Isotretinoin is a member of the retinoid family of drugs, and has been used for the treatment of severe acne. Its use has been associated with various psychiatric and behavioural symptoms.
MethodologyA case report and a non-systematic review of the literature are presented.
ResultsThe case concerns a 13 year-old adolescent with insomnia, delusions, and auditory hallucinations, after two months of treatment with isotretinoin. The patient was admitted to hospital, where the use of psychoactive drugs and systemic disease that could explain the psychotic symptoms are ruled out. After two weeks of stopping the isotretinoin and starting with treatment with olanzapine 10mg per day, there was complete remission of the psychotic symptoms.
DiscussionOn the onset of psychotic symptoms in an adolescent with no prior personal or family history of mental illness, the diagnosis of a secondary psychosis needs to be considered.
ConclusionClinicians would benefit from knowing the psychiatric symptoms that could be associated with the use of this drug, as well as its suspension and specific treatment for emerging psychotic illness.
La Isotreitonina, un medicamento de la familia de los retinoides ha sido utilizada para el tratamiento del acné severo. Su uso ha sido asociado con diversos síntomas psiquiátricos de tipo afectivo, psicótico y comportamental.
MetodologíaReporte de caso y revisión no sistemática de la literatura relevante.
ResultadosHombre adolescente de 13 años con insomnio, ideas delirantes, alucinaciones auditivas, luego de dos meses de tratamiento con isotretinoina. El paciente es hospitalizado, se descartó el consumo de drogas psicoactivas y enfermedad sistémica que explicaran los síntomas psicóticos. Luego de dos semanas de suspender la isotretinoina y recibir tratamiento con olanzapina 10mg al día remitieron los síntomas psicóticos.
DiscusiónEl inicio de síntomas psicóticos en un adolescente sin antecedentes personales ni familiares de enfermedad mental exige considerar el diagnósitico de psicosis secundaria. Los clínicos se benefician de conocer los síntomas psiquiátricos que se pueden asociar con este medicamento, considerar la suspensión y el tratamiento específico para la psicopatología emergente.
Acne vulgaris is a common skin disease that affects 85% of adolescents. The most commonly reported psychological symptoms suffered by patients with acne are related to anxiety, depression and suicidal ideation.1
Among the therapeutic options for severe acne is isotretinoin, a 13-cis–trans isomer of retinoic acid.2 Retinoids are a family of compounds that include vitamin A, its derivatives and chemically related synthetic molecules. The therapeutic effect of isotretinoin is mediated by three mechanisms: (a) reduction in the function of the sebaceous glands; (b) inhibition of the formation of new comedones, and (c) inhibition of growth of Propionibacterium acnes.3
Although isotretinoin is indicated only for the treatment of severe cases of acne, it is often used in mild and moderate cases.4 Isotretinoin was first introduced on the market in 1982, and the following year Hazen et al.5 published a series of 24 cases of depression related to the use of the drug. Initially reports of cases with psychiatric symptoms appeared to be “anecdotal” or an idiosyncratic reaction to the drug, until in 1998 the Food and Drug Administration (FDA) demanded that the laboratory that developed the original isotretinoin molecule insert a warning on the pack containing the product: “Isotretinoin psychiatric disorders. Can cause depression, psychosis and rarely suicidal ideation, suicide attempts and suicide. Discontinuation of this drug as therapy may be insufficient, and further evaluation may be necessary”.
Subsequently there were some cases of suicide which were widely publicised in the United States and prompted a debate in the US Congress. As a result of this, the following warning was added to the product warning label: “Its use may be associated with aggressive and/or violent behaviour”. Later, in 2002, the American Academy of Dermatology convened a panel of experts who concluded that epidemiological studies at that time did not show an association between isotretinoin and depression and suicide, because acne per se may be a risk factor for depression. The panel also pointed out that there was insufficient scientific evidence on the effects of retinoids on adult brain function. From 1982 to 2002, the FDA's Adverse Event Reporting System (AERS) received 3104 reports of psychiatric adverse events attributed to the use of isotretinoin, including 173 suicides.6
The aim of this article is to present the case of an adolescent male who presented with a first psychotic episode associated with the use of isotretinoin for acne. Although the scientific evidence from the past 20 years on the adverse psychiatric effects of isotretinoin in the affective sphere are well documented, mainly depression and suicidal ideation, to date there have been very few cases of psychosis related to this drug.
Description of the caseA 13-year-old adolescent male living in an urban area of Medellín whose parents took him to the Accident and Emergency with a 5-day history of delusional paranoid ideas (“Everyone's trying to hurt me”), hallucinations (“Someone's talking to me from behind the curtains”), suspicious attitude, irritable affect, motor restlessness, difficulty falling and staying asleep, poor appetite and family and social withdrawal. During that period there had been no passive experiences, false acknowledgements, alterations of the form or the course of his thought or affective depressive or manic symptoms. At the time of the consultation the patient lived with both parents, was in the normal year of schooling for his age, with good academic performance and no disciplinary problems and regularly played tennis. His parents described him as sociable, extroverted, calm and responsible. He had no previous psychiatric history.
As significant previous medical history, he had slight head injury at the age of 11; a simple brain CT was normal, with no transient or permanent neurological deficit, and he did not require hospitalisation, surgery or subsequent medical follow-up. The family reported that there was no consumption of toxic substances, and rapid tests in urine were negative in the A&E. For the previous 2 months he had been taking isotretinoin 20mg/day prescribed by dermatology for the treatment of nodular acne on his face and back. There was no family history of mental illness.
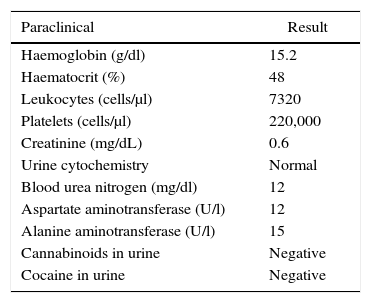
On admission to hospital, laboratory tests were requested (Table 1). Treatment was started with oral haloperidol 2mg/night. Isotretinoin was discontinued and the patient was referred for admission to psychiatric hospital.
Paraclinical results in the A&E.
| Paraclinical | Result |
|---|---|
| Haemoglobin (g/dl) | 15.2 |
| Haematocrit (%) | 48 |
| Leukocytes (cells/μl) | 7320 |
| Platelets (cells/μl) | 220,000 |
| Creatinine (mg/dL) | 0.6 |
| Urine cytochemistry | Normal |
| Blood urea nitrogen (mg/dl) | 12 |
| Aspartate aminotransferase (U/l) | 12 |
| Alanine aminotransferase (U/l) | 15 |
| Cannabinoids in urine | Negative |
| Cocaine in urine | Negative |
During the first unstructured psychiatric interview, the patient was alert, oriented to person, place and time, normal attention, with poor eye contact with the interviewer, restricted affect, language not altered in form and with appropriate tone, with delusional paranoid ideas of injury and harm (“I’m being chased for my family's car licence plate”, “My dad gave them the order to kill me … you’re going to kill me”) and auditory hallucinations (“I can hear them calling me and threatening me”, “They’re telling me it's all my dad's fault, for covering the car plate”).
In addition, during the first psychiatric assessment a painful muscle contracture was observed in the cervical region, described as acute dystonia associated with the use of haloperidol, for which the drug was discontinued and he was started on treatment with olanzapine 5mg/day orally. With these clinical findings, a first psychotic episode was diagnosed and it was decided to admit the patient to hospital.
After 8 days of treatment, the olanzapine was increased to 10mg/night orally. Thereafter improvement in behaviour was observed: better integration with the patient group and greater affective resonance. Progressively the delusional ideas were disrupted, the wake–sleep cycle was regulated and the suspicious attitude disappeared. During the psychiatric interviews no obsessive or anxious symptoms or dysfunctional personality traits were identified.
After 2 weeks in hospital, the patient was free of psychotic and euthymic symptoms. His family found him to have fully recovered, so it was decided to discharge him. Due to administrative problems of his health insurer, it was not possible to perform a brain CT scan or electroencephalogram during the hospital stay. The patient was assessed a month later as an outpatient; he said he felt well, and he had resumed his school and sports activities. He had no difficulties in interacting with peers, friends and family. He was continuing with the olanzapine with no adverse effects. Following an assessment by dermatology, it was decided not to restart the retinoid, but to start other topical therapies for the patient's acne. In view of the complete resolution of the symptoms, the pending investigations were not subsequently requested.
Diagnostic approachFrom the psychopathological point of view, the symptoms presented by the patient were psychotic. Psychosis may present as a symptom or as a syndrome. Of these, the patient had paranoid delusions, auditory hallucinations and disorganised behaviour. No affective symptoms were detected that would have led us to suspect a mood disorder, and the diagnostic criteria for the other diagnostic categories that can manifest themselves with psychotic symptoms were not met.
Psychotic disorders are characterised by different symptomatic domains, each with different courses, patterns of response to treatment and prognostic implications.7 The fifth edition of the Diagnostic and Statistical Manual (DSM-5) includes the category “Schizophrenia spectrum and other psychotic disorders”, and to that may be added the course specifier “first episode”, which applies to the patient described here.
The prevalence of psychosis in young people is 1% in population studies and 4–8% in selected samples.8,9 Social and school problems, distrust, insomnia and motor impairment have been described as premorbid symptoms in schizophrenia.10–13 None of these symptoms had been identified in the patient prior to the onset of psychosis.
Other demographic and clinical factors have been associated with the early onset of “primary” psychotic disorders. These include a family history of psychotic disorders, obstetric complications and the use of cannabis,14 none of which applied to the patient.
Acute psychotic episodes with short duration and complete remission, like the case presented here, have been of great interest to psychiatry since Kraepelin's era. Before classifying psychotic symptoms it is necessary to rule out “organicity” or that the symptoms are the side effect of a drug or a toxic substance. In cases where it is possible to demonstrate psychosis as a consequence of a systemic disease or side effect of a drug or toxic substance, it is called “organic psychosis”.
However, in the case of organic psychoses, delusional disorders and manias secondary to neurological or toxic-metabolic diseases are indistinguishable from functional or primary psychoses.15 Among the most common diseases in this age group that may explain the symptoms are acute porphyria, urea cycle disorders, disorders of homocysteine metabolism and Wilson's disease. In the patient presented here, no other symptoms or signs were observed to cause this type of problem to be suspected.
Another possible explanation for the psychosis in this patient is an adverse drug reaction (ADR), in this case to isotretinoin. To establish a causal relationship between the use of a drug and psychotic symptoms, the causality criteria proposed by Bradford-Hill can be verified16: (a) temporality: the use of the medication precedes the appearance of psychotic symptoms; (b) consistency: similar clinical situations of psychotic symptoms associated with isotretinoin use have been described; (c) dose–response (biological gradient): the higher the dose of isotretinoin, the greater the possibility of psychiatric symptoms, in this case psychosis; (d) reversibility: isotretinoin exposure is discontinued and symptoms disappear; (e) specificity: the use of isotretinoin is associated “specifically” with the appearance of psychotic symptoms; (f) analogy: a similar exposure provides the known effect, and (g) biological plausibility: the cause–effect relationship between isotretinoin and the onset of psychosis can be explained biologically.
In this case, the following criteria were met to support the causal relationship between isotretinoin and the psychotic episode in this patient:
- 1.
Temporality: the patient had not had any psychotic symptoms before starting treatment with isotretinoin.
- 2.
Reversibility: the symptoms disappeared after discontinuation of isotretinoin, although antipsychotic treatment was also given, and for obvious reasons, the patient did not go back to isotretinoin therapy to verify the recurrence of symptoms.
- 3.
Consistency: associated and reported psychiatric symptoms since isotretinoin came on the market are countable.
- 4.
Specificity and analogy met: A case reported by Rajagopal17 shows similarities with the case described here (age, rapid onset of psychotic symptoms after starting isotretinoin, type of hallucinations, and rapid improvement after discontinuing medication). Barak et al.18 reported 5 young soldiers on treatment for severe acne in a specialised dermatology clinic who developed manic psychosis after an average of 7.6 months of exposure to isotretinoin. Three of these cases also attempted suicide and in 3 cases the psychosis lasted more than 6 months. In all of them, previous psychiatric morbidity was ruled out. The main reports of psychopathology associated with isotretinoin are of the depressive and suicidal type, although the studies are insufficient to establish a causal association.19 Decompensation was reported in 1 patient with bipolar affective disorder.20 Other studies show the positive effect of isotretinoin in improving anxious, depressive and obsessive symptoms when the acne lesions improve.21
- 5.
Biological plausibility: met. Retinoids are known to have a direct effect on the central nervous system, which may explain the neuropsychiatric symptoms. To understand the mechanisms that mediate the association between isotretinoin and psychosis, we need to start with the psychoneurobiological effects associated with this drug.
The psychiatric side effects may be related to the important role that retinoids play in signalling processes in the brain that regulate gene expression and control neuronal differentiation in the nervous system.
The physiological actions of retinoids are mediated by retinoic acid receptors, which belong to the steroid/thyroid receptor superfamily. Three subtypes of retinoic acid receptors (RAR) have been discovered: alpha, beta and gamma.22,23 The most studied RAR in the human central nervous system is the alpha receptor, which has shown a broad pattern of distribution in the hypothalamus, with high density in various brain nuclei: suprachiasmatic, paraventricular, supraoptic, infundibular and medial mammillary. In addition, these receptors have been found “colocalised” with vasopressin and corticotropin-releasing neurons, which provides a possible neurobiological basis for the involvement of retinoids in the regulation of various hypothalamic functions and opens up the possibility that these drugs modulate the hypothalamic–pituitary–adrenal axis, which regulates the response to stress and is associated with numerous psychiatric disorders.24
Of the causality criteria presented, four have greater causal weight: (a) existence of association; (b) biological plausibility; (c) adequate temporal presence, and (d) the association cannot be explained entirely by other factors.25 In the case reported, the first three criteria are met.
ConclusionsDetermining causal relationships in health is a highly complex process. However, the numerous reports of psychopathology associated with the use of isotretinoin support this association. The clinician must therefore check for psychiatric symptoms before and during treatment with isotretinoin, and consider discontinuing the drug and providing early and appropriate treatment for the emerging mental disorder.
Ethical disclosuresProtection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of dataThe authors declare that they have followed the protocols of their work centre on the publication of patient data.
Right to privacy and informed consentThe authors have obtained the written informed consent of the patients or subjects mentioned in the article. The corresponding author is in possession of this document.
Conflicts of interestThe authors have no conflicts of interest to declare.
The authors of the article would like to thank Hospital Mental de Antioquia for providing space for patient care.
Please cite this article as: Valderrama F, Gómez A, Restrepo D. Primer episodio psicótico en adolescente con acné vulgar y tratamiento con isotretinoína. Rev Colomb Psiquiat. 2017;46:50–54.