Intestinal intussusception is an uncommon disease in adults, with an incidence of 1–5%.1,2 The mean age of onset is 50, and there is a similar distribution between the sexes.1 Exceptionally, it presents as a bowel obstruction; such instances account for 1% of cases.1 In 90% of cases, it is linked to adherences or a Meckel's diverticulum, whereas in 10% its aetiology is tumoural. In 50–75% of cases, tumours causing intestinal intussusception are benign. Notable among these, in order of frequency, are lymphoid hyperplasia, lipomas, leiomyomas, haemangiomas and polyps. The most common malignant tumour is a metastatic tumour.3 The management of such tumours is debated, given the non-specific nature of the signs and symptoms and the discrepancy among complementary tests. Hence, diagnosis tends to be intraoperative.1,3
The following is a case report that illustrates the importance of a proper medical history and clinical suspicion in the management of a patient with a bowel obstruction caused by jejunal intestinal intussusception.
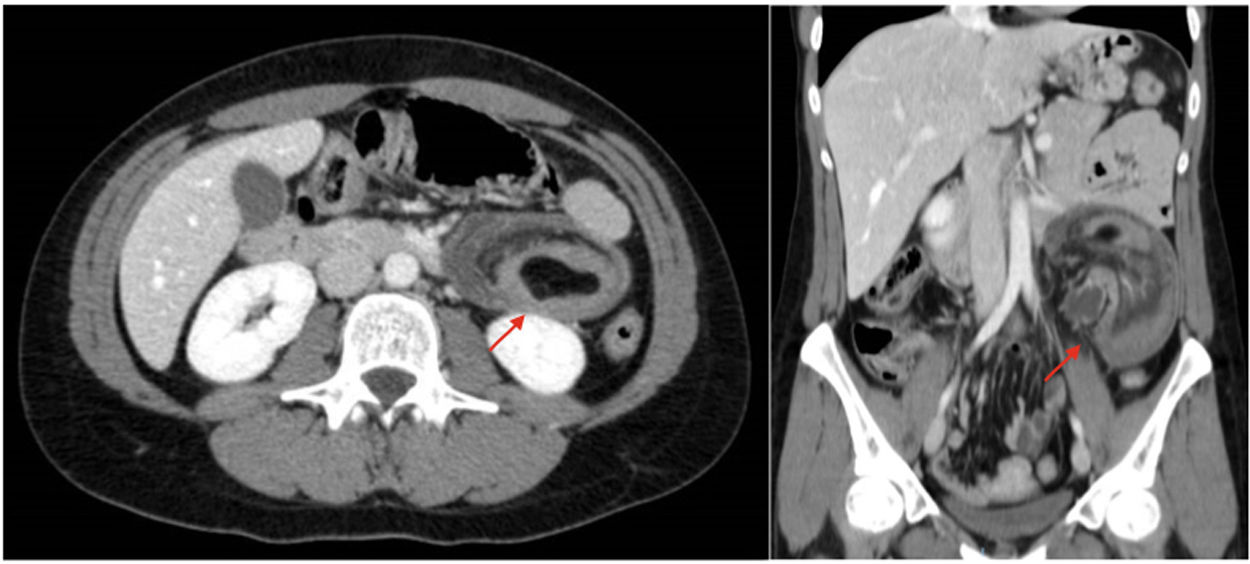
A 23-year-old woman with no prior history of note came in with abdominal pain, vomiting for four hours and gradual weight loss in the past year. She had experienced intermittent episodes leading her to seek emergency care on up to six different occasions. On those occasions, her signs and symptoms resolved with observation and treatment with non-steroidal anti-inflammatory drugs (NSAIDs). Examination found her to be in good general condition, with no fever, and haemodynamically stable. Her abdomen was slightly distended, with pain in all quadrants and without any peritonism or guarding. No mass or organomegaly was palpated. Laboratory testing showed leukocytosis (18,000/mm3) with neutrophilia and elevated PCR (190 mg/dl). A computed tomography (CT) scan revealed a tumour measuring 3 cm × 2 cm × 2 cm in the jejunum and signs of intestinal intussusception (Fig. 1). An emergency laparotomy showed a bowel obstruction secondary to intussusception of jejunal loops, mild signs of loop strangulation and an intraluminal lesion with a lipomatous appearance infiltrating the wall and protruding through the serosa. The intussusception was reduced, and after lukewarm normal saline was administered, the appearance and peristalsis of the bowel loops were restored. A jejunal resection was performed that included the tumour with clear margins and its mesentery, as well as an antiperistaltic mechanical laterolateral anastomosis for bowel transit reconstruction. The patient was discharged on the sixth day after surgery with no associated complications. The pathological workup confirmed the presence of an intraluminal lipoma in the resected segment measuring 4 cm × 3 cm × 3 cm, with no signs of malignancy and no lymphadenopathy. At present, the patient is asymptomatic.
The non-specific clinical presentation of intestinal intussusception in adults represents a diagnostic challenge, as few cases in the literature begin as a bowel obstruction.1,3 Signs and symptoms include intermittent and recurrent abdominal pain with weight loss and melaena at times, associated with normal complementary test results, which makes a definitive diagnosis difficult and also makes these patients high users of emergency departments.1 A differential diagnosis is made with acute appendicitis, since the most common location is enteroenteric (34%)4,5 and the pain tends to be concentrated in the right hemiabdomen.3,6 The preoperative diagnosis is based on an abdominal CT scan, though it is only confirmed in 20–25% of cases.1,3 Treatment of intestinal intussusception in adults consists of surgery, given the risk of malignancy and the possibility of bowel strangulation in an emergency situation, as in this case. Surgery should be planned based on the extent of the intussusception, the condition of the bowel loops, the nature of any tumour present and any mesenteric lymphadenopathy present, though in most cases it is a reaction to the inflammatory process.3 If it is confirmed in advance that the lesion is benign, then the resection should be as conservative as possible.1–3 When a tumour is of an uncertain nature with respect to disease, or malignancy is suspected in a context of prior weight loss and anorexia, en bloc resection should be performed, including removal of the bowel mesentery for a proper lymphadenectomy.1,3,6
In the case reported, the patient's medical history and the findings of her complementary and intraoperative tests were what led to resolving her emergency signs and symptoms and performing a complete tumour resection and associated lymphadenectomy, given the absence of a prior pathological workup and the risk of malignancy.
FundingNo funding was received for this work.
Conflicts of interestThe authors declare that they have no conflicts of interest.
Please cite this article as: Gómez-Sánchez T, Cerrato Delgado S, Camacho Marente V, Varela Recio J, Pacheco García JM. Obstrucción intestinal secundaria a invaginación yeyunal en el adulto. Gastroenterol Hepatol. 2021;44:228–229.