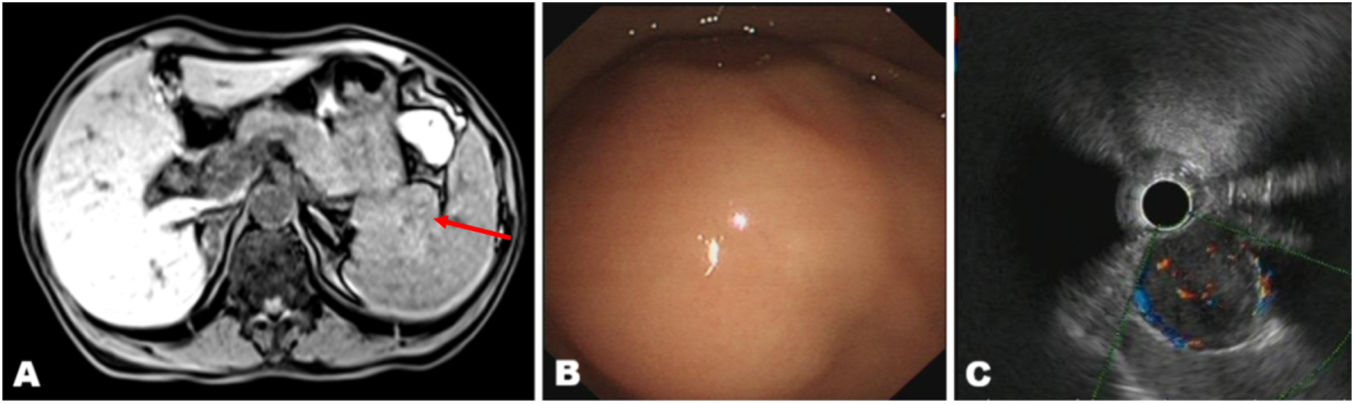
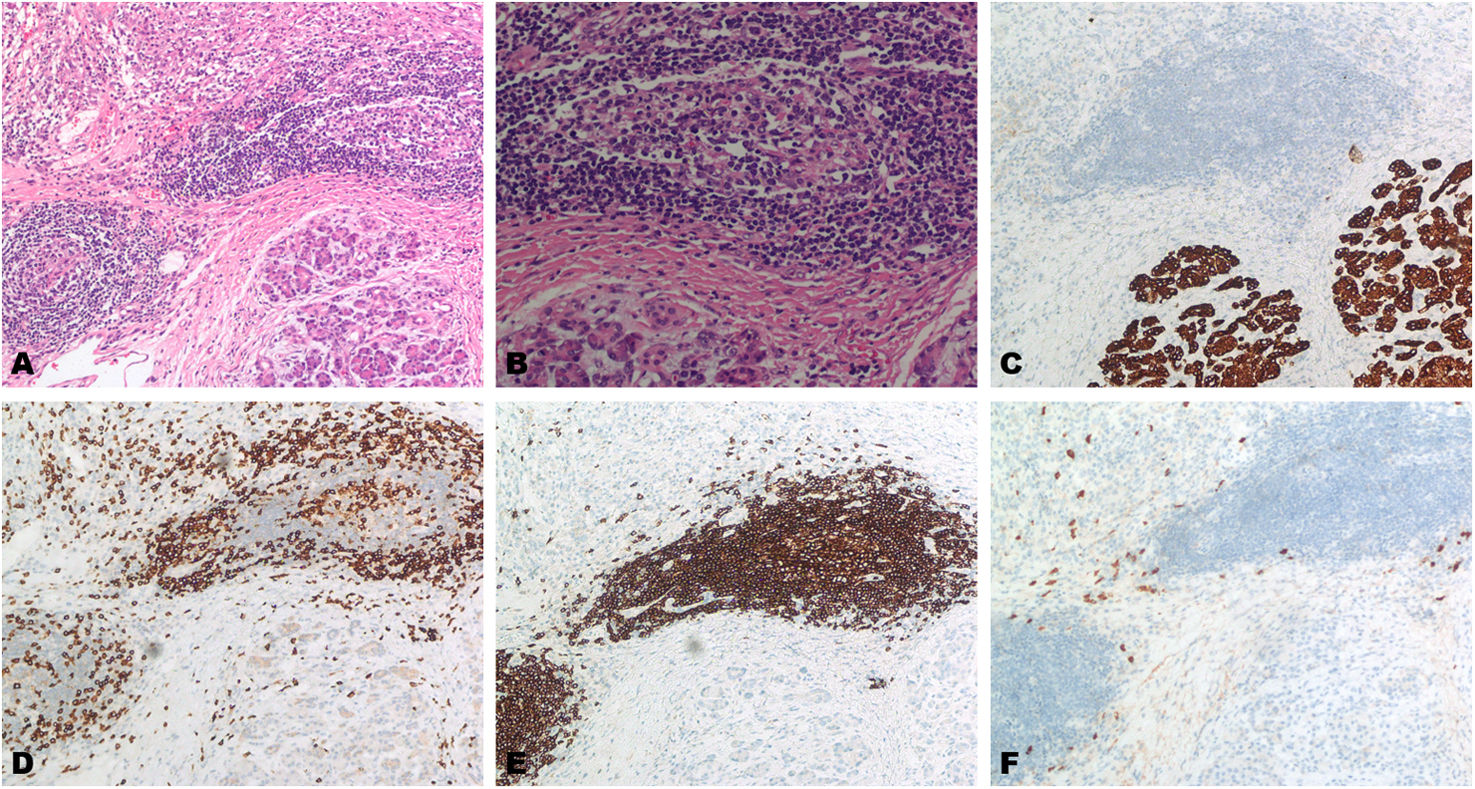
A 68-year-old woman presented with a one-month history of vomiting and diarrhea. Magnetic resonance imaging (MRI) revealed lesions in the pancreatic tail and splenic hilum, with heterogeneous enhancement after contrast administration (Fig. 1A). Endoscopic ultrasound (EUS) identified a large hypoechoic mass in the tail of the pancreas, with scattered internal calcifications (Fig. 1B and C). The laboratory examination shows that the tumor markers have not significantly increased, but the lesion still cannot be ruled out as malignant. Consequently, the patient underwent a laparoscopic distal pancreatectomy and splenectomy. Postoperative pathology confirmed chronic pancreatitis with significant fibrosis and lymphoid follicles (Fig. 2A and B). Immunohistochemical analysis revealed pancreatic tissue atrophy (PCK+) (Fig. 2C). The infiltrating lymphocytes were predominantly CD20+ B cells, alongside CD3+ T cells (Fig. 2D and E). IgG expression was less than 1% (Fig. 2F). Based on these findings, the patient was ultimately diagnosed with follicular pancreatitis. Follicular pancreatitis, a rare Th17-associated disorder, is often indistinguishable from pancreatic cancer preoperatively. Current expert criteria emphasize concurrent periductal lymphocytic infiltration and germinal center formation. Ultrasound-guided fine-needle biopsy may aid accurate diagnosis.1,2
Yu Lu and Qiu Wu collected the data and drafted the manuscript; Tao Yin revised the manuscript and conducted the study. All authors reviewed and approved the final manuscript.
Informed consentInformed consent was obtained from the patient for the publication of their information and image.
FundingNone declared.
Conflict of interestThere are none to declare.