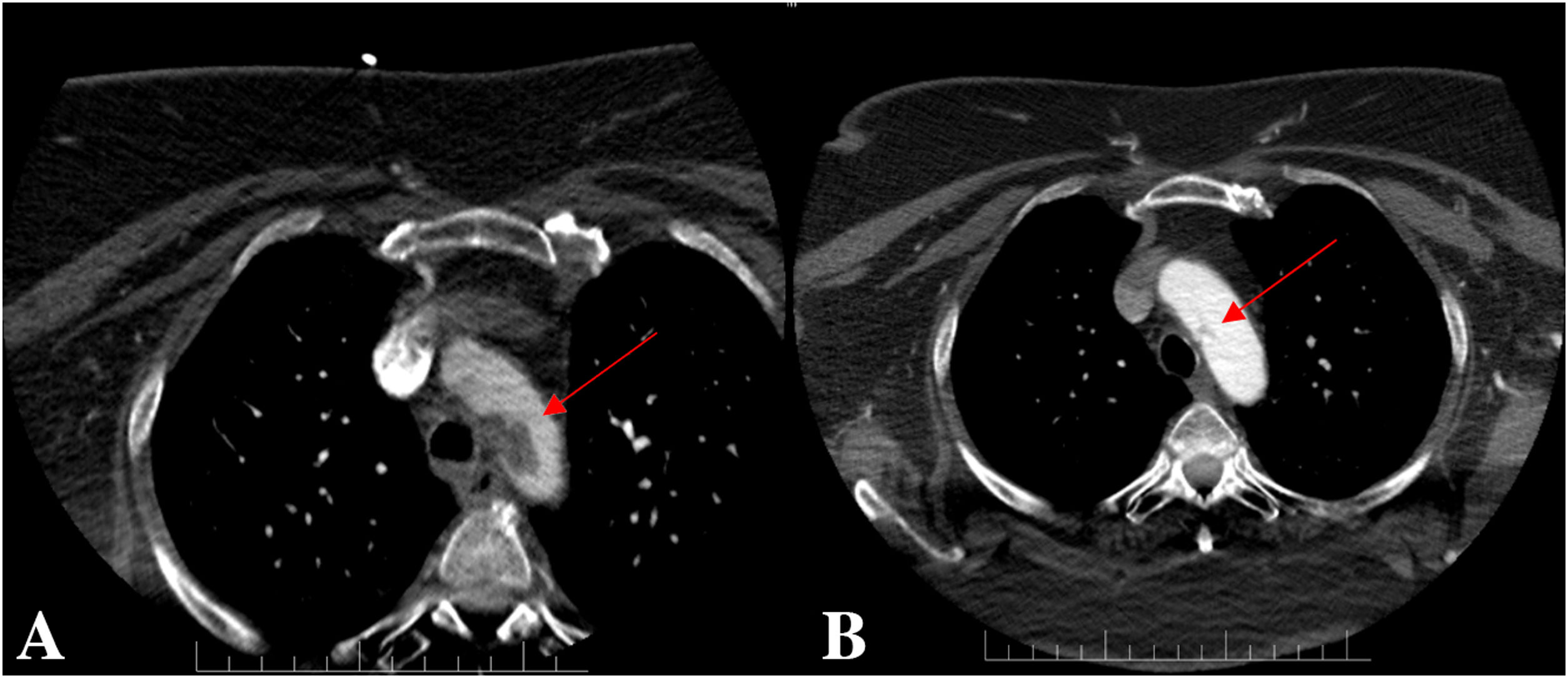
We report the case of a 61-year-old woman with a history of tobacco use, hypertension, and hyperlipidaemia. She was brought to our emergency department five hours after sudden onset of language impairment and right-side weakness. At admission the National Institutes of Health Stroke Scale (NIHSS) score was 23. Non-contrast computed tomography (CT) of the brain showed hypoattenuations in the left insular, lenticular and M2 regions (ASPECTS 7). Ensuing CT angiography (CTA) revealed an occlusion of the left middle cerebral artery (MCA) at the M1 segment and a voluminous (29.3mm×12.7mm×15.3mm) hypodense atherosclerotic plaque in the aortic arch, proximal to the subclavian and common carotid arteries (Fig. 1-A). Urgent mechanical thrombectomy (MT) with stent retriever was performed by direct percutaneous carotid access under ultrasound guidance. MCA perfusion was re-established in>50% of the territory (mTICI 2b) and haemostasis was achieved using an AngioSeal 6F closure device. No procedure-related complications occurred. Neurological examination at the following day revealed a significant improvement of the motor function and comprehension, the NIHSS score was 9. Dual antiplatelet therapy with aspirin and clopidogrel and a high intensity statin was started. The patient refused to undergo a transoesophageal echocardiography (TEE). A contrast enhanced transthoracic echocardiogram was performed showing an anechoic plaque proximal to the subclavian artery of identical dimensions to the one described in the CTA. No mobile thrombus was identified. One week later she was asymptomatic and was discharged home. Follow-up CTA was performed six weeks later, revealing a significant reduction of the atherosclerotic plaque, now measuring 7.45mm×8.35mm×4.7mm (Fig. 1-B). She remained asymptomatic and reported no complications at the follow-up visit.
Aortic arch atheroma (AAA) is a manifestation of systemic atherosclerosis and a potential source of artery-to-artery thromboembolism. Severe arch atheroma increases the risk of stroke up to four times and double the risk of recurrence.1,2 Ulceration, thickness>4mm and the presence of a mobile thrombus confer the biggest overall risk of embolism.3–5 TEE is the procedure of choice for measurement and detection in the elective setting. Performed as part of the evaluation after an acute stroke, it allows for precise detection and characterization of the plaque, as well as being able to determine the presence of a mobile thrombus.6 CTA is a non-invasive technique routinely performed in the acute phase of ischaemic stroke to detect large vessels occlusions. It also detects the presence of plaques in the aortic arch and provide information about its location, size, and density. Additionally, it can assess the anatomical configuration of the patient
Data for mechanical thrombectomy in presence of complex plaques in the aortic arch is scarce, but iatrogenic embolization from the plaque is a known and feared complication. It can happen while navigating the aortic arch, particularly among patients with difficult vascular anatomy.7 Trans-femoral catheterization is the standard access route for MT, but direct carotid puncture (DCP) has been reconsidered as an alternative access route in the last years. Several case series and multicentric registries are available.8–10 DCP has the advantage to bypass the aortic arch, reducing the periprocedural risk of stroke in such patients and shortening revascularization times.11 CTA performed in the acute phase of ischaemic stroke is of special importance here. It can assess the aortic arch and supra-aortic vessels and identify the subset of patients that might benefit from DCP as the initial access strategy.11
Medical treatment for AAA focus on blood pressure control, high intensity statin therapy, lifestyle changes and strict glycaemic control. The optimal antithrombotic management remains uncertain. The ARCH trial (Aortic Arch Related Cerebral Hazard)12 is the only randomized trial conducted specifically on this topic. It compared double antiplatelet therapy with aspirin plus clopidogrel (DAPT) against anticoagulation with warfarin. The DAPT arm showed a non-significant reduction in the rate of recurrent stroke and a significant reduction in vascular death compared to warfarin, while major haemorrhage rates were similar. Unfortunately, lower than expected event rates and slow recruitment ended the trial prematurely, so these results must be interpreted with caution.
In conclusion, AAA is a manifestation of systemic atherosclerosis and a significant source of embolism and stroke recurrence. The antithrombotic regime is uncertain, but high intensity statin therapy and DAPT seem reasonable. CT angiography performed in the acute phase of ischaemic stroke can assess the patient vascular anatomy and the characteristics of the aortic arch. If a complex plaque is present, DCP should be considered as the initial access strategy for MT. This approach has comparable reperfusion rates and can reduce the periprocedural risk of stroke and shorten procedure times.