Hypothyroidism is a common disease that is currently easily diagnosed and treated but is sometimes fatal. The most described symptoms are fatigue, intolerance to cold, weight gain, constipation, voice change and dry skin.1 The decompensation of hypothyroidism, myxoedema, is also well characterized. It can leads to multivisceral failure and require intensive care.2 Besides, some clinical forms are less evocative but nevertheless severe and require rapid management.
We present a 61-years-old man hospitalized for Streptococcus dysgalactiae bacteraemia. His only antecedent was hypertension treated with PERINDOPRIL. He reported recurrent vomiting, deterioration of general condition and fluctuating oedema of the lower limbs.
At admission, he presented a generalized scleroderma of the skin without digital ulceration, a limitation of the mouth opening, and a generalized oedema including face.
Biological abnormalities included normocytic anaemia at 9.6g/dl, inflammatory syndrome with CRP at 191.4mg/l and hyperleukocytosis at 14.83G/l, renal failure with glomerular filtration rate at 41ml/min, nephrotic syndrome with proteinuria at 7g/24h and hypoalbuminemia at 8g/l. Hypothyroidism was detected with TSH at 24.6 μU/ml (Norm 0.27; 4.20 μU/ml), T4L at 0.8 ng/dl (Norm 0.93; 1.7 ng/dl) and T3L at 1.87 pg/ml (Norm 2.0; 4.4 pg/ml).
Exploration of thyroid, including thyroid ultrasound and scintigraphy, anti-TPO, anti-TRAK and anti-thyroglobulin antibodies dosage showed no abnormality.
Exploration of cutaneous lesions with a scleroderma-Dot (including antibodies against Scl-70, CENP-A, CENP-B, PM-Scl 100, PM-Scl 75, Ku, RNA Polymerase III, U1-RNP, Th/to, fibrillarin, NOR90 and SSA/Ro 52kD) was negative. The skin biopsy revealed skin involvement with mucin deposits compatible with myxoedema.
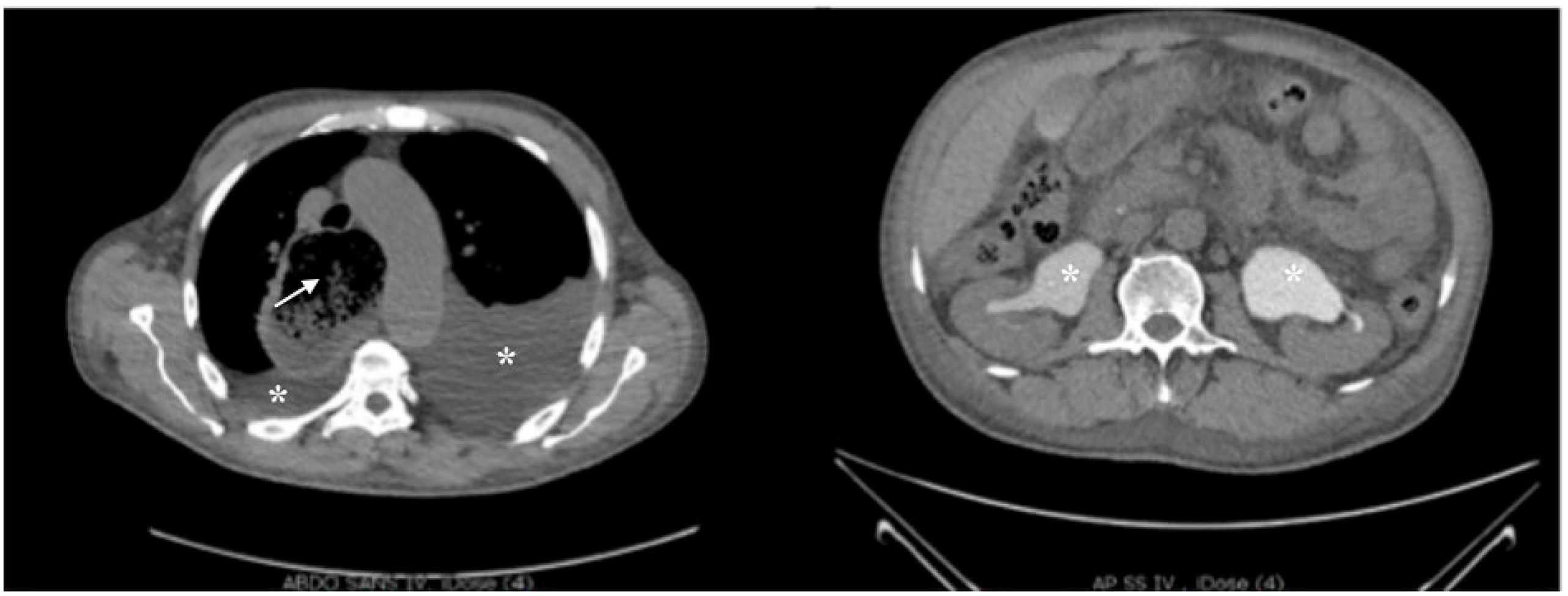
Exploration of deterioration of general condition and vomiting with a CT scan (Fig. 1) showed an anasarca, a megaoesophagus aspect and a bilateral pyelocaliceal dilatation due to a retroperitoneal fibrosis. A bilateral JJ tube was placed.
CT scan: Oesophagus distension (arrow) upstream of a stenotic aspect of the esophagogastric junction. Bilateral pleural effusion of moderate size (asterisk on the left image) and pericardial effusion of small size. Intraperitoneal effusion of moderate abundance and mesenteric fat densification. Bilateral pyelocaliceal dilatation (asterisk on the right image) without detectable lithiasis.
The major oesophageal dilatation was confirmed by endoscopy, and no abnormality was found on multilevel biopsy. Manometry showed an absence of contraction of the body of the oesophagus, suggesting aperistalsis according to the Chicago classification version 3.0.3
For the major nephrotic syndrome, the renal biopsy revealed a stage 3 extra membranous glomerulonephritis with positive anti PLA2R antibodies.
LEVOTHYROXINE and an angiotensin II receptor blocker were introduced, and a great rapid evolution was observed with regression of facial oedema within 3 weeks. He showed a progressive disappearance of skin lesions and the limitation of the mouth opening. Renal function progressively improved with proteinuria at 4g/24h and creatinine at 118μmol/l (Norm 80; 110 μmol/l) after 6 weeks of treatment. For the megaoesophagus, 2 injections of botulinum toxin under endoscopic control, leads to an improvement of the symptomatology.
Altogether, we report a case of hypothyroidism without anti-thyroid antibodies revealed by symptoms of cutaneous mucinosis, megaoesophagus and retroperitoneal fibrosis associated with glomerular nephropathy, and regressive after thyroid hormone supplementation.
Scleroderma-like conditions share fibrosis and thickening of the skin but have many different etiologies. They can be classified into several groups including immune/inflammatory mediated with abnormal deposits: mucinoses. Among the cutaneous mucinoses, dysthyroid mucinoses are described and can be revealed by a scleroderma-like skin involvement.4
Similarly, one of the well-known causes of megaoesophagus is systemic sclerosis. It is a rare disorder associated with hypothyroidism,5 but our case report underlines the importance of evoking this diagnosis for the therapeutic management.
The association of hypothyroidism and extra membranous glomerulonephritis has been reported in a context of autoimmune diseases with an association of autoimmune thyroiditis and anti PLA2R glomerulonephritis.6 In our case, we cannot exclude that, despite the absence of anti-thyroid antibody detection, the mechanism of hypothyroidism is autoimmune.7
Another mechanism that could explain this association would be the renal loss of thyroid hormones due to the nephrotic syndrome, leading to secondary hypothyroidism.8
Retroperitoneal fibrosis is a poorly understood entity with multiple causes including autoimmune diseases.9 Although the pathophysiology is poorly understood, rare associations between hypothyroidism and retroperitoneal fibrosis have also been described.10
In conclusion, although hypothyroidism is very frequent and often typical, it can present with more complicated and severe pictures. In these cases, the implementation of treatment is an emergency, and collaboration between different medical specialties is necessary for a good management.
Ethical disclosuresNo included since there are no personal details of patient, including illustrations.
FundingThis research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.