Epistaxis in cirrhotic patients is a common issue. However, the literature published to date is very scarce.
Material and methodsRetrospective case series of patients with cirrhosis who presented with a significant epistaxis, between 2006 and 2016.
ResultsData were collected from 39 cirrhotic patients with a mean age of 61.4 (±14) years, 75% of which were males. The main comorbidities were hypertension (33%) and diabetes mellitus (26%). Seven (18%) patients were taking antiplatelet drugs and 3 (8%) anticoagulants. One third of patients had a previous history of epistaxis and 6 had a previous ENT pathology. The main aetiological factor of cirrhosis was alcohol in 46% of cases, with 15 (38%) patients presenting with Child A, 12 (31%) Child B and 12 (31%) Child C class. The median MELD score upon admission was 16 [12–21]. Thirty-five (97%) patients had portal hypertension. At admission, the median platelet count was 89,000 [60,000–163,000] and mean INR was 1.52 (±0.37). Clinically, epistaxis presented as haematemesis or melaena in 8 (21%) patients, simulating gastrointestinal bleeding due to swallowing of blood. In 10 (26%) patients, epistaxis was considered as the probable trigger of an episode of hepatic encephalopathy. Two patients required ICU admission due to bleeding and 8 (21%) died during hospitalisation due to causes not directly related to epistaxis.
ConclusionsEpistaxis is a complication to be taken into account in cirrhotic patients, as it can act as an encephalopathy trigger or simulate an episode of gastrointestinal bleeding.
La epistaxis en los pacientes cirróticos es un hecho frecuente. No obstante, la literatura publicada hasta la fecha es muy escasa.
Material y métodosSerie de casos retrospectiva de pacientes con cirrosis que presentaron una epistaxis significativa, entre los años 2006 y 2016.
ResultadosSe recogieron datos de 39 pacientes cirróticos con una edad media de 61,4 (±14) años, 75% varones. Las principales comorbilidades fueron la hipertensión arterial (33%) y la diabetes mellitus (26%). Siete (18%) pacientes tomaban antiagregantes y 3 (8%) anticoagulantes. Un tercio de los pacientes tenían antecedentes de epistaxis y 6 presentaban alguna patología ORL previa. La principal etiología de la cirrosis fue el alcohol en el 46% de los casos, siendo 15 (38%) pacientes Child A, 12 (31%) Child B y 12 (31%) Child C. La mediana de MELD al ingreso fue de 16 [12-21]. Treinta y cinco (97%) pacientes presentaban hipertensión portal. Al ingreso, la mediana de plaquetas fue de 89.000 [60.000-163.000] y la media de INR de 1,52 (±0,37). Clínicamente, en 8 (21%) pacientes la epistaxis se presentó simulando una hemorragia digestiva como hematemesis o melenas al ser la sangre deglutida. En 10 (26%) pacientes la epistaxis fue considerada como el probable desencadenante de una encefalopatía hepática. Dos pacientes requirieron ingreso en UCI por el sangrado y 8 (21%) fallecieron durante el ingreso, por causas no directamente relacionadas con la epistaxis.
ConclusionesLa epistaxis es una complicación a tener en cuenta, pudiendo actuar como desencadenante de encefalopatía o simular un episodio de hemorragia digestiva.
Epistaxis (from the Greek, literally “to drip”) is the term used to describe a haemorrhage or bleeding from the nostrils or paranasal sinuses, which exits through the nostrils or towards the mouth via the nasopharynx. The abundant vascularisation of the nasal passages and their special distribution in the thin nasal mucosa makes epistaxis very common in the general population, in the great majority of cases consisting of isolated and self-limiting episodes of little consequence. In extreme cases, or patients with significant comorbidity, however, it can become a life-threatening complication.1 The majority of episodes of epistaxis (90–95%) come from the Kiesselbach plexus, which is an area located in the anterior inferior part of the nasal septum, susceptible to mucosal dryness and probing by fingers. The remaining 5–10% of episodes originate from further back in the nasal cavity, from where the blood can drip into the oropharynx more easily and then be swallowed into the gastrointestinal tract.2
Epistaxis is the most common otorhinolaryngology emergency, with more than 25,000 cases a year in Accident and Emergency departments in countries like the United Kingdom. However, there is little scientific evidence on the subject and the first epistaxis clinical practice guidelines were only published very recently.3 Epistaxis is most commonly caused by trauma or hypertension, or it can be idiopathic; liver disease in general is a rare cause (<5%) of this type of bleeding in the general population.4
Patients with chronic liver disease are particularly susceptible to bleeding disorders and epistaxis.2 However, in recent years, we have witnessed a paradigm shift in the approach to coagulopathy in patients with cirrhosis. We now know that these patients have a very unstable balance between the different phases of haemostasis. This balance can be tilted towards a higher thrombotic risk, but also in special situations towards a higher bleeding risk.5 In certain disorders which often affect the liver, such as hereditary haemorrhagic telangiectasia (Osler-Weber-Rendu syndrome), nasal bleeding is a predominant symptom.6 However, recurrent epistaxis may also be the first symptom to suggest advanced chronic liver disease.7
Bleeding from the nasal cavity can be swallowed and manifest as gastrointestinal bleeding in the form of haematemesis and/or melaena. According to classic series8, this is the case in up to 0.5% of patients with suspected gastrointestinal bleeding. The differential diagnosis becomes even more important in patients with liver cirrhosis and oesophageal varices, as a massive epistaxis could be mistaken for variceal bleeding and cause significant delays in the appropriate treatment (or unnecessary treatment for the varices, with the consequent risk of iatrogenesis).9
The literature on epistaxis in patients with cirrhosis is fairly limited to date.10–12 In view of all the above factors, and the routine feeling in our clinical practice that this is not just an anecdotal problem, we decided to carry out this study to identify the clinical characteristics of patients with cirrhosis who had episodes of significant nasal bleeding while in hospital.
Material and methodsThis was a retrospective observational study which analysed a case series of patients with liver cirrhosis admitted to Hospital Universitario Ramón y Cajal in Madrid from 2006 to 2016 who had an episode of epistaxis while in hospital. A retrospective search was performed on the hospital discharge report software, which included the terms “cirrhosis”, “chronic liver disease”, “epistaxis” and “nasal bleeding”.
Demographic, clinical, analytical and treatment variables, and clinical outcome during the index admission for which they were included in the study were collected for all the enrolled patients. Patients whose episodes of epistaxis were managed in the Accident and Emergency Department and who were discharged from there were excluded.
The qualitative variables are expressed as absolute and relative frequencies. Quantitative variables with a normal distribution are expressed as mean and standard deviation, and all other variables as median and interquartile range. All statistical analyses were performed with Stata v13.0 software (StataCorp LP, TX, USA).
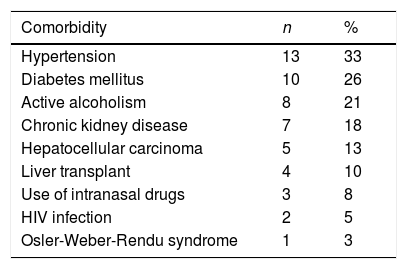
ResultsDuring the study period, 39 patients with cirrhosis met the search criteria and were included in the analysis. The mean age of the patients was 61.4 (±14 years), and 75% were male. The main comorbidities were hypertension (13 patients) and diabetes (10 patients). The most relevant comorbidities are shown in Table 1. In terms of usual medication being taken at the time of admission that might have played a part in the epistaxis, seven (18%) patients were on anti-platelet agents and three (8%) were on anticoagulants. Six (15%) patients were on treatment with beta-blockers.
Main comorbidities of the patients enrolled in the study (N=39).
| Comorbidity | n | % |
|---|---|---|
| Hypertension | 13 | 33 |
| Diabetes mellitus | 10 | 26 |
| Active alcoholism | 8 | 21 |
| Chronic kidney disease | 7 | 18 |
| Hepatocellular carcinoma | 5 | 13 |
| Liver transplant | 4 | 10 |
| Use of intranasal drugs | 3 | 8 |
| HIV infection | 2 | 5 |
| Osler-Weber-Rendu syndrome | 1 | 3 |
HIV: human immunodeficiency virus.
A third of the patients had a history of epistaxis and six had a significant ENT disorder in their medical history: two had external nasal trauma; one perforated nasal septum; one traumatic placement of a nasogastric (NG) tube in the Accident and Emergency Department; one granulomatous septal lesion; and one nostril angioma.
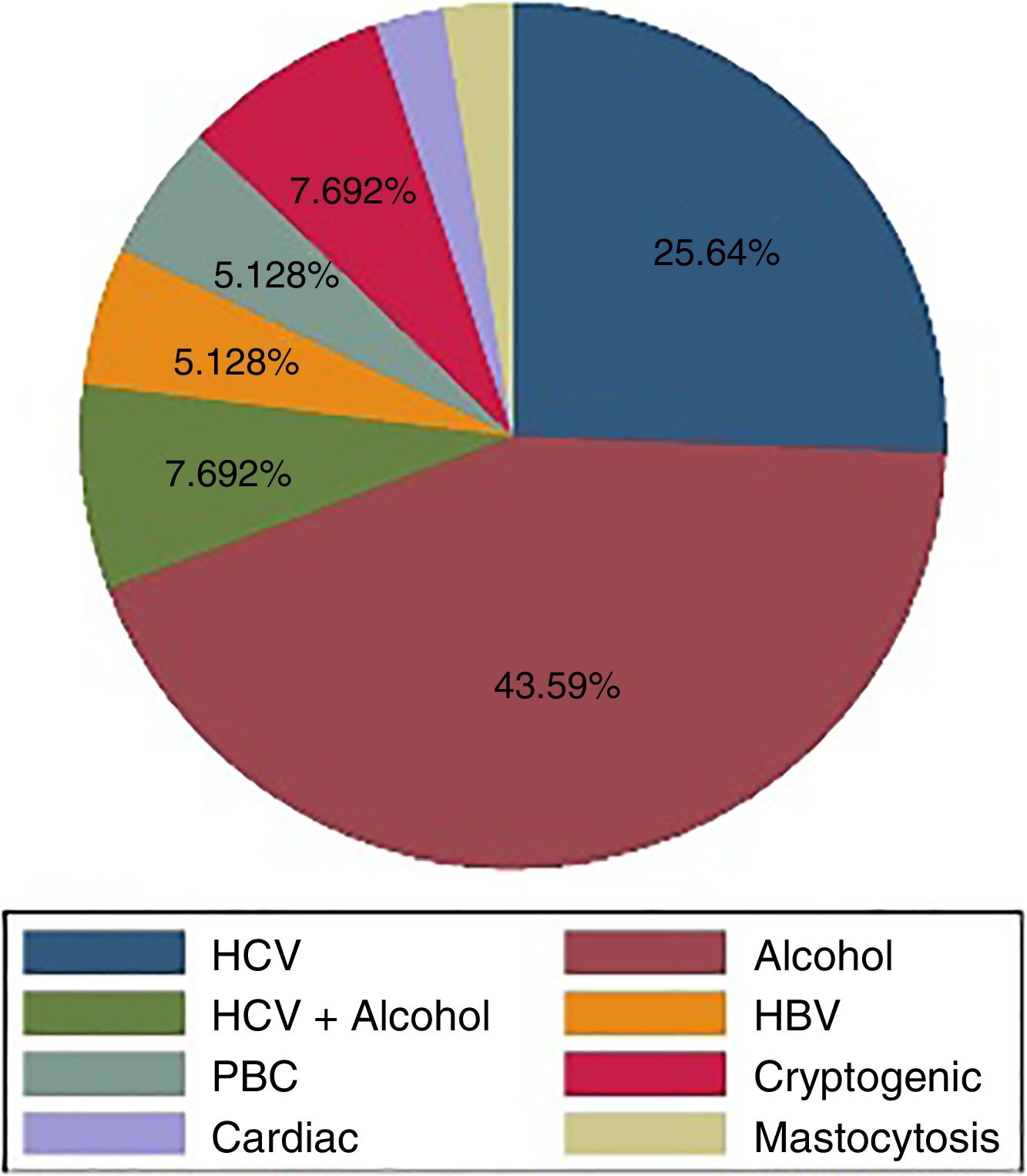
The main aetiological factor responsible for the cirrhosis was alcohol (44% of the patients). Fig. 1 summarises the associated aetiological factors. On admission, 15 (38%) patients were Child-Pugh class A, 12 (31%) Child-Pugh B and 12 (31%) Child-Pugh C. The median Model for End-Stage Liver Disease (MELD) score was 16 [12–21]. Thirty-five (97%) patients had some stage of decompensated liver disease: 25 ascites; 13 hepatic encephalopathy; and 6 bleeding from oesophageal varices. The median platelet count on admission was 89,000 [60,000–163,000] cells/mm3 and the mean INR was 1.52 (±0.37).
A one-third of the patients required transfusions of red blood cell concentrate (with an average of 1.3units per patient and a range of 0–9), two patients required transfusion of platelet concentrate and one patient required transfusion of fresh frozen plasma to correct their coagulopathy. The median length of hospital stay was 13 [6–24] days.
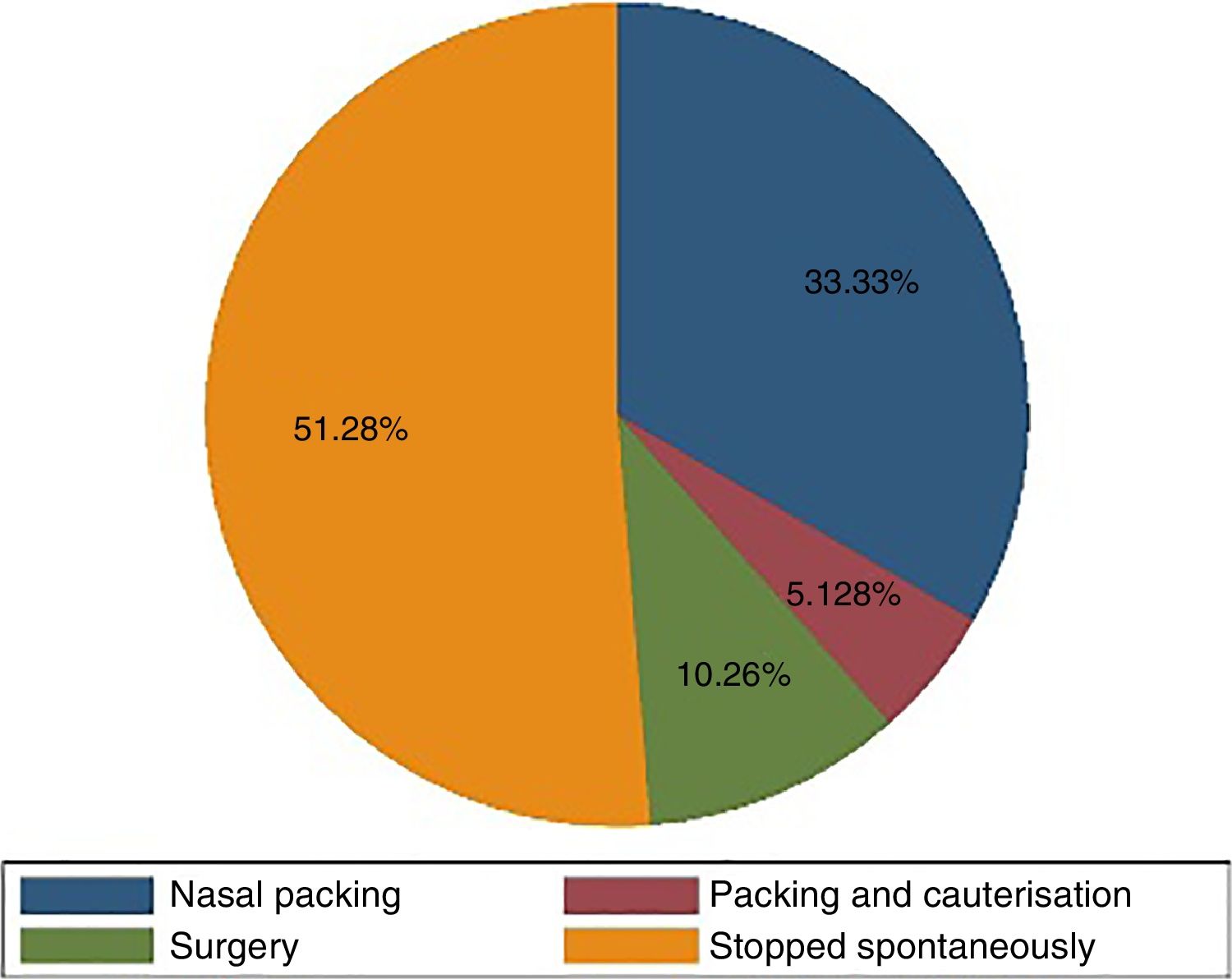
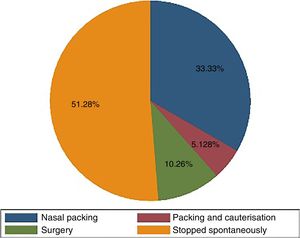
A one-third of patients already had epistaxis on admission. In the remaining two thirds, the epistaxis appeared during their hospital stay. Clinically, in 27 (69%) patients it presented as typical anterior epistaxis, in four (10%) as posterior bleeding and in eight (21%), as haematemesis or melaena as a result of the blood having been swallowed, simulating a gastrointestinal bleed. In ten (26%) patients, the epistaxis was thought by the treating medical team to be the probable trigger of hepatic encephalopathy (three of these ten patients had swallowed blood). The treatment applied to the epistaxis is shown in Fig. 2.
Two patients had to be admitted to the ICU because of the bleeding and eight (21%) died while in hospital, for reasons not directly related to nasal bleeding.
DiscussionAlthough it is a rare complication, epistaxis should be considered as a potential source of bleeding in patients with cirrhosis who present with upper gastrointestinal bleeding (UGIB) symptoms.
The largest series of patients with liver disease and epistaxis, only recently published, was based on a US national registry of hospital admissions.11 This population-based study included 1436 patients with liver disease who were compared with more than 38,000 patients without liver disease used as controls. The authors found that patients with epistaxis and liver disease were significantly younger (55.7 vs 67.5), had longer hospital stays (3.9 vs 3.2 days) and had more known risk factors for liver disease (alcohol abuse, coagulopathy, renal failure, etc.). They calculated a greater risk of transfusion and in-hospital mortality in patients with liver disease, with odds ratios of 1.52 (1.336–1.729) and 2.26 (1.372–3.736), respectively.
Camus et al. published a series,10 in which the study design makes it more similar to ours, from a reference centre for liver transplantation in Los Angeles,10 which included 461 patients with cirrhosis and registered in the database for UGIB. Epistaxis was considered as the origin of bleeding in 20 (4.3%) of these 461 patients. In our study which, being retrospective, only included cases of epistaxis confirmed in the hospital discharge report, evacuation of the blood as UGIB in the form of haematemesis and/or melaena was detected in eight (21%) of the total 39 epistaxis episodes.
These patients had advanced liver disease, two thirds of them being in Child-Pugh class B or C and 95% having had some type of complication related to portal hypertension. In the series by Camus et al., the patients also had very advanced liver disease, with 95% Child-Pugh class C, and an average MELD score of 29.6. Alcoholic aetiology predominated in both of these series, affecting approximately 50% of patients.
In the patient's previous medical history, it is important to identify particular comorbidities (hypertension, use of intranasal drugs), previous ENT disorders (present in a third of our patients) and nasal trauma, especially related to NG tube insertion attempts; although this was only recorded in one of our patients, it occurred in 80% of the cases in the American series. Careful consideration of the use of an invasive procedure with potential complications such as the insertion of an NG tube is even more important in patients with such advanced liver disease with marked thrombocytopenia and risk of nosebleed.13
It is interesting that only six patients (15%) in our series were on beta-blocker treatment when almost all of them had portal hypertension. Of these six patients, three had hypertension, four had oedema/ascites decompensation and one had a history of variceal UGIB. Considering the effect beta-blockers have on the systemic and portal circulation and the fact they are widely used in cirrhosis, it is possible that the lack of beta-blocker treatment in the rest of the patients of the series (85%) was a factor involved in the development of epistaxis.
Diagnosing epistaxis mimicking UGIB is complex. In addition to a high degree of suspicion, except in the very rare cases where the nasal origin is obvious from the clinical presentation, it requires an urgent oesophagogastroscopy to rule out bleeding varices. Bleeding that presents as haematemesis or melaena usually originates in the posterior nasal cavity, from where the patient is more likely to swallow the blood inadvertently. Another interesting finding from our series was that in a quarter of the patients, the blood ingested from the epistaxis was thought to have probably triggered an episode of hepatic encephalopathy.
Therapeutic management in most cases involved the help of an otolaryngologist and simple therapeutic measures such as nasal packing. In half of the cases, the bleeding stopped spontaneously and only 10% of the patients required more advanced measures such as surgery or embolisation of the bleeding vessel. This contrasts with the American series,10 in which up to 45% of patients presented with shock or hypotension, 75% required nasal packing and 10% arterial embolisation. However, the patients in that series had more advanced liver disease and coagulopathy.
Although there was only one death directly attributable to epistaxis in the American series and none in ours, because these patients have advanced liver disease, in-hospital mortality can be as high as 21% (25% in the American series).
The main limitation of our study is its retrospective nature, making it subject to multiple biases, such as only selecting cases which are potentially more serious (episodes included in the hospital discharge or death reports). Further prospective studies are needed to help better understand the characteristics of this potential complication of liver cirrhosis and to confirm the hypotheses generated here.
ConclusionsEpistaxis is a complication that must be considered in patients with chronic liver disease who present with symptoms of UGIB. It tends to affect patients with advanced cirrhosis and can on occasion act as a trigger for hepatic encephalopathy.
Conflicts of interestThe authors declare that they have no conflicts of interest.
Please cite this article as: Ferre Aracil C, Núñez Gómez L, Téllez Villajos L, Albillos Martínez A. Epistaxis en el paciente cirrótico: una complicación a tener en cuenta. Gastroenterol Hepatol. 2019;42:11–15.