Coronavirus disease 2019 (COVID-19) has become the most important public health issue worldwide due to its rapid spread, morbidity, and mortality. Although its main target is the respiratory system, a significant proportion of COVID-19 patients exhibits myocardial injury, which is associated with a worse in-hospital prognosis.1–3 The pathophysiological mechanisms related to cardiovascular affectation are not entirely understood but may be related to intense endothelial damage, inflammation, thrombosis, and coagulopathy.4 However, it is unknown if COVID-19 may affect the mid and long-term cardiovascular outcomes. We aim to describe the cardiovascular outcomes at six months following COVID-19 diagnosis.
This is a single-center, retrospective registry of all consecutive hospitalized patients who underwent a real-time reverse transcriptase-polymerase chain reaction (RT-PCR) for SARS-CoV-2 from March 1 to April 19, 2020, at the University Hospital Hospital Clínic, Barcelona, Spain. The study was approved by the Ethics Committee and adhered to the principles outlined in Helsinki's Declaration.
All information was obtained from electronic records (medical history and national social security database). Patients were divided into two groups according to the RT-PCR result to have a comparator arm. Rates of all-cause death and cardiovascular outcomes (cardiovascular death, acute coronary syndrome [ACS], stroke, heart failure hospitalization [HFH], and pulmonary embolism [PE]) were evaluated at 6-month follow-up and compared between groups. Endpoints were defined according to the Academic Research Consortium-2.5 A Cox proportional hazards model along with a Wald test was used for comparison of outcomes. A crude analysis was performed for all endpoints, and adjusted analysis was performed only for all-cause death. Kaplan–Meier curves were used to derive the event rates at follow-up and to plot time-to-event curves. Patients not eligible for six-month follow-up were considered at risk until the date of last follow-up, at which point they were censored. A two-side p-value <0.05 was considered statistically significant. All data were processed using the Statistical Package for Social Sciences, version 25.0 (SPSS Inc., Chicago, IL, USA).
A total of 865 individuals were included in the study, divided into 620 with COVID-19 and 245 without COVID-19. Patients with COVID-19 were older (59±18.6 years vs. 45±18.5 years, p<0.001), more frequently male (333 [53.7%] vs. 112 [45.7%], p=0.034), with higher body mass index (BMI) (27.5±5.0 vs. 24.2±5.0, p<0.001) compared with patients without. Furthermore, patients with COVID-19 had higher rates of hypertension (237 [38.2%] vs. 43 [17.6%], p<0.001), diabetes mellitus [94 (15.2%) vs. 6 (2.4%), p<0.001], and hypercholesterolemia [161 (26%) vs. 23 (9.4%), p<0.001] as compared to non-COVID-9 counterparts.
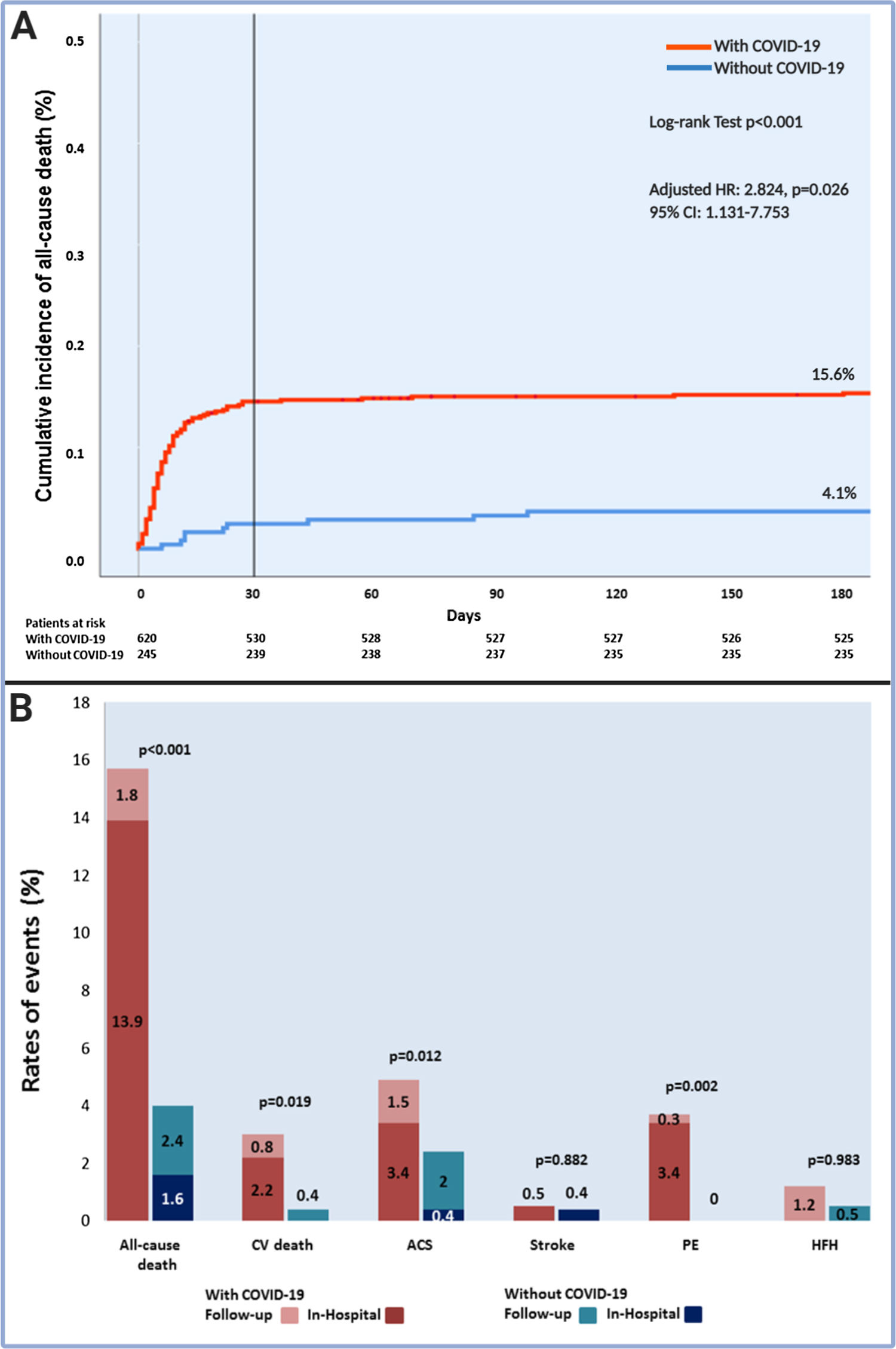
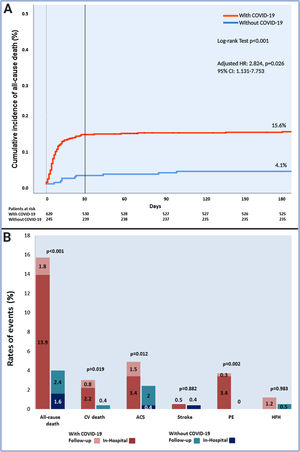
Patients with COVID-19 had a higher risk of all-cause death compared to those without (15.6% [97/620] vs. 4.1% [10/245], adjusted HR: 2.82, [95% CI: 1.13–7.75], p=0.026) (Fig. 1A). Of note, this difference was driven by a higher risk of in-hospital all-cause death (13.9% vs. 1.6%, un-adjusted HR: 9.10 [95% CI 3.34–24.80], p=0.001), with no differences in post-discharge risk of all-cause death between patients with or without COVID-19 (2.1% [11/534] vs. 2.5% [6/241], un-adjusted HR: 0.85 [95% CI 0.31–2.28], p=0.739). Furthermore, at 6-month follow-up, cardiovascular death and PE rates were higher in COVID-19 patients than those without. Nevertheless, these differences were due to a higher rate of in-hospital cardiovascular death (2.3% vs. 0%, p=0.018) and PE (3.4% vs. 0%; p=0.001), without differences in the post-discharge follow-up. The in-hospital ACS rate was higher in patients with COVID-19 than those without (3.4% vs. 0.4%, p=0.008). At 6-month, there were no differences in ACS between patients with or without COVID-19. Ultimately, there were no differences in stroke or HFH (Fig. 1B).
All-cause death and cardiovascular outcomes at six months follow-up in patients with or without COVID-19. (A) All-cause death time-to-event curve. (B) Six months follow-up cardiovascular outcomes. ACS, acute coronary syndrome; CV, cardiovascular; HFH, heart failure hospitalization; PE, pulmonary embolism.
At 6-month follow-up, we found a higher risk of all-cause death in COVID-19 patients. However, the difference between the groups was driven by a higher in-hospital all-cause death risk, without an increased risk during the post-discharge follow-up. Our data suggest that COVID-19 infection could be related to adverse acute cardiovascular outcomes without impaired outcomes beyond the disease's acute phase. Larger registries with extended follow-up must be performed to determine the long-term effect of COVID-19 on the cardiovascular system.
FundingThis study has been funded by Carlos III Institute, Madrid, Spain [Research grant COV20/00040].