Depression is the main cause of years lossed due to disability in the world, and it affects 50% more women 50% than men. Perinatal depression has been linked with more anxiety, a chronic course, and disability than depression in other life stages. In spite of its high prevalence and serious health effects on both mother and foetus, it is frequently under-diagnosed. This study was performed on all high risk obstetric patients admitted to a critical care obstetric unit in Cali, Colombia, from January to June, 2014. Depressive symptoms and psychosocial risk factors were screened by means of a survey and the Edinburgh Prenatal Depression Scale (EPDS). A total of 695 women were included, of whom 30.2% had depressive symptoms on the EPDS, and 3.6% reported having self-injury thoughts in the last 7 days. Our findings are consistent with previous reports on a history of child abuse and family depression as risk factors. It was also suggested that lower socio-economic status is associated with more vulnerability. Early screening is needed to ensure timely detection and treatment.
La depresión es la principal causa de años perdidos por discapacidad en el mundo, y en mujeres la carga de la enfermedad es un 50% mayor que en varones. La depresión perinatal tiene mayor asociación con ansiedad, cronicidad y discapacidad que en otras etapas de la vida y es poco reconocida a pesar de su alta prevalencia y sus graves efectos en la salud de la madre y el feto. Se realizó un estudio en pacientes ingresadas y valoradas en una unidad de alto riesgo obstétrico en el proceso de implementación del programa durante los meses de enero a junio de 2014; se utilizaron la Edinburgh Prenatal Depression Scale (EPDS) y un cuestionario previamente desarrollado para identificar la presencia de síntomas depresivos y factores de riesgo psicosocial. Se evaluó sistemáticamente a más de 600 mujeres, y se encontró que el 30,2% de las mujeres evaluadas tenían síntomas depresivos según la EPDS y el 3,6% había tenido ideas de autolesión en los últimos 7 días. Los factores relacionados evaluados indican una condición de vulnerabilidad de las mujeres con menor nivel socioeconómico. Los datos encontrados reiteran la importancia de detectar factores que tradicionalmente el personal de salud no identifica ni interviene a lo largo de la vida y particularmente durante la gestación.
Depression is the most prevalent mental illness and the leading cause of disability-adjusted life years worldwide.1 Depression is twice as prevalent among women than men. Prevalence peaks during reproductive age, the clinical course varies greatly, and there is a high risk of recurrence.
Perinatal depression is defined as an episode of major depressive disorder occurring either during pregnancy or within the first 12 months postpartum; it is more closely associated with anxiety, chronicity and disability than depression in other stages of life.2–4
Prenatal depression in particular, despite its high prevalence and serious effects on the health of the mother and the foetus, is a poorly recognised clinical entity. It increases the risk of both adverse perinatal outcomes and alterations in the development and health of the foetus until adulthood.5–13 Likewise, depression during pregnancy is the main predictor of postpartum depression and life-long recurrence of depressive episodes in women.14,15
Prenatal depression is a risk factor for miscarriage, preeclampsia, preterm birth and low birth weight. It is also a risk factor for the child's health, and is associated with delayed psychomotor development, child abuse, depression, attention and behavioural disorders, dissocial disorder and poor academic performance.16–26
In Latin America, the prevalence of depression during pregnancy is estimated to be between 17.4% and 40.1%.27–29 In Colombia, estimates suggest that 32.8% of pregnant adolescents suffer from depression.30
Studies have identified a series of risk factors for perinatal depression: personal and family history of mental illness, stressful life events in the year before pregnancy, conjugal conflict, domestic violence, single motherhood, social and economic deprivation, low educational level, unemployment, history of abuse during childhood, inadequate social support, young maternal age and loss of or separation from a parent before 16 years of age.27,30–39 Some studies have also observed a certain interaction between these risk factors, suggesting that the higher the number of risk factors, the greater the severity of depressive symptoms.40
The protective factors so far identified are: higher income, higher educational level, permanent or secure job, partner with a job, and adequate emotional and social support.28,35
Different scales can be used to detect symptoms of perinatal depression. The Edinburgh Postnatal Depression Scale (EPDS), for example, is a short, self-administered 5–10min scale designed to improve detection of postpartum depression in rural communities in developing countries, and has also been tested for use in the prenatal period.
The first step in treating perinatal depression and preventing negative outcomes in both the mother and baby is to introduce mechanisms for the early detection of depression or risk factors for depression in pregnant women.
MethodsWe performed a cross-sectional study in patients admitted to the High Complexity Obstetric Care (HCOC) unit from January to June 2014, during the introduction of the programme. We used the EPDS and an in-house questionnaire to identify the presence of depressive symptoms and psychosocial risk factors.
Our aim was to detect the presence of depressive symptoms using the EPDS and the frequency of the psychosocial variables routinely evaluated by the interdisciplinary team in patients with depressive symptoms detected by the EPDS.
The EPDS scale consists of 10 items; the first 9 explore the cognitive symptoms of depression and the last item is specific for self-harm ideas in the last 7 days. It has been translated into Spanish and validated in Latin America in general, and Colombia in particular.41 With a cut-off point of 10, the EPDS has a sensitivity of 100%, a specificity of 80% and a positive predictive value of 37%.42 The EPDS is a screening scale, and it was initially administered by the study nurse at admission, together with a questionnaire developed by the authors to evaluate certain psychosocial and clinical variables.
In this study, we present the results of our evaluation of the data from the first stage of the implementation of a programme for early detection and comprehensive management of depressive symptoms and depression in pregnant women treated in the HCOC unit of the Fundación Valle del Lili. The unit is staffed by a multidisciplinary team that includes gynaecologists, psychiatrists, psychologists, occupational therapists and social workers. The sample comprised all patients aged over 18 years admitted to the HCOC hospitalisation unit for gynaecological disorders during pregnancy or after delivery during the study period who agreed to participate in the study and signed the informed consent form.
The study was conducted according to international bioethical standards, and was approved by the ethics committee of the Fundación Valle de Lili Clinical.
Although this is an administrative database, this study was planned from the moment data collection started. The Fundación Valle del Lili is a private tertiary referral clinic located in the south west of Colombia. It provides highly complex medical care for individuals included in both the contributory and subsidised schemes of the General Social Security System (GSSS).
Analytical planWe conducted an initial exploratory analysis and a descriptive analysis of the population, and determined the frequency of depressive symptoms in the sample of women and the distribution of sociodemographic variables. We then compared the distribution of study variables between groups using the χ2 and Fisher's exact test, as appropriate. For normally distributed continuous variables the Student's t-test was used; for variables with non-normal distribution, the Mann–Whitney U test was used. The strength of association between the dependent variable and independent variables (bivariate analysis) was determined by the odds ratio (OR) and 95% confidence interval (95% CI).
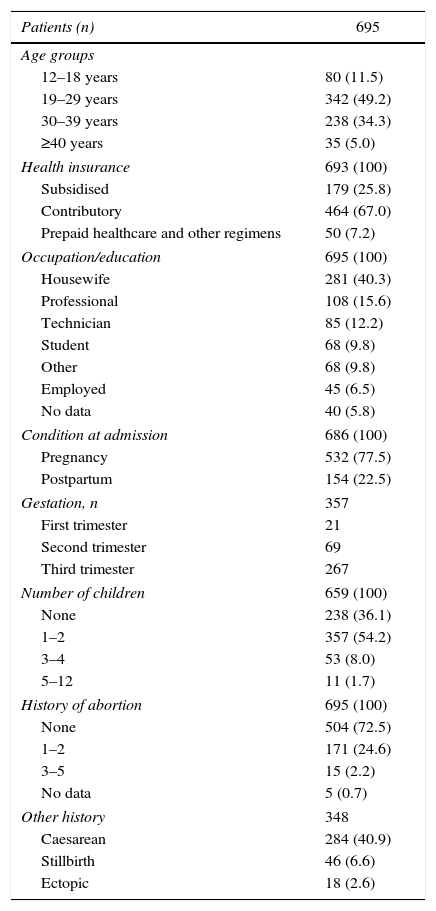
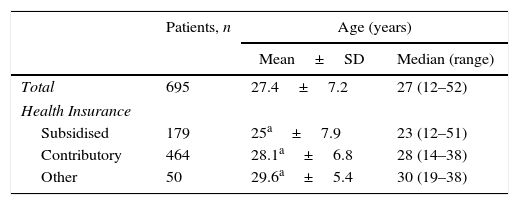
ResultsA total of 695 women admitted to the HCOC during the period from January to June 2014 were evaluated. The average age was 27.4 years; 40% were housewives and 67% were enrolled in the contributory scheme of the GSSS (Tables 1 and 2).
Sociodemographic characteristics.
| Patients (n) | 695 |
|---|---|
| Age groups | |
| 12–18 years | 80 (11.5) |
| 19–29 years | 342 (49.2) |
| 30–39 years | 238 (34.3) |
| ≥40 years | 35 (5.0) |
| Health insurance | 693 (100) |
| Subsidised | 179 (25.8) |
| Contributory | 464 (67.0) |
| Prepaid healthcare and other regimens | 50 (7.2) |
| Occupation/education | 695 (100) |
| Housewife | 281 (40.3) |
| Professional | 108 (15.6) |
| Technician | 85 (12.2) |
| Student | 68 (9.8) |
| Other | 68 (9.8) |
| Employed | 45 (6.5) |
| No data | 40 (5.8) |
| Condition at admission | 686 (100) |
| Pregnancy | 532 (77.5) |
| Postpartum | 154 (22.5) |
| Gestation, n | 357 |
| First trimester | 21 |
| Second trimester | 69 |
| Third trimester | 267 |
| Number of children | 659 (100) |
| None | 238 (36.1) |
| 1–2 | 357 (54.2) |
| 3–4 | 53 (8.0) |
| 5–12 | 11 (1.7) |
| History of abortion | 695 (100) |
| None | 504 (72.5) |
| 1–2 | 171 (24.6) |
| 3–5 | 15 (2.2) |
| No data | 5 (0.7) |
| Other history | 348 |
| Caesarean | 284 (40.9) |
| Stillbirth | 46 (6.6) |
| Ectopic | 18 (2.6) |
The values are expressed as n (%) unless otherwise indicated.
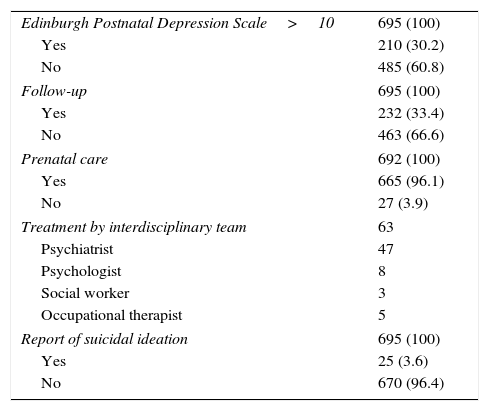
Clinical variables.
| Edinburgh Postnatal Depression Scale>10 | 695 (100) |
| Yes | 210 (30.2) |
| No | 485 (60.8) |
| Follow-up | 695 (100) |
| Yes | 232 (33.4) |
| No | 463 (66.6) |
| Prenatal care | 692 (100) |
| Yes | 665 (96.1) |
| No | 27 (3.9) |
| Treatment by interdisciplinary team | 63 |
| Psychiatrist | 47 |
| Psychologist | 8 |
| Social worker | 3 |
| Occupational therapist | 5 |
| Report of suicidal ideation | 695 (100) |
| Yes | 25 (3.6) |
| No | 670 (96.4) |
The mean age of women enrolled in the subsidised scheme was lower (p=0.0001) than that of those enrolled in the contributory regime (Tables 3 and 4).
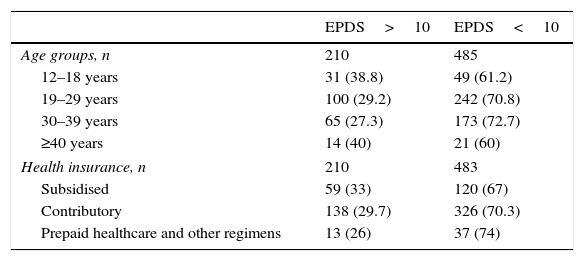
Depressive symptoms according to the Edinburgh scale.
| EPDS>10 | EPDS<10 | |
|---|---|---|
| Age groups, n | 210 | 485 |
| 12–18 years | 31 (38.8) | 49 (61.2) |
| 19–29 years | 100 (29.2) | 242 (70.8) |
| 30–39 years | 65 (27.3) | 173 (72.7) |
| ≥40 years | 14 (40) | 21 (60) |
| Health insurance, n | 210 | 483 |
| Subsidised | 59 (33) | 120 (67) |
| Contributory | 138 (29.7) | 326 (70.3) |
| Prepaid healthcare and other regimens | 13 (26) | 37 (74) |
EPDS: Edinburgh Postnatal Depression Scale.
Of the total sample, 77% were pregnant at admission, 54% of the women evaluated had 1 or 2 children, and 96% of them had received prenatal care. It was found that 30.2% of the women scored ≥10 on the EPDS, and 3.6% reported thoughts of self-harm (Tables 1–4).
The psychosocial risk factors evaluated were age, health insurance (a proxy for social and economic status, since individuals enrolled in the contributory regimen have a higher level of income than those in the subsidised regimen), number of children, history of abortion, history of sexual and emotional abuse, previous suicide attempts, personal or family history of depression and cohabitation with the spouse (Table 1).
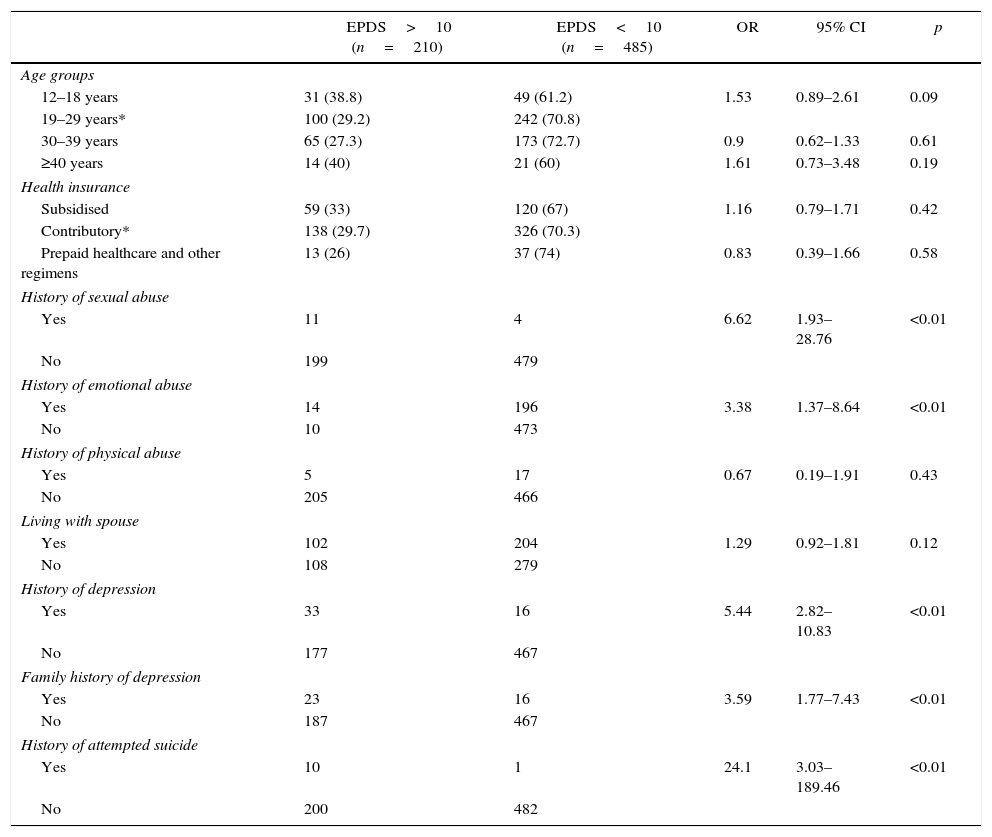
The bivariate analysis showed that women with depressive symptoms were more likely to report sexual (OR=6.6; 95% CI, 1.93–28.76) or emotional (OR=3.4, 95% CI, 1.37–8.64) abuse at some time during their life, previous suicide attempts and a personal and/or family history of depression (Table 5).
Bivariate analysis.
| EPDS>10 (n=210) | EPDS<10 (n=485) | OR | 95% CI | p | |
|---|---|---|---|---|---|
| Age groups | |||||
| 12–18 years | 31 (38.8) | 49 (61.2) | 1.53 | 0.89–2.61 | 0.09 |
| 19–29 years* | 100 (29.2) | 242 (70.8) | |||
| 30–39 years | 65 (27.3) | 173 (72.7) | 0.9 | 0.62–1.33 | 0.61 |
| ≥40 years | 14 (40) | 21 (60) | 1.61 | 0.73–3.48 | 0.19 |
| Health insurance | |||||
| Subsidised | 59 (33) | 120 (67) | 1.16 | 0.79–1.71 | 0.42 |
| Contributory* | 138 (29.7) | 326 (70.3) | |||
| Prepaid healthcare and other regimens | 13 (26) | 37 (74) | 0.83 | 0.39–1.66 | 0.58 |
| History of sexual abuse | |||||
| Yes | 11 | 4 | 6.62 | 1.93–28.76 | <0.01 |
| No | 199 | 479 | |||
| History of emotional abuse | |||||
| Yes | 14 | 196 | 3.38 | 1.37–8.64 | <0.01 |
| No | 10 | 473 | |||
| History of physical abuse | |||||
| Yes | 5 | 17 | 0.67 | 0.19–1.91 | 0.43 |
| No | 205 | 466 | |||
| Living with spouse | |||||
| Yes | 102 | 204 | 1.29 | 0.92–1.81 | 0.12 |
| No | 108 | 279 | |||
| History of depression | |||||
| Yes | 33 | 16 | 5.44 | 2.82–10.83 | <0.01 |
| No | 177 | 467 | |||
| Family history of depression | |||||
| Yes | 23 | 16 | 3.59 | 1.77–7.43 | <0.01 |
| No | 187 | 467 | |||
| History of attempted suicide | |||||
| Yes | 10 | 1 | 24.1 | 3.03–189.46 | <0.01 |
| No | 200 | 482 | |||
EPDS: Edinburgh Postnatal Depression Scale.
In this study, we present the data collected following the introduction of a programme for screening and treatment of depression in women with highly complex pregnancies at the Fundación Valle del Lili. It is the first study of its kind to be conducted in this population in Colombia. We found that 30.2% of study subjects presented depressive symptoms on the EPDS, and 3.6% reported thoughts of self-harm in the last 7 days.
In their systematic review, Gavin et al. showed that the combined prevalence of major and minor depression reported in the studies included in their meta-analysis varied from 6.5% to 12.9% in the different trimesters of pregnancy. However, the published rate of prenatal depression in Latin America is higher. Studies in Mexico and Chile have shown a prevalence of prenatal depression confirmed by clinical interview of 17.4% and 22%, respectively.27
In Colombia, studies using the Zung scale reported a prevalence of depressive symptoms in pregnant adolescents of 32.8%,30 while in Ecuador, the CESD-10 (Center for Epidemiologic Studies Depression) scale showed that 56.6% of pregnant women presented depression.43
Other researchers have used the EPDS with higher cut-off points to diagnose depression. In Peru, Lam et al. reported that 34.1% of pregnant women had an EPDS score ≥14, and Luna-Mattos et al. found 40.1% with an EPDS score ≥13. In Colombia, Borda-Pérez et al. reported a prevalence of 19.9% with an EPDS score ≥13 and Peinado-Valencia et al. found 31.5% with an EPDS score ≥14.
This shows that the prevalence of probable depression found in our study population is in line with national and South American data, and is greater than that described in other parts of the world.
A review of the studies included in the databases analysed failed to identify any papers dealing with the systematic evaluation and treatment of depressive symptoms in this patient group in Colombia.
In our study, the GSSS regimen of each patient was used as a proxy for social and economic status, as enrolment in this regimen means that the woman or her partner are currently employed, while individuals that are unemployed and have no private means receive medical attention under the subsidised regimen. For example, the differences found in age and number of children show that women from a lower social and economic status are more at risk of depression in this population.
The finding that 12% of all women with a positive EPDS score had ideas of self-harm is in line with the expected rate of suicidal ideation in the depressed patient population, which could be explained by the severity of the depressive symptoms found in this population.
Our findings highlight the importance of detecting risk factors that healthcare personnel do not usually identify and, therefore, do not treat, particularly during pregnancy. As previously mentioned, previous episodes of depression and a history of abuse and sexual violence increase the risk for the health and well-being of women and their children.
Some studies have used other variables not included in our study to evaluate this problem. For example, Peinado Valencia et al. found the number of children and non-Catholic religion to be risk factors; Borda et al. found an association with a history of abortion (OR=3.39, 95% CI, 1.41–8.15), some degree of family dysfunction (OR=2.78, 95% CI, 1.08–7.1) and activity outside the home (OR=2.92, 95% CI, 1.03–8.23).
In Mexico, Lara et al. found a history of depression in the mother of the pregnant woman (risk increased 0.8-fold), personal history of depression (risk increased 1.08-fold), lack of social support (risk increased 1.7-fold) and no partner (risk increased 1.51-fold) to be significant prenatal depression variables. These findings are consistent with our study.
Although probabilistic sampling was not performed, more than 600 women were systematically evaluated in this study. This provided a larger sample size than previous studies with similar methodologies conducted at a national and regional level. In addition, being a tertiary referral hospital, our sample is made up of women referred to the Valle de Lili Clinic from different public and private hospitals throughout the south-west region of Colombia. The methodology used to select study subjects, however, exposes the study to memory bias, insofar as patients with depressive symptoms are more likely to remember traumatic events in their lifetime than other, non-depressive patients.
This study provides some data that may be useful in future prospective studies that use the clinical interview to detect depressive disorders, and which evaluate specific outcomes – miscarriage, preeclampsia, preterm birth and low birth weight – associated with prenatal depression.15–18
This study also contributes to public health, insofar as it shows the need to improve the screening of depressive symptoms and the treatment of depression in high-risk pregnant women in Colombia, and can improve the health prognosis of both these patients and their children.
Ethical disclosuresProtection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of dataThe authors declare that no patient data appear in this article.
Right to privacy and informed consentThe authors declare that no patient data appear in this article.
Conflicts of interestThe authors have no conflicts of interest to declare.
Please cite this article as: Guerra AM, Dávalos Pérez DM, Castillo Martínez A. Detección de síntomas depresivos en mujeres gestantes de alta complejidad obstétrica y factores correlacionados. Rev Colomb Psiquiat. 2017;46:215–221.