Strategies to determine who could be safely discharged home from the Emergency Department (ED) in COVID-19 are needed to decongestion healthcare systems.
ObjectivesTo describe the outcomes of an ED triage system for non-severe patients with suspected COVID-19 and possible pneumonia based on chest X-ray (CXR) upon admission.
Material and methodsRetrospective, single-center study performed in Barcelona (Spain) during the COVID-19 peak in March–April 2020. Patients with COVID-19 symptoms and potential pneumonia, without respiratory insufficiency, with priority class IV–V (Andorran triage model) had a CXR upon admission. This approach tried to optimize resource use and to facilitate discharges. The results after adopting this organizational approach are reported.
ResultsWe included 834 patients, 53% were female. Most patients were white (66%) or Hispanic (27%). CXR showed pneumonia in 523 (62.7%). Compared to those without pneumonia, patients with pneumonia were older (55 vs 46.6 years old) and had a higher Charlson comorbidity index (1.9 vs 1.3). Patients with pneumonia were at a higher risk for a combined outcome of admission and/or death (91 vs 12%). Death rates tended to be numerically higher in the pneumonia group (10 vs 1). Among patients without pneumonia in the initial CXR, 10% reconsulted (40% of them with new pneumonia).
ConclusionCXR identified pneumonia in a significant number of patients. Those without pneumonia were mostly discharged. Mortality among patients with an initially negative CXR was low. CXR triage for pneumonia in non-severe COVID-19 patients in the ED can be an effective strategy to optimize resource use.
La pandemia de COVID-19 conlleva una alta ocupación de los servicios de urgencias (SU). Se requieren nuevas estrategias para optimizar la gestión de estos recursos.
ObjetivosDescribir los resultados de un sistema de triaje en urgencias para pacientes no graves con sospecha de COVID-19 y posible neumonía, basado en la radiografía de tórax (RT).
Material y métodosEstudio retrospectivo, unicéntrico realizado en Barcelona (España) entre marzo y abril de 2020. Se realizó una RT al ingreso en SU de pacientes con síntomas de COVID-19 y sospecha de neumonía, sin insuficiencia respiratoria, con una prioridad clase IV-V (sistema andorrano de triaje). Esta medida pretende optimizar los recursos y facilitar las altas. Se reportan los resultados tras adoptar esta estrategia.
ResultadosSe incluyeron 834 pacientes (53% mujeres, 66% caucásicos, 27% hispánicos). La RT mostró neumonía en 523 (62,7%). Comparados con los pacientes sin neumonía, los que sí la padecían eran mayores (55 vs. 46,6 años), con un índice de comorbilidad de Charlson más elevado (1,9 vs. 1,3) y con mayor riesgo de ingreso y/o muerte (91 vs. 12%). La mortalidad fue numéricamente mayor en el grupo con neumonía (10 vs. 1). El 10% de los pacientes sin neumonía en RT consultaron de nuevo al SU (40% con neumonía).
ConclusiónLa RT identificó neumonía en múltiples pacientes. Los que no tenían neumonía fueron mayoritariamente dados de alta. La mortalidad entre pacientes con RT negativa fue baja. La RT como triaje para neumonía en pacientes con COVID-19 no grave puede ahorrar recursos.
The disease associated with the 2019 coronavirus or COVID-19 was described after reports of patients with pneumonia associated with a new coronavirus (SARS-CoV-2) in Wuhan (China) in late 2019. Currently, COVID-19 is a global pandemic.1 The clinical presentation of COVID-19 is variable, ranging from asymptomatic presentations to flu-like symptoms or adult respiratory distress syndrome (ARDS). Respiratory complications typically appear about 7–10 days after the first symptom,2 causing significant morbidity and mortality.3–5
The spread of SARS-CoV-2 has caused significant peaks in healthcare demand. Emergency Department (ED) triage during a pandemic is closer to that of an accident with multiple victims. Furthermore, no COVID-19 specific validated strategies have been developed, despite different proposals exist.6 In early 2020, the rapid increase of the number of cases was followed by a significant number of limitations: diagnostic capacity (less sensitive and slower polymerase chain reaction (PCR) tests, no valid antigen tests), clinical space, human resources, and personal protective equipment. The preexisting experiences from China and Italy showed that chest X-ray (CXR) had a limited sensitivity to diagnose COVID-19 versus chest computerized tomography (CT), especially earlier in the disease.7 The European Society of Radiology encouraged EDs to use CT.8
Due to high patient volumes and congestion of our center in Barcelona, Spain, generalizing the use of chest CT was deemed as not feasible. CXRs’ sensitivity for COVID-19 is 69-75% and it increases with a higher prevalence.9 Patients with severe manifestations, especially respiratory insufficiency, would obviously need admission to the hospital and high-level acute care at the ED. We considered that CXR would be a fast and cheap way to stratify the different levels of severity upon ED triage in patients without apparent signs of severity on admission. This way, we would be able to safely discharge some of them home, to concentrate our limited in-hospital resources on the right cases during the peak.
The aim of this study is to report the outcomes of an ED triage system based on CXR for non-severe patients with suspected COVID-19 and possible pneumonia.
Material and methodsDesign and settingWe performed a retrospective cohort study including patients visited at the Emergency Department (ED) at the Vall d’Hebron University Hospital (Barcelona, Spain) from March 25 to April 8, 2020. This is a university tertiary care center, with more than 1000 in-patient beds, with an assigned population of more than 450,000 people. The period of inclusion included the 2 weeks when the hospital was at full capacity, corresponding to the first incidence peak in the COVID-19 pandemic in Catalonia (Spain). For the 7-day period March 30 to April 5, 2020, the 14-day cumulative incidence of COVID-19 cases in Catalonia was 267.07 (population as of January 1, 2020, was 7,722,203 inhabitants), 8928 new cases were diagnosed with PCR, and 2649 people died.10 On 31 March 2020, the center reached the peak of COVID-19 activity, accounting for 100 daily admissions, 170 inpatients at the intensive care unit, and more than 600 inpatients in conventional wards.
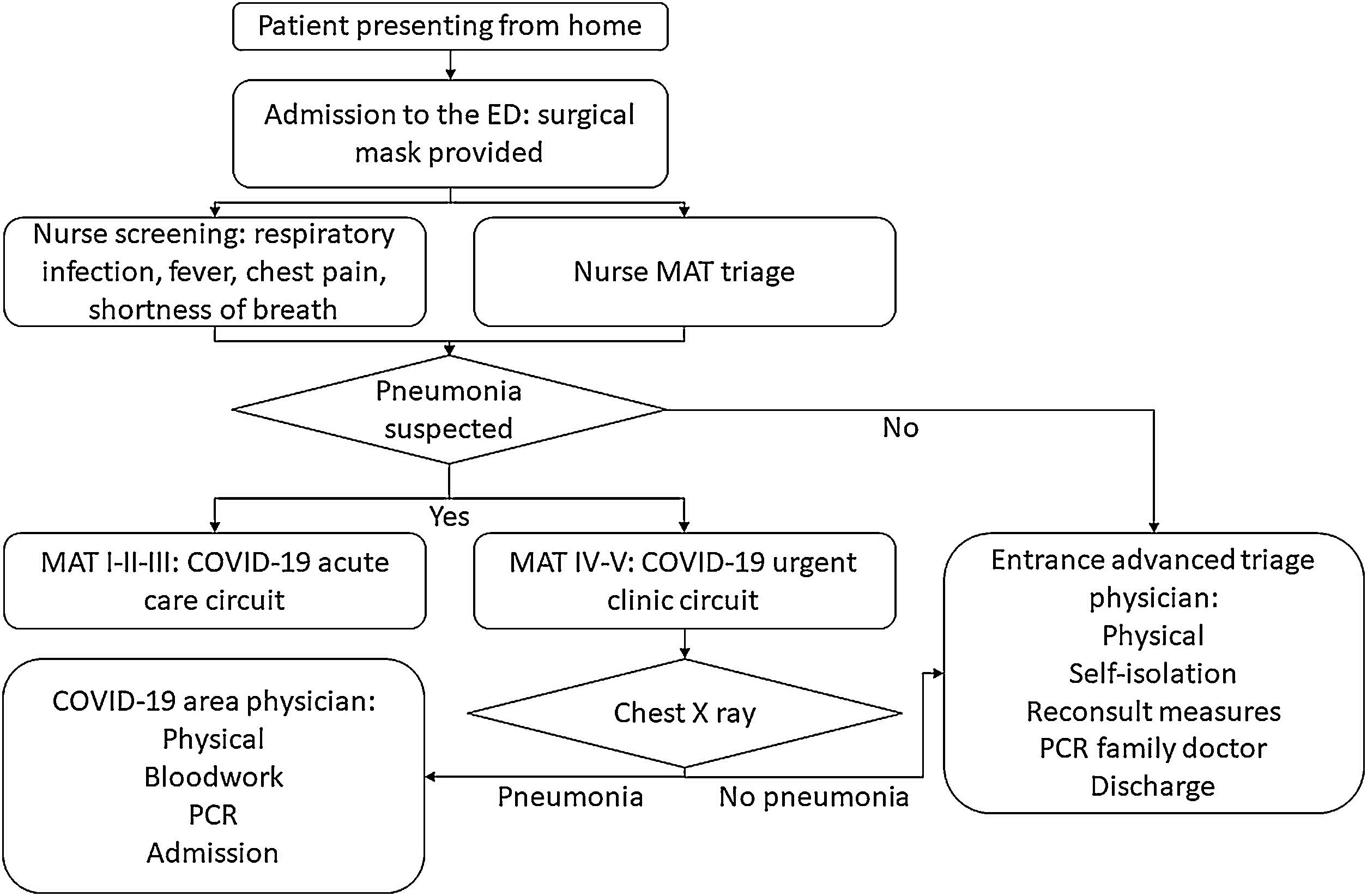
In this context, a protocol for COVID-19 triage and management had been implemented at the institution (Fig. 1). Most of the patients visited at the ED had suspected COVID-19 and a physically separated circuit was made for non-COVID-19 patients. Patients reporting possible COVID-19 symptoms were identified at the entrance, admitted to the ED, and triaged by a registered nurse using the Andorran triage model (MAT),11,12 an adaptation from the Canadian Emergency Department Triage and Acuity Scale (CTAS).13 Patients scoring levels I to III were transferred to the acute care area (more severe cases or deconditioned, generally needing oxygen, stretcher). Patients in levels IV and V suspicious for pneumonia were directly sent for CXR (posterior-anterior and lateral projections, reported by a dedicated radiologist) and moved to a separated waiting room. If the CXR was negative for pneumonia they were taken back to an advanced triage office, where a physician made a rapid assessment, provided isolation recommendations and symptomatic treatment, and discharged patients to the care of their general practitioner. Due to the limited availability of PCR kits, those patients had them, depending on availability, a few days after under primary care supervision. Those patients with pneumonia or with more functional impairment or inability to isolate at home were assessed by an ED physician, got bloodwork drawn and a therapeutic/admission decision was taken. This subgroup of patients had their PCR swab at the ED (Allplex 2019-nCoV, Seegene, Seoul, South Korea14). No antigen or serology tests were available, and the turnover for the microbiology lab results was 8–12h.
PatientsInclusion criteria were:
- -
Patients ≥16 years-old visited at the ED from March 25 to April 8, 2020.
- -
Screening positive for suspected COVID-19 symptoms and pneumonia (including usual symptoms i.e. fever, cough, myalgias, dyspnea, chest pain, …).
- -
MAT11,12 level IV or V.
- -
Oxygen saturation (SpO2) room air≥95%.
A search into the electronic medical record SAP® was performed including the following items: patients visited at the ED for medical pathologies (non-surgical, ortho, gynecology or pediatric), visits from March 25 to April 8, 2020, MAT levels IV or V, diagnostic codes specific for coronavirus infection (coronavirus, non-specific coronavirus infection, other coronaviruses that cause diseases elsewhere specified) or any viral or respiratory infection. We obtained 1046 clinical encounters. All charts were reviewed to check that the COVID-19 working diagnosis was accurate, information was available, and patients with repeated consults were identified. The review was performed from June 19 to August 20, 2020. An anonymized password-protected database was created along with an encrypted master list kept by AFC, ASG, JLA, and IPF. The research team reviewed the different charts including the ED visit and the data available in the EMR (in-hospital care, primary care) including the evolution up to 14 days after the ED visit, and recorded any death (in-patient or outpatient) in the following 6 weeks. The demographic variables included: sex, age, race, smoker status, Charlson comorbidity index score, death, and date of death. For COVID-19 specific items, we reviewed: SARS-CoV-2 PCR status, time since the first symptom, reported symptoms (headache, nasal congestion, dry cough, expectoration, fatigue, dyspnea, nausea or vomiting, diarrhea, myalgia, anosmia, dysgeusia, fever, or febricula), vitals (systolic blood pressure, diastolic blood pressure, heart rate, respiratory rate, temperature, SpO2 room air), triage chest X-ray status (viral pneumonia or not), re-consult at the ED or primary care, and presence of complications (pneumonia, deep vein thrombosis, pulmonary embolism).
Statistical analysisSTATA 14.1 software was used for the statistical analysis. p<0.05 was considered significant. Dichotomous variables were expressed as absolute frequencies and percentages, and continuous variables were reported as means and standard deviations. Comparisons between groups were made using Chi-squared, Fisher's exact tests, or Student's t-test, as appropriate. Logistic and linear regression were used to adjust comparisons for age, gender, and race.
EthicsThe study design adhered to the declaration on Helsinki for ethical principles for medical research involving human subjects. The local ethics review board reviewed and approved this protocol (PR(AG)334/2020). Since it was a retrospective study using chart review, the obtention of informed consent was waived. This manuscript follows the STROBE recommendations for reporting observational studies.
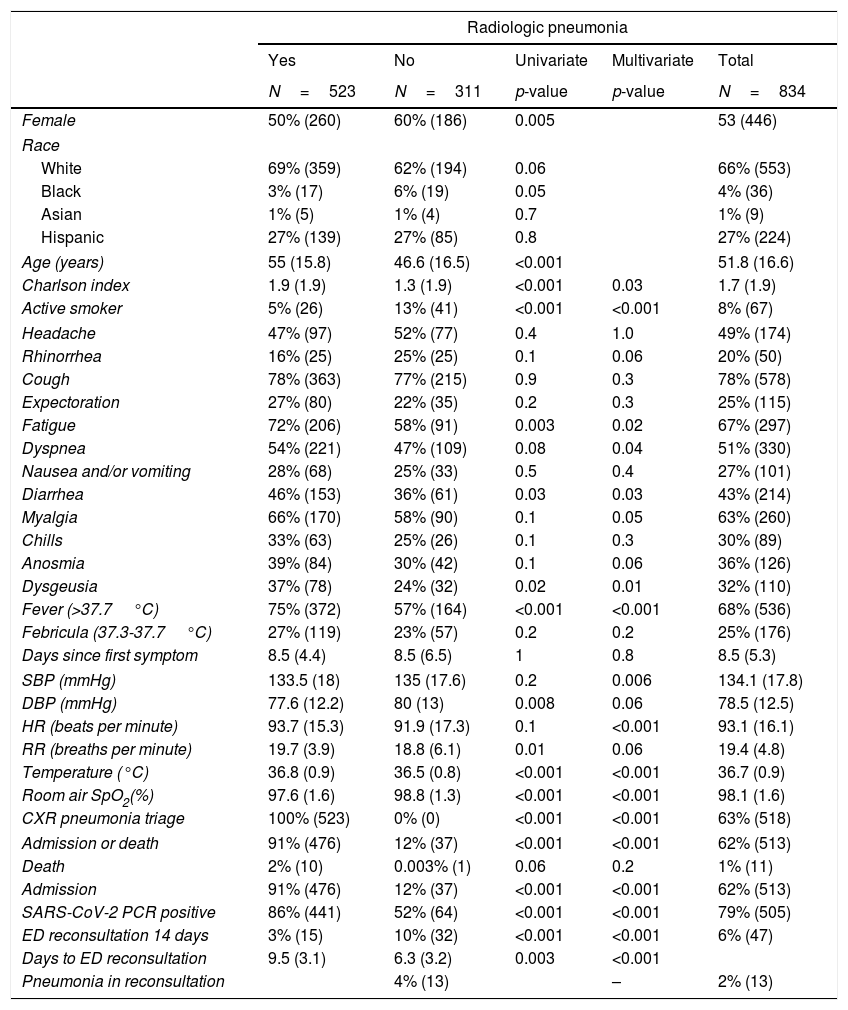
ResultsFrom 1046 consecutive clinical encounters at our institution's ED with MAT levels IV–V held from March 25 to April 8, 2020, we identified 834 patients with suspected non-severe COVID-19 pneumonia, who met the inclusion criteria. The demographics and COVID-19-related symptoms reported during the ED visit are shown in Table 1.
Comparison of the characteristics of patients triaged as non-severe suspected COVID-19 depending on the presence of pneumonia in the chest X-ray.
| Radiologic pneumonia | |||||
|---|---|---|---|---|---|
| Yes | No | Univariate | Multivariate | Total | |
| N=523 | N=311 | p-value | p-value | N=834 | |
| Female | 50% (260) | 60% (186) | 0.005 | 53 (446) | |
| Race | |||||
| White | 69% (359) | 62% (194) | 0.06 | 66% (553) | |
| Black | 3% (17) | 6% (19) | 0.05 | 4% (36) | |
| Asian | 1% (5) | 1% (4) | 0.7 | 1% (9) | |
| Hispanic | 27% (139) | 27% (85) | 0.8 | 27% (224) | |
| Age (years) | 55 (15.8) | 46.6 (16.5) | <0.001 | 51.8 (16.6) | |
| Charlson index | 1.9 (1.9) | 1.3 (1.9) | <0.001 | 0.03 | 1.7 (1.9) |
| Active smoker | 5% (26) | 13% (41) | <0.001 | <0.001 | 8% (67) |
| Headache | 47% (97) | 52% (77) | 0.4 | 1.0 | 49% (174) |
| Rhinorrhea | 16% (25) | 25% (25) | 0.1 | 0.06 | 20% (50) |
| Cough | 78% (363) | 77% (215) | 0.9 | 0.3 | 78% (578) |
| Expectoration | 27% (80) | 22% (35) | 0.2 | 0.3 | 25% (115) |
| Fatigue | 72% (206) | 58% (91) | 0.003 | 0.02 | 67% (297) |
| Dyspnea | 54% (221) | 47% (109) | 0.08 | 0.04 | 51% (330) |
| Nausea and/or vomiting | 28% (68) | 25% (33) | 0.5 | 0.4 | 27% (101) |
| Diarrhea | 46% (153) | 36% (61) | 0.03 | 0.03 | 43% (214) |
| Myalgia | 66% (170) | 58% (90) | 0.1 | 0.05 | 63% (260) |
| Chills | 33% (63) | 25% (26) | 0.1 | 0.3 | 30% (89) |
| Anosmia | 39% (84) | 30% (42) | 0.1 | 0.06 | 36% (126) |
| Dysgeusia | 37% (78) | 24% (32) | 0.02 | 0.01 | 32% (110) |
| Fever (>37.7°C) | 75% (372) | 57% (164) | <0.001 | <0.001 | 68% (536) |
| Febricula (37.3-37.7°C) | 27% (119) | 23% (57) | 0.2 | 0.2 | 25% (176) |
| Days since first symptom | 8.5 (4.4) | 8.5 (6.5) | 1 | 0.8 | 8.5 (5.3) |
| SBP (mmHg) | 133.5 (18) | 135 (17.6) | 0.2 | 0.006 | 134.1 (17.8) |
| DBP (mmHg) | 77.6 (12.2) | 80 (13) | 0.008 | 0.06 | 78.5 (12.5) |
| HR (beats per minute) | 93.7 (15.3) | 91.9 (17.3) | 0.1 | <0.001 | 93.1 (16.1) |
| RR (breaths per minute) | 19.7 (3.9) | 18.8 (6.1) | 0.01 | 0.06 | 19.4 (4.8) |
| Temperature (°C) | 36.8 (0.9) | 36.5 (0.8) | <0.001 | <0.001 | 36.7 (0.9) |
| Room air SpO2(%) | 97.6 (1.6) | 98.8 (1.3) | <0.001 | <0.001 | 98.1 (1.6) |
| CXR pneumonia triage | 100% (523) | 0% (0) | <0.001 | <0.001 | 63% (518) |
| Admission or death | 91% (476) | 12% (37) | <0.001 | <0.001 | 62% (513) |
| Death | 2% (10) | 0.003% (1) | 0.06 | 0.2 | 1% (11) |
| Admission | 91% (476) | 12% (37) | <0.001 | <0.001 | 62% (513) |
| SARS-CoV-2 PCR positive | 86% (441) | 52% (64) | <0.001 | <0.001 | 79% (505) |
| ED reconsultation 14 days | 3% (15) | 10% (32) | <0.001 | <0.001 | 6% (47) |
| Days to ED reconsultation | 9.5 (3.1) | 6.3 (3.2) | 0.003 | <0.001 | |
| Pneumonia in reconsultation | 4% (13) | – | 2% (13) | ||
N=absolute number, SBP=systolic blood pressure, DBP=diastolic blood pressure, HR=heart rate, RR=respiratory rate, SpO2=oxygen saturation, CXR=chest X-ray, PCR=polymerase chain reaction, ED=Emergency Department. Dichotomous variables were expressed as absolute frequencies and percentages, and continuous variables as means and standard deviations. Univariate bivariate comparisons for continuous variables used the Student's t-test and for dichotomous variables the Fisher's or Chi-squared tests, as appropriate. Multivariate comparisons used logistic and linear regression to adjust for age, gender, and race.
All patients had their triage CXR. The features and outcomes according to the presence or absence of radiological viral pneumonia are also presented in Table 1. Compared to those without radiological evidence of pneumonia, patients with pneumonia were more likely to be male and older, without racial clinically relevant differences. In addition, they reported fatigue, dyspnea, diarrhea, myalgia, dysgeusia, and fever more frequently (all adjusted p≤0.05).
Those presenting with pneumonia were statistically significantly more likely to be admitted to the hospital and mortality tended to be higher in this subgroup. Patients reconsulting were earlier in the course of the disease the first time they came to the ED (6.5 days from the first symptom vs. 8.6 in those who did not come back to the ED, p<0.009 multivariate analysis), were more likely to have a normal baseline CXR in the initial ED visit (62% vs. 32%, p<0.001) and experienced a lower number of deaths (2 vs. 9, p<0.009). Deep vein thrombosis and pulmonary embolism within 14 days just appeared in 3 patients in the pneumonia subset.
Deceased patients were all white. They had a median age of 80 years and a median Charlson index of 5.4, all statistically significantly different from the surviving cases. Ten of them had pneumonia in their triage CXR and one did not. She reconsulted 3 days after with a pathologic CXR.
DiscussionIn the context of an abrupt surge of cases and with the need to optimize the use of resources, we explored the use of CXR to screen non-critical patients with suspected COVID-19 pneumonia in the ED setting. CXR was able to identify viral pneumonia in 60% of 834 patients without respiratory insufficiency and MAT IV–V. Those with a negative CXR were discharged home. ED reconsults were limited in number, although forty percent of them had new pneumonia in the control CXR. Mortality was 0.003% among patients with negative CXR. CXR for COVID-19 pneumonia screening in non-severe patients at the ED is an effective and feasible strategy to stratify those patients in need of hospital care and those who do not.
Barcelona was no exception for the COVID-19 pandemic. The high volumes of patients posed a significant organizational challenge to provide the right level of care to each patient in a timely fashion. Human resources, space, respiratory therapy equipment, personal protective equipment, and SARS-CoV-2 tests were scarce in our country,15 like in many others. Patients with respiratory insufficiency and/or pneumonia clearly need inpatient medical treatment to some degree and can be easily identified at the ED in the more severe triage groups (MAT or CTAS I–III). This subset of patients will consume a significant part of the ED capacity. Therefore, identifying patients who could be safely discharged is a priority.
The demographics of our series of patients corresponded to a subset of younger and less comorbid group of patients, compared to all the patients who were visited at an ED16 or ended up being admitted due to COVID-19 in Spain.17 This is because our cases corresponded to mild COVID-19 disease, without respiratory insufficiency or any other major organ damage as per MAT triage IV–V. On presentation, patients mainly reported cough, fatigue, myalgia, and fever. Dyspnea was only present in half of the patients, whereas other reports mixing severe and non-severe patients found over 70% of cases with shortness of breath.18 In terms of disease duration, patients came to the ED about 8 days after the first symptom like in many other European series.16,18 Vitals on arrival are not comparable, as we did not include more severe patients. Some patients had fever, but none had respiratory insufficiency or hemodynamical instability. The lower number of positive PCR for the negative CXR subgroup can be explained due to the delayed performance of the swab in those patients that were discharged, as the viral load gets lower over time.
We found that 60% of the screened patients had viral pneumonia in the CXR. CXR was initially discouraged for diagnosis of pneumonia in SARS-CoV-2 in low prevalence areas.19 In a context like ours, it was found in a significant number of cases among patients without respiratory insufficiency. CXR is cheap and can be done in any ED. Other imaging approaches have proved effective in diagnosing COVID-19 pneumonia. Using chest CT scans would include a dedicated machine and more time to do the image acquisition, which is not feasible admitting 100 patients a day. Lung ultrasound is another promising technique to diagnose COVID-19 pneumonia and to provide a prognosis in terms of respiratory deterioration in critical patients.20,21 Quicker than CTs, it is not available in all centers and needs personnel with ultrasound skills. Our initial approach of dedicated radiologists reporting the tests has been recently refined. A simple semiquantitative score has been created to stage the degree of involvement (<1/3, 1/3 to 2/3, or >2/3 of lung parenchyma affected by alveolar opacities), correlating with the risk of intubation after presentation at the ED.22 Artificial intelligence has been used to interpret retrospectively chest radiography, being able to predict adverse outcomes in COVID-19.23 Nevertheless, in a healthcare system at the brink of collapse, any ED physician can interpret the CXR on its own.
Patients with suspected COVID-19 and possible pneumonia with a negative CXR screening were younger, predominantly female, with fewer comorbidities, and experienced less mortality than those with pneumonia. Once pneumonia was ruled out, they were discharged home under primary care supervision. This provided an important relief to the high volume of patients needing to remain at the hospital. Forty percent of patients without previous pneumonia who reconsulted had a newly diagnosed pneumonia. This is attributable to a lower number of days since the first symptom at the first ED visit. Hence, pneumonia might not be visible in the first CXR or simply had not developed already. Only one old and frail patient with pneumonia in the second visit ended up dying. One study in New York (USA) showed that 5.6% of COVID-19 patients reconsulted to the ED within 72h after being discharged.24 CXR was not systematically done, but 41% of the reconsults needing admission had an abnormal CXR at the initial visit. Moreover, only 25% of the admissions had a previously normal CXR. Mortality was 16%. Another Spanish study on 925 COVID-19 discharges from the ED, found a 20.5% of ED re-consultations, mostly within patients with CTAS III. Patients needing to be revisited differed from those who did not in having new CXR findings or not having a previous chest radiography, an older age, and comorbidities. They suggested discharging any suspected COVID-19 patient under 48 years old without comorbidities and with normal vitals. Finally, a severity score for the need for high flow oxygen (and therefore a worse prognosis) was recently developed in our center with COVID-19 patients admitted to the Internal Medicine ward.25 Seventy percent of the patients did not need oxygen on admission. The main predictors for that outcome were: SpO2/fraction of inspired oxygen (adjusted Hazard Ratio-aHR=8), CXR (aHR=4), prior immunosuppressive therapy (aHR=4), obesity (aHR=2), interleukin-6 serum levels (aHR=2) and platelet count (aHR=0.5).
This study is limited by its retrospective and single-center design. The triage algorithm might be difficult to export to other centers with different characteristics and epidemiological situations. Moreover, variables were obtained from medical reports performed under a unique situation of work overload and stress, with some missing or underreported data. There was no control arm as this was how the clinical protocol established at our center worked. Otherwise, the sample is big, and data comes from an expert referral center for COVID-19. A high incidence of COVID-19 is still making struggle many developing countries after repeated waves. This feasible proposal could certainly help to optimize resource use in those situations.
Overall, CXR is inexpensive, convenient in the ED, and strongly correlated with prognostic implications in COVID-19. Choosing which patients will benefit from more intensive observation and treatment in-hospital is an unmet need. Using the CXR triage model for patients with non-severe COVID-19 suspected pneumonia would help to identify those patients with early pneumonia and those without it who could be potentially discharged with a low complication rate. Other techniques like lung ultrasound could be used for the same purpose. Additionally, strategies like home hospitalization for selected patients can be considered to decongest the ED and wards.
ConclusionIn summary, CXR identified pneumonia in 60% of a series of symptomatic non-severe suspected COVID-19 patients without respiratory insufficiency presenting at the ED with possible pneumonia. Patients without radiological condensation had less mortality and were mostly discharged. Deceased patients were elder and with a higher Charlson index. The re-consultation rate was low compared to other series, developing pneumonia in 40% of bounce backs without previous pneumonia. CXR triage for suspected COVID-19 pneumonia in patients with CTAS/MAT IV–V in the ED could be useful to decongest urgent care facilities working at capacity during the pandemic.
FundingThis research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Conflict of interestNone.
Authors would like to acknowledge the collaboration and hard work in difficult times of rest of the Vall d’Hebron medical emergency group (Santiago Aranda-Rodríguez, Pablo Rodríguez De Vera-Marín, Cristina Marcos-Fosch, Begoña Santos-García de Vicuña, Lluís Jubany-Mari, Claudia Casellas-Montagut, Mireia López-Corbetó, Andrés Parra-Rojas, Isidro Sanz-Pérez, Marcelo Alvarado-Cárdenas, Cristina Pérez-Cameo, Paula Suanzes-Díez, Juan Espinosa-Pereiro, Luisa Roade-Tato, Pau Bosch-Nicolau, Jordi Navarro-Mercadé, Judit Vidal-González), ED staff (registered nurses, nurses, clerks) and all the other healthcare providers who transiently joined the ED.