis anti-NMDAr. La alta prevalencia de síntomas psiquiátricos en la encefalis anti-NMDAr demanda a los médicos psiquiatras y neurólogos a tener un alto índice de sospecha en presencia de síntomas atípicos en pacientes evaluados por primer episodio de psicosis.
N-methyl-d-aspartate (NMDA) receptor antibody encephalitis is a recently described clinical condition,1 with a growing number of reported cases which is indicative of its epidemiological importance.2 In it, IgG antibodies are expressed against the NR1 subunit of the NMDA receptor (NMDAr), leading to the onset of complex neuropsychiatric symptoms.3 During the first month of illness, 90% of patients suffer at least four symptoms from the characteristic clinical groups: behavioural alterations or cognitive dysfunction, speech disorders, epileptic seizures, movement disorders, deteriorating state of consciousness, autonomic symptoms and hypoventilation.4 However, psychiatric symptoms dominate in the early stages, which can lead this disease to be confused with primary psychiatric disorders, delaying treatment and leading to serious consequences for patients.5
Although anti-NMDAr encephalitis has been described in young women as a paraneoplastic syndrome associated with ovarian teratoma, it is now known that it also occurs in men and children, with and without evidence of associated neoplasms.6 In spite of the seriousness of this disease, more than 75% of patients achieve a substantial recovery with prompt and adequate treatment; early detection is therefore essential.3
Case report 1A 26-year-old male patient, with no history of significance, consulted due to a clinical picture of holocranial headache, tinnitus, dizziness and behavioural changes which had been ongoing for one month. The headache episodes were accompanied by difficulty holding a conversation. In the first week he suffered an episode of disorientation and fixed gaze lasting one minute. Two weeks later, the patient was observed to be confused, inattentive and irritable, with delirious ideas of damage and harm. He had no flu-like symptoms or fever prior to the onset of the illness.
It was treated as a first episode of psychosis. Both the simple cranial tomography and lumbar puncture (LP) were normal. In the psychiatric hospital, he presented catatonic symptoms, and nine days later suffered a generalised tonic–clonic seizure (GTCS) which alerted physicians to the fact that there could be an underlying neurological syndrome.
In our neurology department, the possibility of encephalitis was discussed and empirical treatment with aciclovir was started. Magnetic resonance imaging of the brain and a second LP were normal. Nevertheless, the electroencephalogram (EEG) showed severe generalised dysfunction with extreme delta brush. Suspecting autoimmune encephalitis, immunotherapy was started. Later on, anti-NMDAr antibodies were confirmed to be positive in cerebrospinal fluid (CSF).
Case report 2An 18-year-old male patient consulted due to a clinical picture of insomnia, soliloquy, unmotivated laughter, suspicion, and aggressiveness which had been ongoing for eight days. He had a history of problematic use of inhalers and benzodiazepines, suspended three months earlier. His studies, including cranial tomography and LP, were normal. He had no flu-like symptoms or fever prior to the onset of the illness.
It was treated as substance-induced psychosis and the patient was referred to inpatient psychiatric care, where he started treatment with risperidone and clonazepam. Four days later, he presented postures maintained for long periods and a GTCS lasting 2min, and was therefore referred to our neurology department.
This time, the EEG revealed severe generalised dysfunction with no epileptic activity; magnetic resonance imaging of the brain was normal. He was initially treated with aciclovir. After ruling out a viral aetiology, and suspecting autoimmune encephalitis, immunotherapy was started. Later on, anti-NMDAr antibodies were confirmed to be positive in CSF.
DiscussionThe discovery of anti-NMDAr encephalitis has changed the diagnostic approach to patients presenting at medical departments with psychotic symptoms.3 The predominance of psychiatric symptoms in the early stages of the disease means that 75% of patients are initially treated by psychiatrists: epileptic seizures and dyskinesia are the cardinal symptoms that often herald the possibility of an underlying neurological disease,3 as is demonstrated in the cases reported here. However, Kayser et al. indicate that approximately 4% of cases of anti-NMDAr encephalitis can present with psychiatric symptoms with no other neurological impairment,7 making diagnosis even more difficult.
Currently, no guidelines recommend looking for anti-NMDAr antibodies in studies of patients with a first psychotic episode. Nevertheless, some authors have recommended testing for them in that clinical context. For example, Lennox et al. recommend measuring anti-NMDAr antibodies in all individuals with a first psychotic episode,9 while Steiner et al. make this recommendation only for young women with disorganised and/or catatonic symptoms with an acute onset.10 More recently, Maneta et al. proposed key factors to consider the possibility of anti-NMDAr encephalitis in a first episode of psychosis: prodromal flu-like symptoms, psychosis and catatonia of sudden onset, female sex, presence of epileptic seizures or other neurological dysfunctions, presence of malignancy, severe autonomic manifestations and worsening of symptoms with the use of antipsychotics.5 The emphasis on women is in keeping with the predominance of female sufferers of this disease; however, diagnosis in men is increasing in frequency, reaching 32% of cases in recent systematic reviews.2 Other imitators reported in cases of anti-NMDAr encephalitis are delirium and dissociative disorders.11–13
Some of the available diagnostic studies support, but do not exclude, the probability of a diagnosis of anti-NMDAr encephalitis and must be requested for patients in whom this disease in suspected (Table 1). CSF is abnormal in 80% of patients at the onset of the disease and around 90% in later stages.3 However, in the recent systematic review by Zhang et al. only 58% of patients presented abnormalities in CSF.2 The EEG showed changes in 85–90% of patients, including nonspecific patterns of generalised dysfunction and focal epileptic activity.3 The characteristic so-called “extreme delta brush” pattern is present in only 30% of cases.14 On the other hand, magnetic resonance imaging of the brain can be abnormal in 50% of subjects, with a unilateral or bilateral increase in T2-FLAIR signal intensity in the medial temporal lobes.3 Therefore, although the definitive diagnosis of this disease is made on detection of anti-NMDAr antibodies in CSF,4,15 conventional clinical and standard paraclinical assessments allow immunotherapy to be initiated early.4
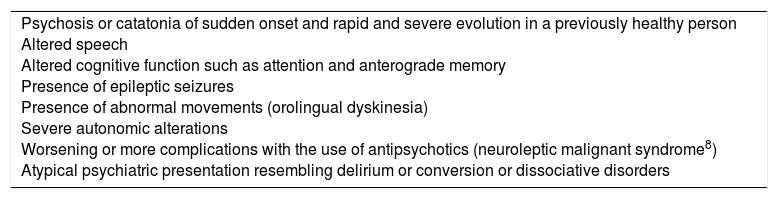
Red flags for suspecting anti-NMDAr encephalitis in a first psychotic episode.
| Psychosis or catatonia of sudden onset and rapid and severe evolution in a previously healthy person Altered speech Altered cognitive function such as attention and anterograde memory Presence of epileptic seizures Presence of abnormal movements (orolingual dyskinesia) Severe autonomic alterations Worsening or more complications with the use of antipsychotics (neuroleptic malignant syndrome8) Atypical psychiatric presentation resembling delirium or conversion or dissociative disorders |
To conclude, anti-NMDAr encephalitis should be considered as a differential diagnosis in patients with a first psychotic episode. Its recognition is highly relevant, as prompt diagnosis and treatment are associated with more favourable outcomes. The clinical red flags proposed are grounds to suspect the disease in patients consulting with psychotic symptoms, helping psychiatrists, neurologists and other physicians to play a significant role in the early diagnosis of this condition.
Ethical disclosuresNone.
Conflicts of interestThe authors have no conflicts of interest to declare.
Please cite this article as: Restrepo Martínez M, Bautista GP, Espínola-Nadurille M, Bayliss L. Banderas rojas para sospechar encefalitis anti-NMDAr en un primer episodio psicótico: reporte de dos casos. Rev Colomb Psiquiat. 2019;48:127–130.