Histiocytosis is a disease that is caused by the proliferation of the cells of the mononuclear phagocytic system in different tissues. Langerhans cell histiocytosis (LCH) is a type of histiocytosis that is not very prevalent in adults and is more common in children between the age of 1 and 3 years.
In 55% of cases, the infiltration of these cells is limited to a single organ; their systemic spread to other sites, such as bones, skin, lymphatic vessels, lungs, liver, spleen or central nervous system, is less common.1
The prognosis and treatment depend mainly on the patient's age and the number and dysfunction of the affected organs.
Here we report the case of an elderly female patient with a final diagnosis of LCH and exclusively colonic involvement.
81-year-old woman with a personal medical history of DM2, hypertension, hepatic steatosis and chronic grade IV ischaemia of the legs. On treatment with mixed insulin, ramipril, gemfibrozil and aspirin.1
She was admitted to gastroenterology for symptoms that appeared 2–3 months earlier,2 which included periumbilical and hypogastric postprandial abdominal pain, together with occasional vomiting. She did not report any changes in bowel movements or blood or mucous in stools. In addition, she had asthenia and a lack of appetite in recent months.
The patient was in a good general condition, clearly thin and with a slight mucocutaneous pallor. Her abdominal pain was diffuse on deep palpation, with no masses nor enlarged organs detected. Her legs showed signs of chronic venous insufficiency.
The lab test showed only a minimally elevated CRP and leukocytosis with no neutrophilia.
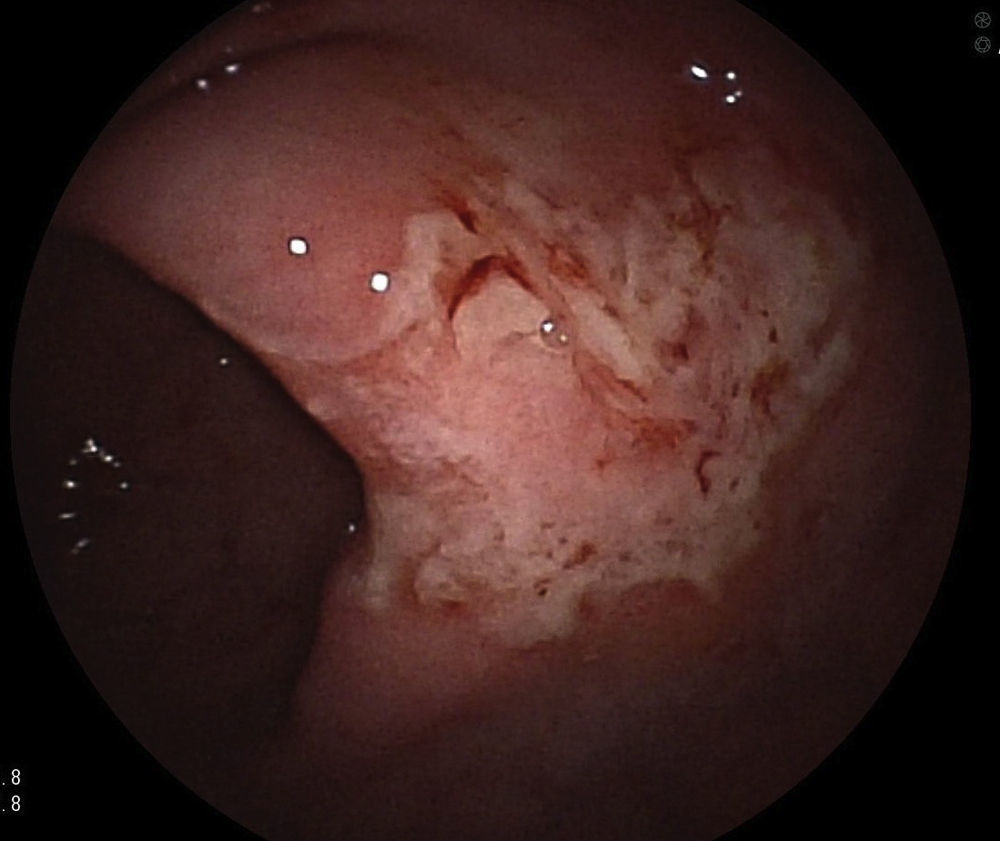
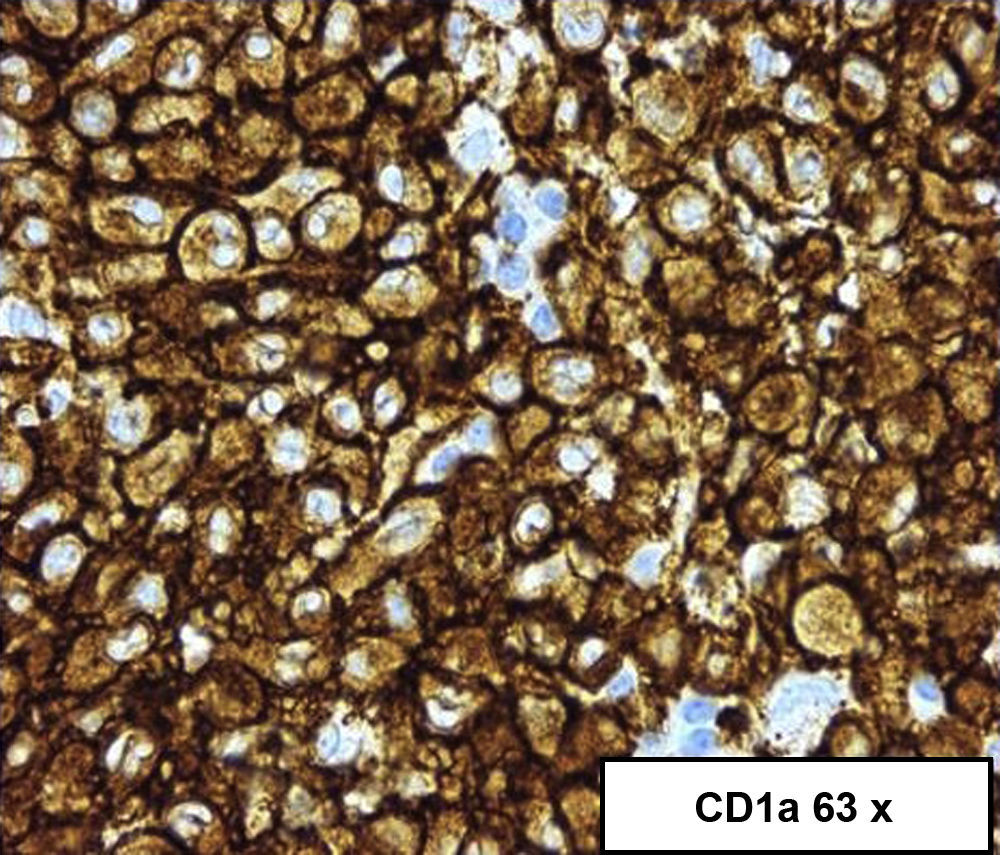
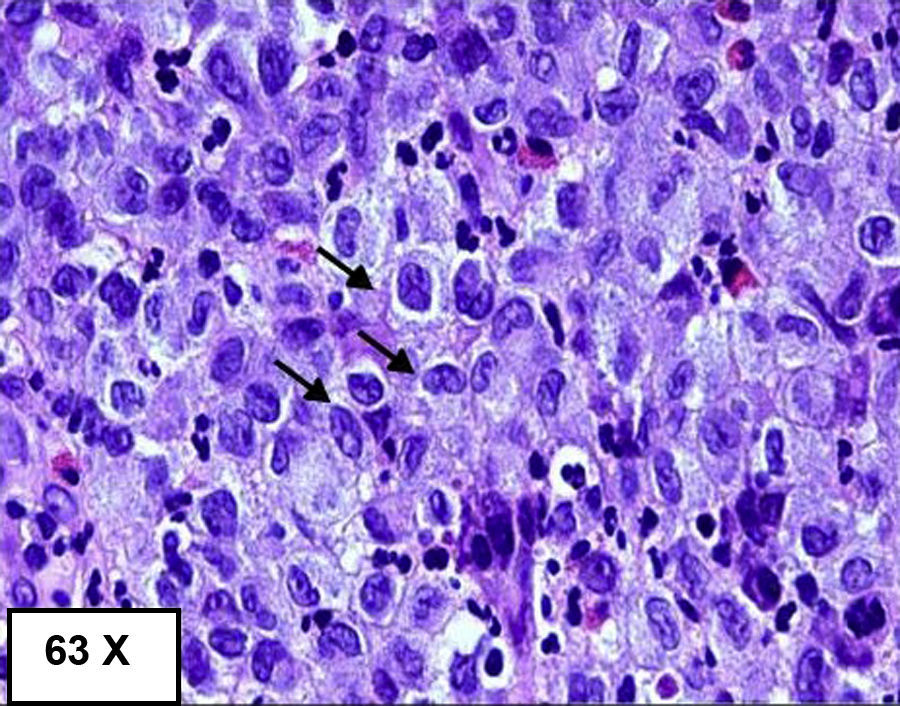
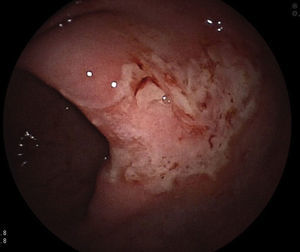
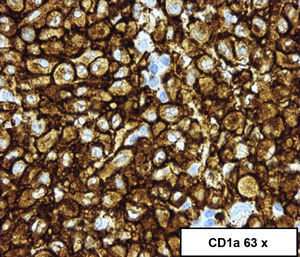
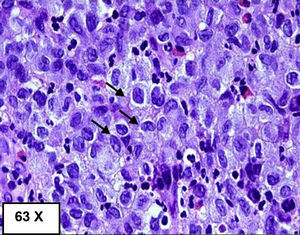
A colonoscopy was performed, observing, at 55cm of the anal margin (descending colon), mucosa with flat and superficial ulcerations, and some haemorrhagic suffusions, extending 10cm in length,3 the initial diagnosis of which was compatible with ischaemic colitis; however, the biopsy suggested a diagnosis of LCH (image of initial colonoscopy below: Fig. 1).4 The biopsy showed dense and diffuse cell proliferation of a neoplastic nature, with histiocytic cells, lobed nuclei and eosinophilic cytoplasm. The immunohistochemistry was positive for the S100 protein, vimentin, CD68 and CD1a.5 A second colonoscopy performed during the month of admission showed that the mucous membrane with the above-mentioned lesions was healing, with several small superficial ulcerations persisting.3
An abdominal CT scan showed that there was an increase in pericolic fat with wall thickening of the colon at the splenic angle. A chest CT scan and a bone scan with technetium-99m were performed, and the results were negative with regard to any involvement suggesting histiocytosis in other areas.
The final diagnosis was LCH affecting only the descending colon. The patient was therefore referred to haematology, where she was treated with corticosteroids, vinblastine for 6 weeks and 6-mercaptopurine for 12 months.
In the subsequent follow-up the patient showed clinical improvement, although since she has moved to another city we do not have a follow-up colonoscopy. Due to poor glycaemic control, it was decided to discontinue the corticotherapy after 6 doses of vinblastine and prednisone.
After 7 months of outpatient follow-up, the patient had improved considerably with the treatment.
LCH is present in most cases with isolated involvement of only one organ, but its systemic spread is less common. Gastrointestinal involvement is uncommon; solitary colorectal polyps are usually an incidental finding in asymptomatic patients. Only 2% of patients show symptoms of diarrhoea or poor absorption.2,3 There are few published cases on the exclusively colonic involvement of LCH, and most of them are about solitary colonic polyps.
Endoscopic examination and biopsies are required to confirm the presence of4,5 histiocytic infiltrate in mucosal cells, in addition to specific staining for CD1a and S100, or to demonstrate the presence of Birbeck granules in the cytoplasm with electron microscopy (Figs. 2 and 3).4,5
With the increase in the number of colonoscopies performed for other reasons, LCH should be considered as a rare cause of mucosal disease in the colon given its therapeutic and prognostic implications.
Please cite this article as: San Juan López C, Anguita Montes MF, Lázaro Sáez M, Gálvez Miras A, Hernández Martínez Á, Hallouch Toutouh S, et al. Histiocitosis de células de Langerhans en rango de edad poco frecuente. Gastroenterol Hepatol. 2017;40:505–506.