To evaluate the acceptability/quality of abdominal ultrasound studies requested by primary care physicians in Barcelona; to develop ultrasound guidelines and assess their impact on acceptability.
MethodsDesign: 2-phase study, one retrospective, descriptive phase evaluating the acceptability/quality of requests (pre-intervention phase) and another to assess the impact of guidelines on acceptability/quality (post-intervention phase). Subjects: Requests for ultrasound studies from January-June 2010 from 10 primary care centers and the same number of requests from the same centers after the intervention. Variables. Pre-intervention phase: reason for consultation and request; presence of diagnostic orientation; results of ultrasound; acceptability/quality of the request. Intervention: design guidelines using the nominal group technique, dissemination of guidelines in the same centers. Post-intervention phase: three months after dissemination analyze the same number of requests assessing the same variables included in the pre-intervention phase.
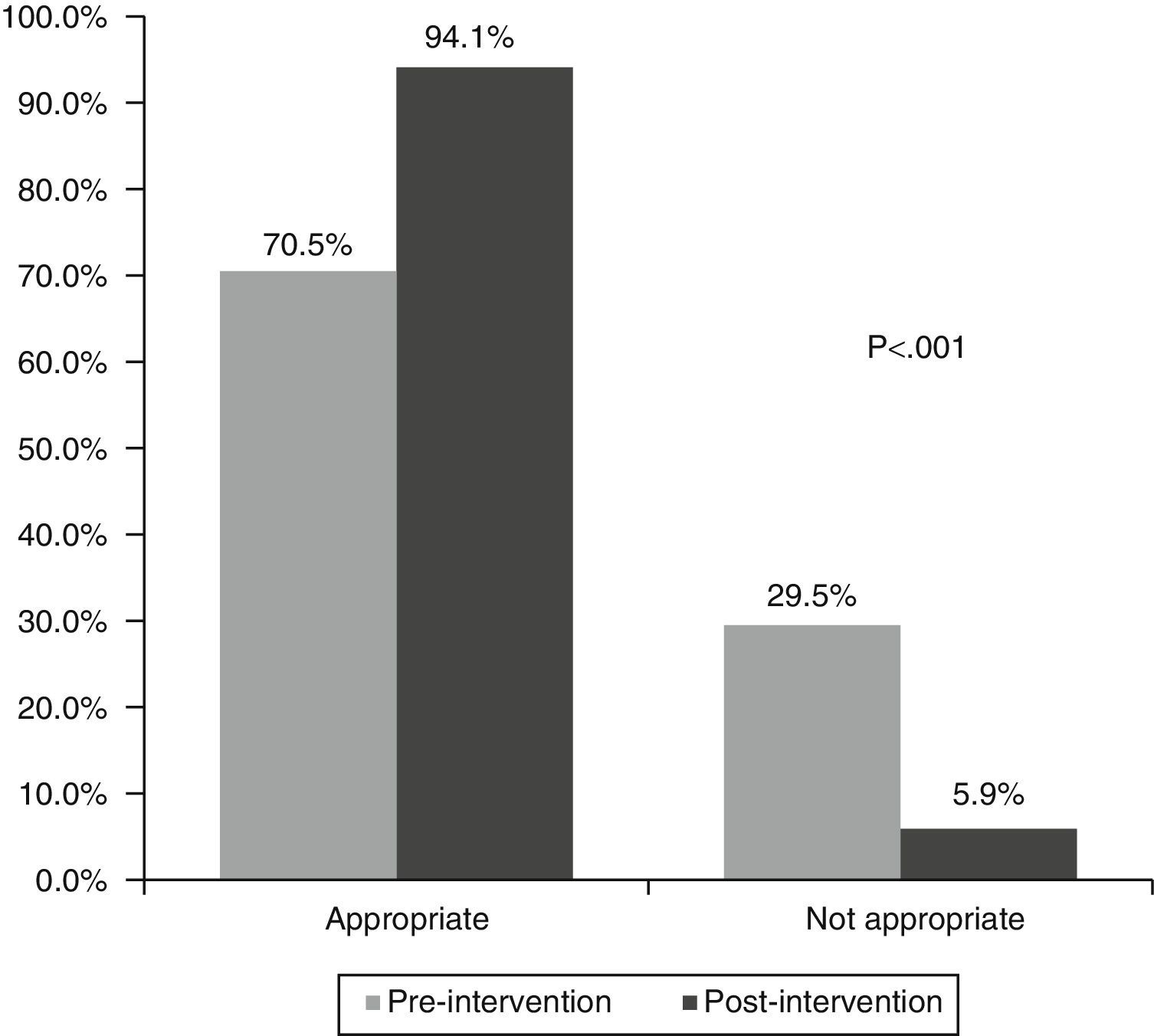
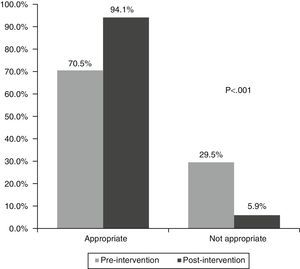
ResultsPre-intervention phase: 1,063 requests, 52.4% women, mean age 52±16years (range 11-94). Post-intervention phase: 1,060 requests, 57.6% women, mean age 54±17years (range 6-91). Main reasons for requests: abdominal pain/discomfort 38.3% (pre-intervention) and 43.1% (post-intervention). Diagnostic orientation in 14.5% (pre-intervention) and 40.8% (post-intervention). Normal ultrasound results in 46.0% (pre-intervention) and 42.3% (post-intervention). Good quality of requests in 42.7% (pre-intervention) and 46.5% (post-intervention). Acceptability of ultrasound: 70.5% (pre-intervention) and 94.1% (post-intervention). The better the quality of the request, the better the acceptability of the studies and the greater the number of pathological conditions identified.
ConclusionsGuidelines for ultrasound improve the quality of requests, diagnostic orientation and acceptability of the studies.
Evaluar la adecuación/calidad de las ecografías abdominales solicitadas por médicos de atención primaria de Barcelona, desarrollar una guía para la ecografía y evaluar su impacto en la adecuación.
MétodosDiseño: estudio en 2 fases, una descriptiva, retrospectiva, que evalúa la calidad/adecuación de las solicitudes (fase preintervención), y otra que evalúa el impacto en la calidad/adecuación gracias a la guía (fase postintervención). Sujetos: solicitudes de ecografías durante enero-junio del 2010 procedentes de 10 centros de AP y el mismo número de solicitudes provenientes de los mismos centros después de la intervención. Variables. Fase preintervención: motivo de la visita y petición; presencia de orientación diagnóstica; resultado de la ecografía; calidad/adecuación de la solicitud. Intervención: diseño de una guía mediante técnica grupo nominal y difusión de la guía en los mismos centros. Fase postintervención: 3 meses después de la difusión, analizar el mismo número de solicitudes evaluando las mismas variables que en la fase preintervención.
ResultadosFase preintervención, 1.063 solicitudes, 52,4% mujeres, edad media 52±16años (rango 11-94). Fase postintervención, 1.060 solicitudes, 57,6% mujeres, edad 54±17años (rango 6-91). Principales motivos de petición: dolor abdominal/molestias 38,3% (preintervención) y 43,1% (postintervención). Orientación diagnóstica en el 14,5% (preintervención) y el 40,8% (postintervención). Resultado de ecografía normal en el 46,0% (preintervención) y el 42,3% (postintervención). Calidad de las solicitudes buena en el 42,7% (preintervención) y el 46,5% (postintervención). Adecuación de ecografía del 70,5% (preintervención) y del 94,1% (postintervención). A mayor calidad de la solicitud, mejor adecuación y mayor presencia de patología.
ConclusionesLa guía de la ecografía mejora la calidad de las solicitudes, la orientación diagnóstica y su adecuación.
Abdominal ultrasound is a very valuable test in primary care (PC), as it enhances the clinician's diagnostic capability, allows serious disorders to be detected quickly, has no associated adverse effects or contraindications, is inexpensive, and provides useful information.1 Ultrasound is therefore the most cost-effective technique for the initial study of most patients with suspected abdominal problems,2 and for monitoring diseases that require periodic repetition of the ultrasound examination.3
Our healthcare system provides a good level of care, which means that more and more complementary examinations are requested in order to confirm clinical diagnoses. However, the high demand has exceeded the capacity of diagnostic radiology services, leading to long waiting lists, delay in performing tests and, consequently, delays in diagnoses and starting treatment. PC physicians, therefore, have an obligation to carefully assess whether all ultrasound requests are justified, and must state any clinical information that can guide the radiologist in the search for a likely pathological condition.4,5 This is because clinicians often request repeat tests with little clinical justification, and without considering whether the result will change their therapeutic approach.6
This situation prompted us to conduct a study to evaluate the appropriateness of abdominal ultrasound requests by PC physicians in our setting. In this study we also assess the quality of abdominal ultrasound requests, present a set of recommendations and criteria for indicating abdominal ultrasound drawn up by a panel of PC physicians and specialists, and evaluate the impact of implementing these guidelines on the quality and appropriateness of abdominal ultrasound requests.
Materials and methodsStudy designThe study was divided into 2 phases: a preliminary descriptive, retrospective phase that evaluated the appropriateness and quality of abdominal ultrasound requests (pre-intervention phase), and a second (post-intervention) phase that evaluated the extent to which dissemination of a protocol containing a series of recommendations and criteria for indicating abdominal ultrasound studies improved the appropriateness and quality of requests made by PC professionals.7
Study subjectsPre-intervention phaseAll abdominal ultrasound referrals (n=1063) made by 10 regional PC centres in the province of Barcelona to the Maresme department of radiology, the diagnostic radiology reference centre for these centres, between January and June 2010 were reviewed to obtain the total sample size of 1050 ultrasounds from different patients. This gave a level of precision of 6% or more, assuming maximum uncertainty (p=50%).
Post-intervention phaseOnce the guidelines had been drawn up, and professionals from the participating centres had been given the recommendations for requesting abdominal ultrasounds, all (1060) abdominal ultrasound requests in the period from June to December 2011 were collected, generally from patients other than those participating in the first phase (unpaired sample).
Variables and study phasesPre-intervention phaseAll abdominal ultrasound requests were analysed, and computerised patient medical records were accessed to collect the following variables:
- 1.
Patient details (sex, date of birth, PC centre to which they are assigned).
- 2.
Details of the consultation.
- a.
Date of consultation.
- b.
Reason for consultation and reason for requesting the ultrasound: abdominal pain and/or non-specific abdominal discomfort, biliary dyspepsia, repeated vomiting, abnormal liver function tests, or monitoring of chronic liver disease, biliary polyps, gallstones, haemangiomas, liver cyst, renal calculi and renal cyst.
- c.
Presence/absence of tentative diagnosis in the request.
- d.
Type of request: ordinary or urgent.
- a.
- 3.
Details of the abdominal ultrasound
- a.
Date of ultrasound and delay between request and actual test.
- b.
Ultrasound results: normal, fatty liver disease, gallstones, biliary polyps, calcifications or granulomas, abnormal hepatic ultrasound structure, haemangioma, hepatic cyst, renal calculi, renal cyst, others.
- a.
- 4.
Evaluation of the appropriateness and quality of the abdominal ultrasound request. The quality of the requests in both the pre-intervention and post-intervention phases were based on the Spanish Society of Radiology's “criteria for referral of patients to radiology services”.6 Therefore, and to avoid any errors in interpretation, the request forms had to be correctly and legibly filled in, clearly explaining the reason for requesting the examination and providing sufficient clinical information to enable the diagnostic radiologist to understand the tentative diagnosis or the problems to be resolved by the radiological examination. Since there is no validated classification in the literature, we rated requests according to the following criteria:
- -
Very good: detailed clinical information on why the patient came to the centre and a tentative diagnosis to explain why an abdominal ultrasound is indicated in this case.
- -
Good: sufficient clinical information on the reason for the consultation, without going into detail and with no tentative diagnosis.
- -
Poor: little or generic clinical information (e.g. bultoma, abdominal pain).
- -
Very poor: no information.
- -
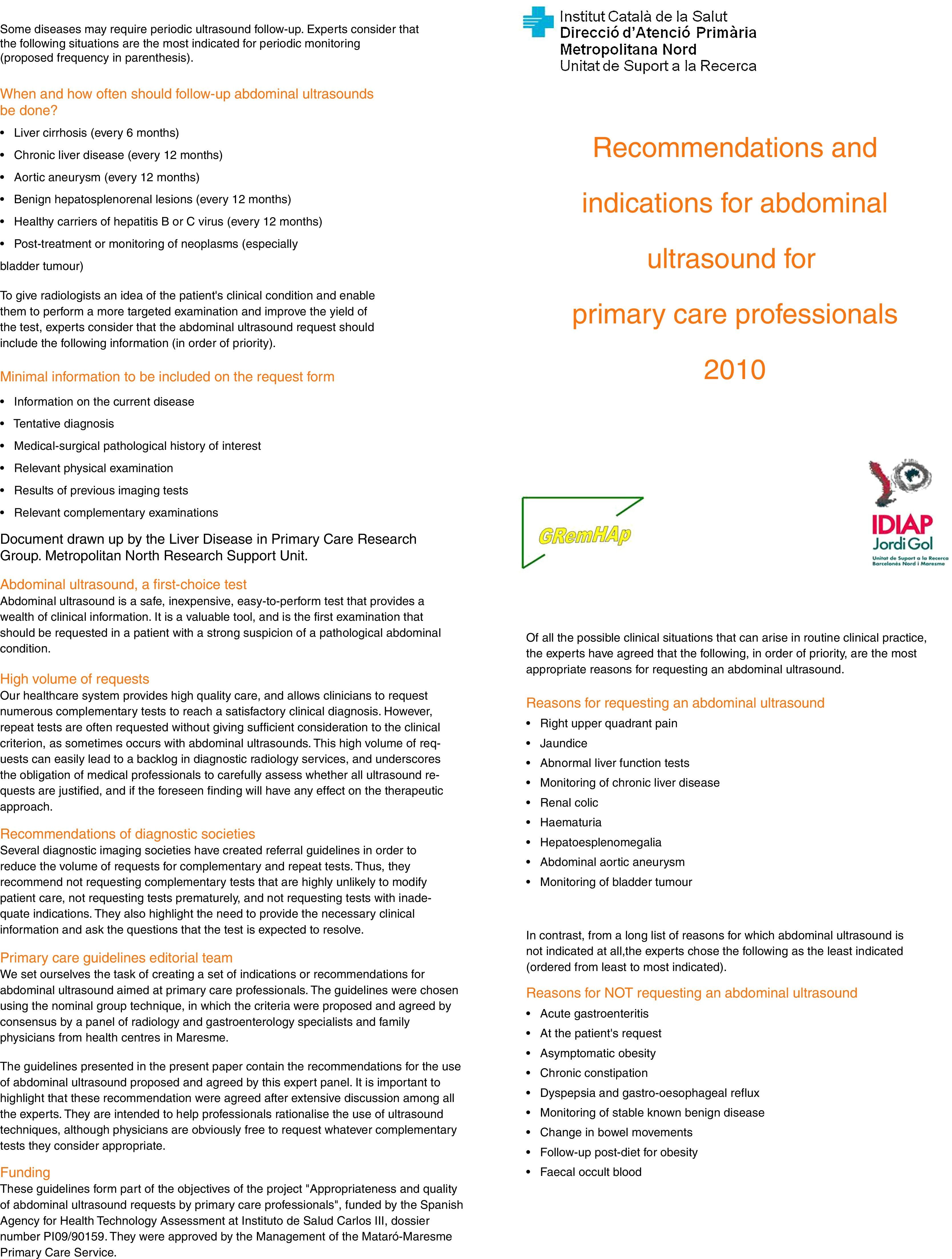
Design of consensus recommendations for abdominal ultrasound that clearly define the criteria for proper use of the diagnostic procedure. The methodology used was the consensus technique known as the “nominal group technique”,8 in which 4 family physicians, 4 gastroenterologists and 4 diagnostic radiology specialists met in a single session. The technique consists of asking some questions and, after several minutes of reflection, each member gives their answers independently, noting them on a flip chart. Each of the answers is then discussed briefly and grouped according to pathology, and conclusions are reached, choosing the responses with the highest score, up to a total of 10. The questions asked were: reasons for requesting an abdominal ultrasound; reasons for not requesting an abdominal ultrasound; minimal information that should be provided on an abdominal ultrasound request form; and when and how often follow-up abdominal ultrasounds should be performed. Appendix A, Annex 1 (Tables A1–A4) shows the responses to each of the questions. The consensus document was used to assess the appropriateness of the ultrasound requests in both the pre- and post-intervention phases.
The recommended criteria for indicating abdominal ultrasound were disseminated in meetings and sessions with the healthcare professionals in the different participating centres (one 60-minute session in each centre), and the guidelines were published in a leaflet (Appendix B, Annex 2; Fig. A1) and distributed to each of the physicians between January and May 2011.
Post-intervention phaseThree months after dissemination of the guidelines, the impact of the recommendations was estimated, based on the appropriateness of the ultrasounds and quality of the requests. To that end, we analysed 1060 abdominal ultrasounds from the physicians involved in the pre-intervention phase, and studied the same variables used in the pre-intervention phase.
Analysis planData were entered into an ACCESS database and then cleaned.
Univariate statistical analysis was performed on the quantitative variables (percentiles, mean and standard deviation) and qualitative variables (frequency and percentage). The Chi-square test and Fisher's exact test were used to compare qualitative variables in both phases, and the Student t-test and non-parametric Mann–Whitney test were used for quantitative variables. Statistical significance was established at p<0.05. Analyses were performed using statistical package Stata v12.
ResultsA total of 1063 abdominal ultrasounds (all from different patients) were evaluated in the pre-intervention phase. Of these, 557 corresponded to women (52%) and 506 to men (48%), with a mean age of 52±16 years (range 11–94). In the post-intervention phase, 1060 ultrasound requests were evaluated, of which 611 corresponded to women (58%) and 449 to men (42%), with a mean age of 54±17 years (range 6–91). The percentage of patients in the different participating centres was similar in each phase.
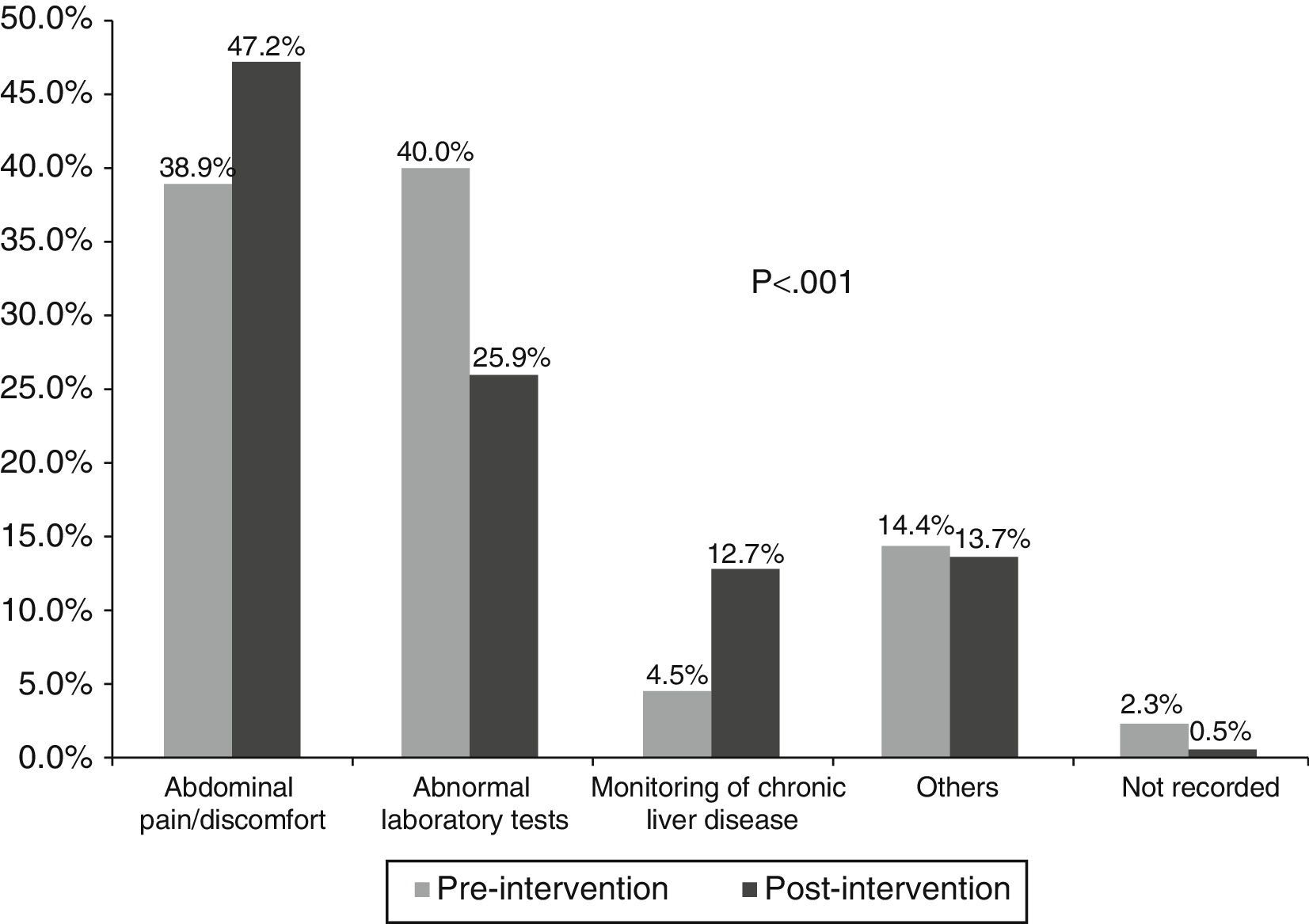
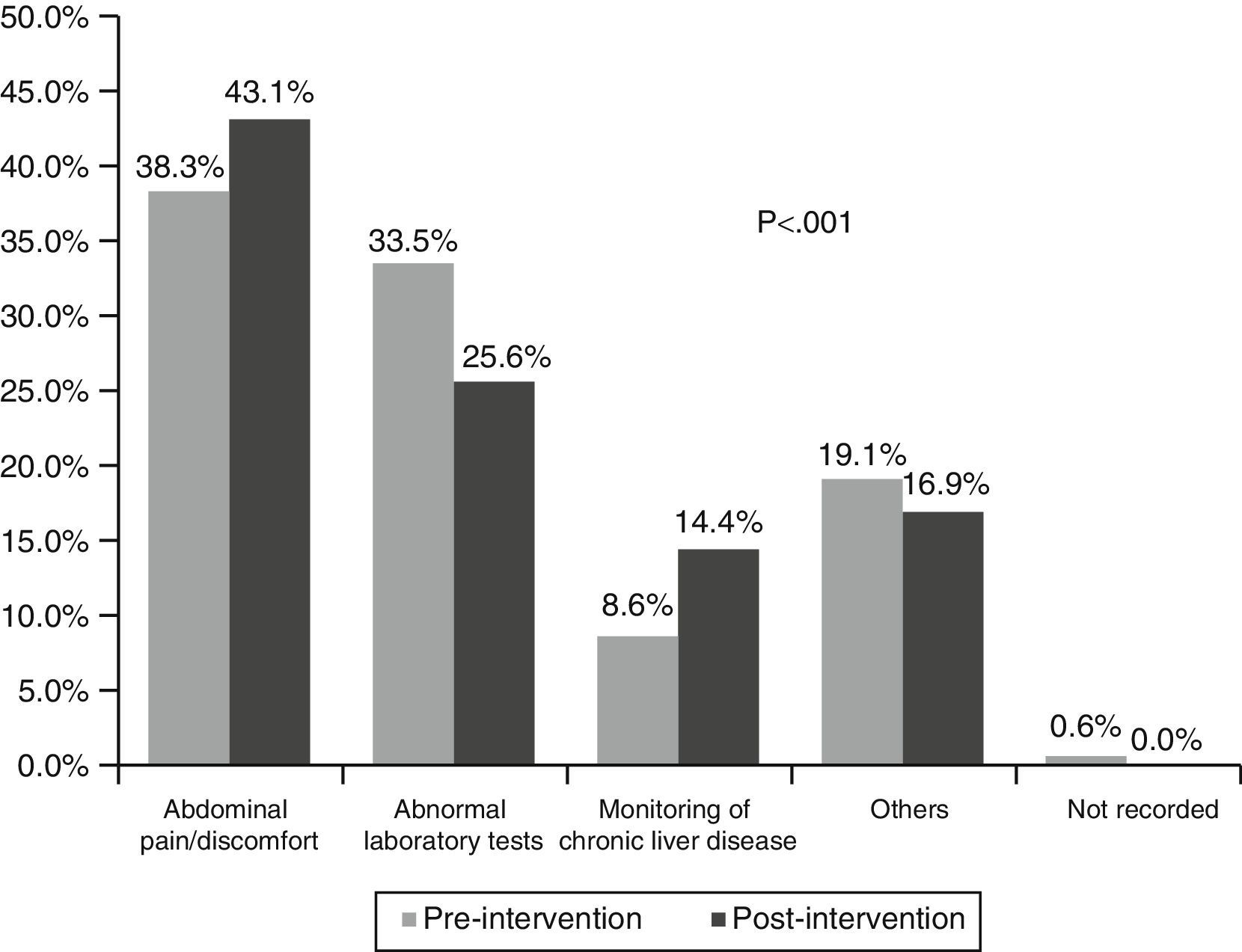
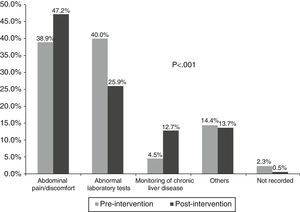
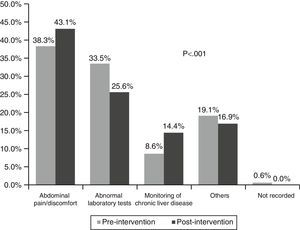
In the first phase, the main reason for consultation was abnormal liver function tests (40%), while in the second it was the presence of abdominal pain/discomfort (47%), p<0.001 (Fig. 1). The main reason for requesting abdominal ultrasound was abdominal pain/discomfort in both the first (38%) and second phase (43%), p<0.001 (Fig. 2).
In the pre-intervention phase, 14.5% of requests were referred with a tentative diagnosis, while in the post-intervention phase this increased to 40.8% (p<0.001). With respect to the type of request, in the pre-intervention phase, 1.8% of requests were for urgent ultrasound, compared to 5.0% in the post-intervention phase (p<0.001). The delay in performing the ultrasound was 33.6±17.1 days in the pre-intervention phase and 37.7±26.0 days in the post-intervention phase (p<0.001).
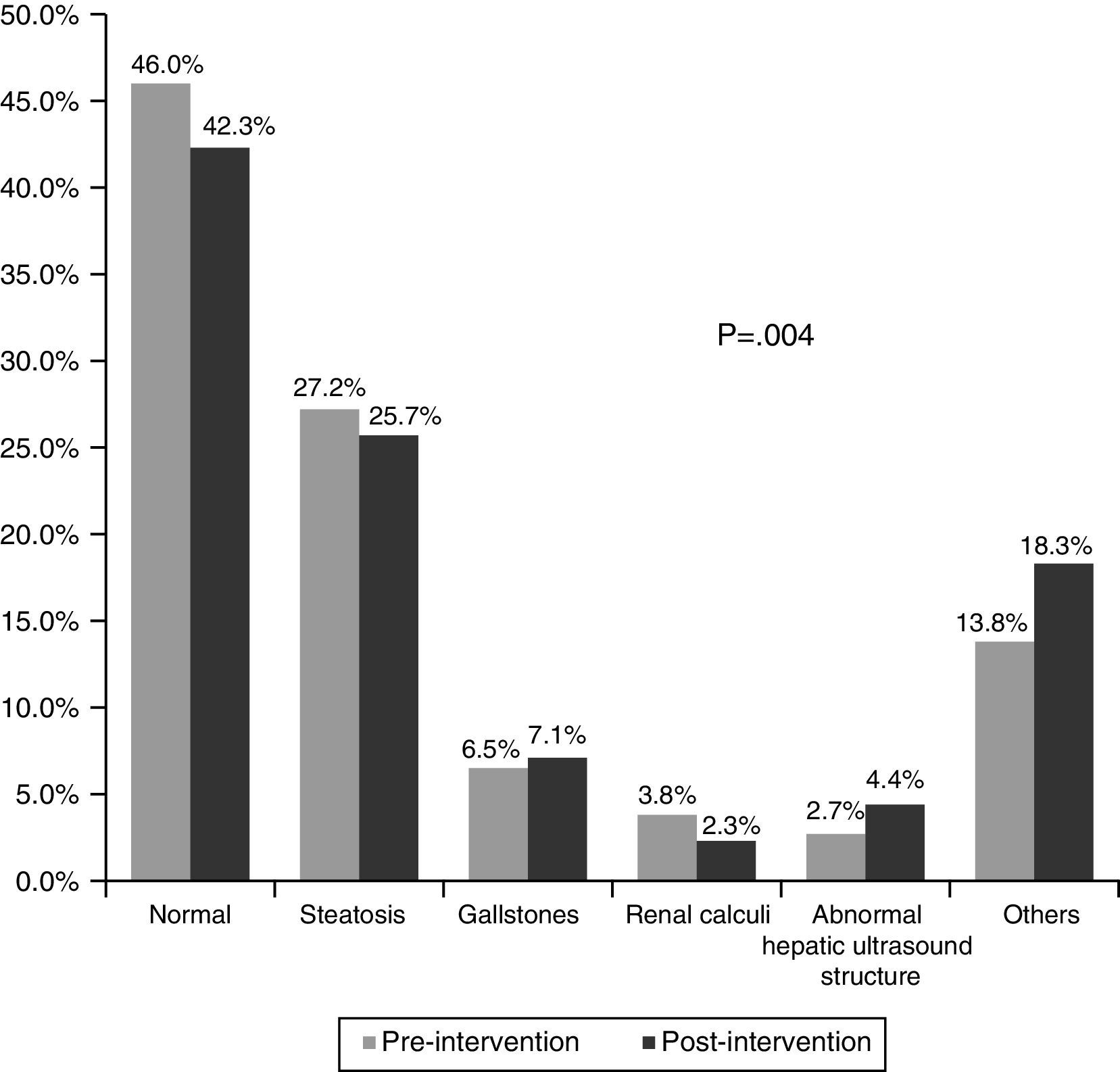
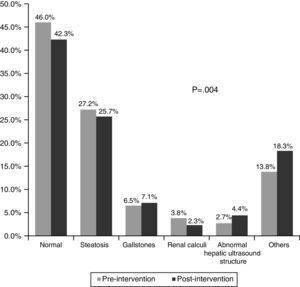
Fig. 3 shows the main results of the ultrasounds. These were normal in 46.0% of cases in the pre-intervention phase and in 42.3% in the post-intervention phase. The most common pathological finding was fatty liver disease, in 27.2% in the pre-intervention phase and 25.7% in the post-intervention phase (p=0.004). The other pathological findings were similar in both phases.
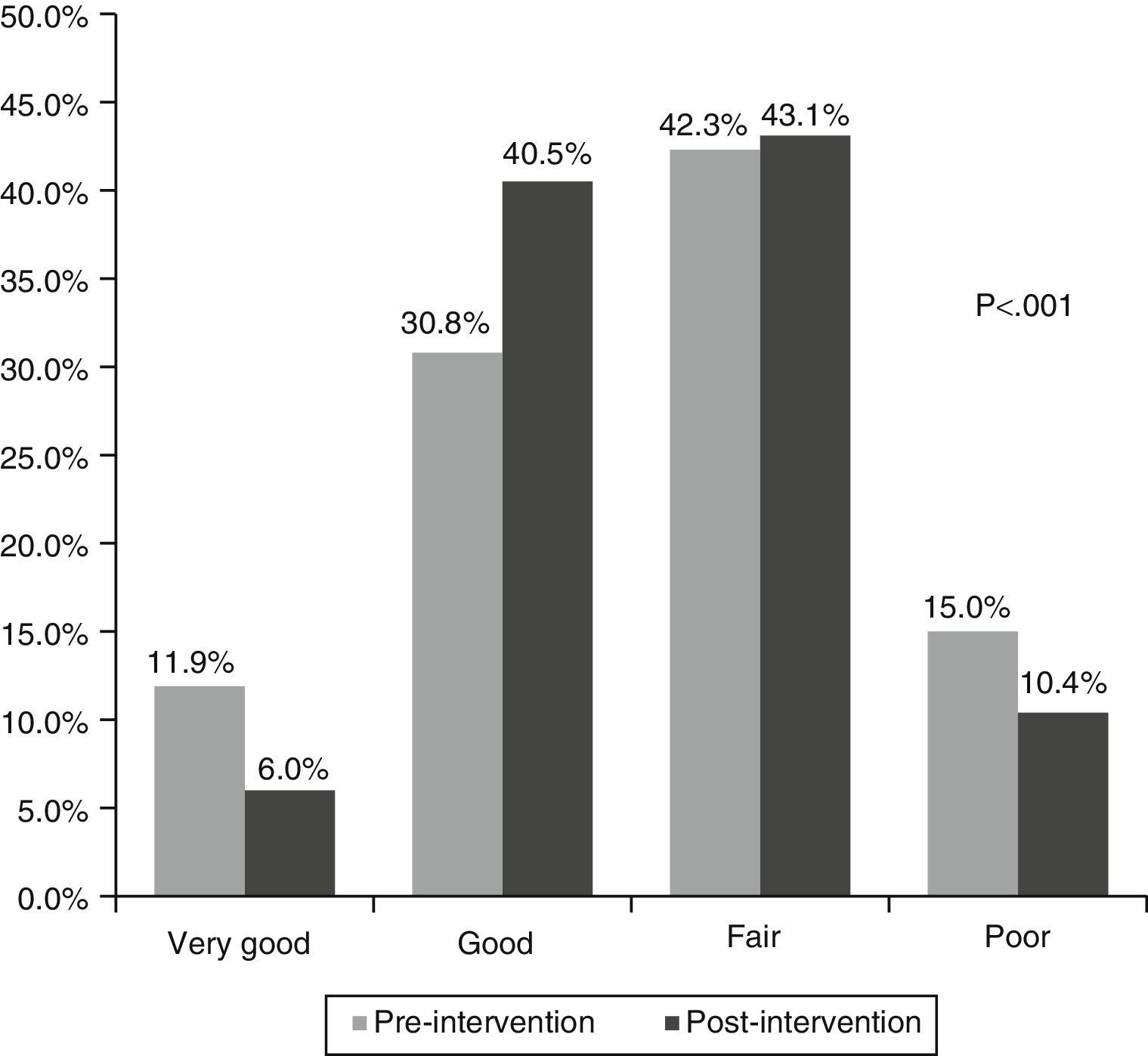
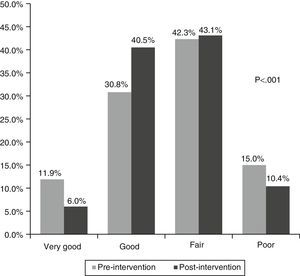
In terms of the quality of the requests, in the pre-intervention phase, 42.7% were good or very good, compared to 46.5% in the post-intervention phase (p<0.001). Fifteen percent of requests in the pre-intervention test were very poor quality, as they contained no information, compared to 10.4% in the post-intervention phase (Fig. 4).
Fig. 5 shows the appropriateness of the ultrasounds: 70.5% were appropriate in the pre-intervention phase and 94.1% in the post-intervention phase (p<0.001).
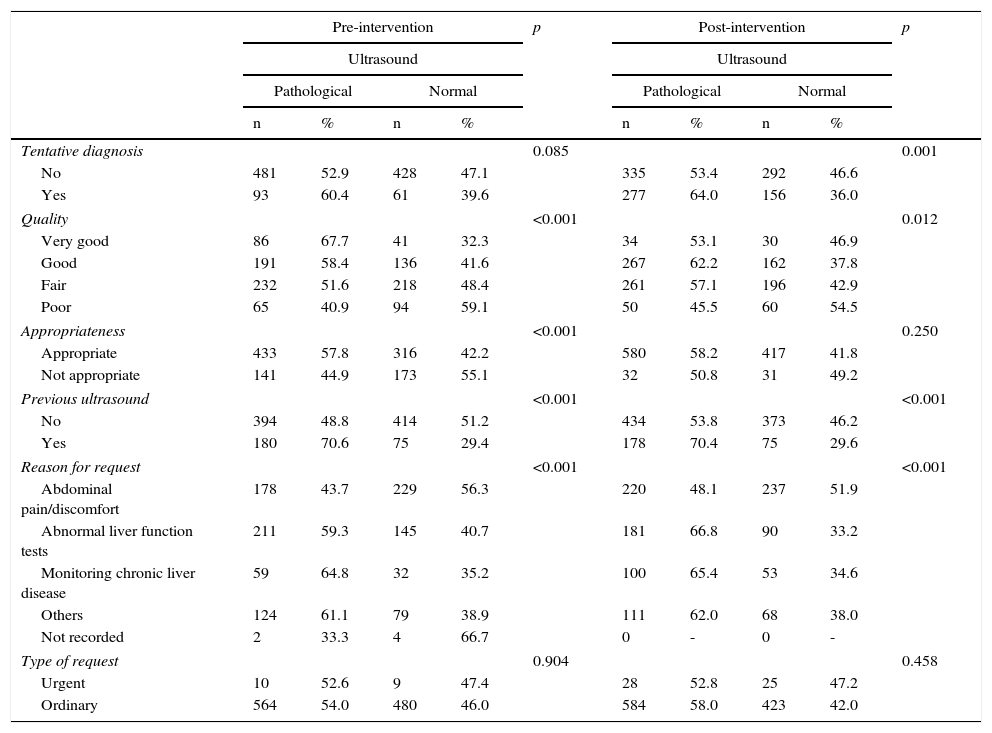
Table 1 shows the presence of a pathological condition on the ultrasound in relation to various aspects of the request, in both the pre- and post-intervention phase. Thus, according to the reason for the request, in patients with abdominal pain/discomfort, a pathological condition was found in 44% and 48% of cases in the first and second phases, respectively. A pathological condition was found in 59% and 67% of cases (pre- and post-intervention phases, respectively) if liver function tests were abnormal, and in 65% of cases in both phases if the request was for monitoring chronic liver disease (p<0.001). In requests with a tentative diagnosis, better quality and more appropriate requests were associated with a higher percentage of pathological results.
Relationship between the result of the ultrasound and the characteristics of the request.
| Pre-intervention | p | Post-intervention | p | |||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Ultrasound | Ultrasound | |||||||||
| Pathological | Normal | Pathological | Normal | |||||||
| n | % | n | % | n | % | n | % | |||
| Tentative diagnosis | 0.085 | 0.001 | ||||||||
| No | 481 | 52.9 | 428 | 47.1 | 335 | 53.4 | 292 | 46.6 | ||
| Yes | 93 | 60.4 | 61 | 39.6 | 277 | 64.0 | 156 | 36.0 | ||
| Quality | <0.001 | 0.012 | ||||||||
| Very good | 86 | 67.7 | 41 | 32.3 | 34 | 53.1 | 30 | 46.9 | ||
| Good | 191 | 58.4 | 136 | 41.6 | 267 | 62.2 | 162 | 37.8 | ||
| Fair | 232 | 51.6 | 218 | 48.4 | 261 | 57.1 | 196 | 42.9 | ||
| Poor | 65 | 40.9 | 94 | 59.1 | 50 | 45.5 | 60 | 54.5 | ||
| Appropriateness | <0.001 | 0.250 | ||||||||
| Appropriate | 433 | 57.8 | 316 | 42.2 | 580 | 58.2 | 417 | 41.8 | ||
| Not appropriate | 141 | 44.9 | 173 | 55.1 | 32 | 50.8 | 31 | 49.2 | ||
| Previous ultrasound | <0.001 | <0.001 | ||||||||
| No | 394 | 48.8 | 414 | 51.2 | 434 | 53.8 | 373 | 46.2 | ||
| Yes | 180 | 70.6 | 75 | 29.4 | 178 | 70.4 | 75 | 29.6 | ||
| Reason for request | <0.001 | <0.001 | ||||||||
| Abdominal pain/discomfort | 178 | 43.7 | 229 | 56.3 | 220 | 48.1 | 237 | 51.9 | ||
| Abnormal liver function tests | 211 | 59.3 | 145 | 40.7 | 181 | 66.8 | 90 | 33.2 | ||
| Monitoring chronic liver disease | 59 | 64.8 | 32 | 35.2 | 100 | 65.4 | 53 | 34.6 | ||
| Others | 124 | 61.1 | 79 | 38.9 | 111 | 62.0 | 68 | 38.0 | ||
| Not recorded | 2 | 33.3 | 4 | 66.7 | 0 | - | 0 | - | ||
| Type of request | 0.904 | 0.458 | ||||||||
| Urgent | 10 | 52.6 | 9 | 47.4 | 28 | 52.8 | 25 | 47.2 | ||
| Ordinary | 564 | 54.0 | 480 | 46.0 | 584 | 58.0 | 423 | 42.0 | ||
p, p value of a Chi-square test comparing the presence/absence of a pathological result according to the various categories of variables studied.
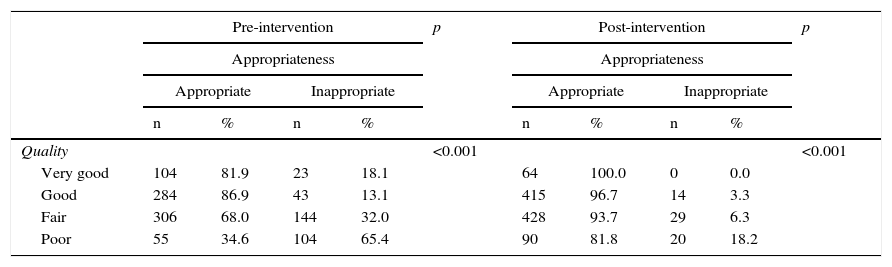
Finally, Table 2 shows the relationship between the quality of the ultrasound request and its appropriateness. As can be seen, better quality was significantly associated in both phases with a more appropriate request (p<0.001), especially in the post-intervention phase.
Relationship between the quality of the ultrasound request and its appropriateness.
| Pre-intervention | p | Post-intervention | p | |||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Appropriateness | Appropriateness | |||||||||
| Appropriate | Inappropriate | Appropriate | Inappropriate | |||||||
| n | % | n | % | n | % | n | % | |||
| Quality | <0.001 | <0.001 | ||||||||
| Very good | 104 | 81.9 | 23 | 18.1 | 64 | 100.0 | 0 | 0.0 | ||
| Good | 284 | 86.9 | 43 | 13.1 | 415 | 96.7 | 14 | 3.3 | ||
| Fair | 306 | 68.0 | 144 | 32.0 | 428 | 93.7 | 29 | 6.3 | ||
| Poor | 55 | 34.6 | 104 | 65.4 | 90 | 81.8 | 20 | 18.2 | ||
p, p value of a Chi square test comparing the appropriateness of the ultrasound with the quality of the request.
Abdominal ultrasound, being a safe, inexpensive, easy-to-perform test that provides a wealth of information, is a valuable clinical tool, particularly at the PC level. It is the first examination that should be requested in a patient with a strong suspicion of a pathological abdominal condition. However, the widespread availability of this test greatly increases the number of examinations requested, some of them unjustified, prompting several diagnostic imaging societies to create referral guidelines to address this problem.9–13 According to these guidelines, clinicians should not request complementary tests that are highly unlikely to modify patient care, should not request tests prematurely, and should not request tests with inadequate indications; at the same time, they underscore the need to provide the necessary clinical information and ask the questions that the test is expected to resolve.
With this aim, we decided to create a set of indications and recommendations for abdominal ultrasound for PC professionals using the nominal group technique,18 in which a panel of experts in diagnostic radiology, gastroenterology and family medicine agreed on the different criteria to be included. The guidelines presented in the present paper contain the recommendations for the use of abdominal ultrasound proposed and agreed by this expert panel. They are intended to help professionals rationalise the use of ultrasound techniques, although physicians are obviously free to request whatever complementary tests they consider appropriate.
Many abdominal ultrasounds are requested in our catchment area, sometimes without any justification, and less than half of these requests can be considered to be good quality; the most striking feature was that 15% and 10% of requests in each study phase were of very poor quality, as they contained no clinical information.
A poor quality ultrasound request could lead the radiologist to make mistakes in assessing the findings. For this reason, requests should be correctly and legibly filled in, clearly explaining the reason why the examination is requested and providing sufficient clinical information to allow the diagnostic radiologist to understand the tentative diagnosis or the problems to be resolved by the ultrasound.6,14,15
Few studies have analysed abdominal ultrasound requests referred by PC physicians to radiology services; however, the available data show that pathological changes are found in only 30% of ultrasounds, and that the diagnostic yield could be improved if the requests included relevant clinical information.16 A recent study observed that 12.1% of abdominal ultrasound requests were not justified, and that they lacked sufficient information that could give some orientation regarding the problem for which the examination had been requested.15 In this respect, the introduction of recommendations and criteria for indicating imaging tests in general–and abdominal ultrasound in particular–is thought to reduce the number of requests by between 25% and 30% and improve the criteria for indication.17,18 In our study, following introduction of the guidelines, the percentage of poor quality requests fell from 15% to 10%; the presence of a tentative diagnosis increased from 15% to 41%; and the appropriateness of the ultrasound increased from 71% to 94%, showing that the better the quality, the more appropriate the request. We also observed that improving the quality and appropriateness of requests resulted in a higher percentage of pathological conditions detected, thus enhancing the effectiveness of the process.
In order to prevent the inappropriate use of diagnostic imaging techniques, diagnostic radiology societies in both the United Kingdom and Spain6,14,19,20 have drawn up guidelines for referring patients to diagnostic imaging services in order to unify referral criteria, as complementary tests are useful when the results–whether positive or negative–help to modify the clinician's diagnostic and therapeutic approach. In this respect, in 2003 the Catalan Institute of Health asked a group of experts to draw up a set of recommendations and criteria for indicating computed tomography (CT) and magnetic resonance imaging (MRI); the implementation of these guidelines had a positive effect on improving indications and reduced the number of referrals.21 Guidelines can clearly be very useful, as shown in our study, but previous studies have shown that clinicians tend to ignore them and do not follow the recommendations.2,16,22 Failure to follow guidelines is more prevalent in the case of ultrasounds than in CT or MRI scans.16,22
In our study, the main reasons for consultation or requesting abdominal ultrasound were abdominal pain or discomfort, abnormal liver function tests and, to a lesser degree, monitoring of chronic liver diseases. In a significant percentage of these scans, the ultrasound result was normal in both the first (46%) and second phase (42%). Studies have shown that the higher the quality of the request, the greater the chance of detecting a pathological condition. This is important, because in many patients with abdominal discomfort, very little information was provided, and in these cases the percentage of normal results was higher. These findings are similar to those of a recent study.15 Therefore, we believe that it is important to select patients who could benefit both diagnostically and therapeutically from this examination. In this respect, an interesting cohort study was conducted in Holland in 2003–2004, which included a total of 76 PC physicians and 396 patients. The study objectives were to quantify the influence of positive and negative abdominal ultrasound findings on changes in therapy and patient management. The most relevant results were a change of therapeutic approach in 64% of cases, a significant reduction in the number of referrals to a specialist (from 45% to 30%) and more frequent reassurance of the patient by their PC physician (from 15% to 43%).23
Finally, an interesting development has been the recent publication of studies echoing the recommendations made by various radiology and family medicine societies that family physicians receive training in the diagnostic use of abdominal ultrasound, and even that this be included in specialist training programmes.18,24–26 This would be particularly interesting for simple complaints where the family doctor would be able to confirm or rule out the presence of disease, and would speed up both diagnosis and treatment, avoid referrals, and reduce the number of examinations in diagnostic radiology departments. It is clear that this will involve specifying objectives, both in terms of clinical practice and training requirements.27
Our study has some limitations that should be mentioned. Firstly, one of the problems encountered was to define the concept of quality in the context of the abdominal ultrasound request. As we were unable to find any information regarding this in the literature, we based our definition on the 4 categories described in the methodology, after having carried out a pilot study on 100 requests. Obviously, other criteria could be defined, but we believe that those used in this study would enable us to classify the quality of the requests in a valid and simple manner. Secondly, we were unable to differentiate between new and repeat ultrasound scans; therefore, a pathological finding may not have been newly identified, but might have been diagnosed previously. Although we did not have this information, a pathological finding on ultrasound does not necessarily indicate a good quality request. Thirdly, the study was based on abdominal ultrasounds related with abdominal disease; however, since they were sometimes requested for monitoring renal calculi and polyps, or for studying renal function, we included the results derived from these conditions. Lastly, although ultrasound requests were collected at different times of the year, we do not believe that this affected our results in any way, as the vast majority of symptoms and much of the pathology associated with abdominal ultrasounds are not influenced by seasonal factors. However, delay in performance and results could be increased in the month of August (peak holiday time in Spain and therefore with little activity).
In view of our results, we can conclude that recommendations and indications for abdominal ultrasound improve the quality of requests, as they provide more clinical information, a tentative diagnosis and, based on the results of our study, can also improve appropriateness.
FundingThis project received a grant from the Spanish Ministry of Science and Innovation, Instituto de Salud Carlos III, Spanish Agency for Health Technology Assessment (PI09/90159), and a Gonçal Calvo Grant 2009, from the Maresme Branch of the Academy of Medical Sciences of Catalonia and the Balearic Islands.
Conflict of interestsThe authors declare that they have no conflict of interests.
The authors would like to thank Dr Conxita Bru for her review and critical appraisal of the manuscript.
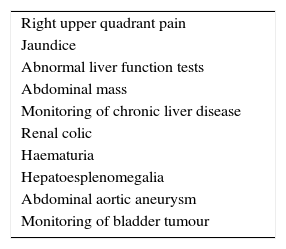
First question. What reasons do you consider appropriate for requesting an abdominal ultrasound?
| Right upper quadrant pain |
| Jaundice |
| Abnormal liver function tests |
| Abdominal mass |
| Monitoring of chronic liver disease |
| Renal colic |
| Haematuria |
| Hepatoesplenomegalia |
| Abdominal aortic aneurysm |
| Monitoring of bladder tumour |
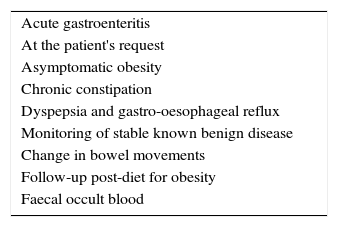
Second question. What reasons do you consider unjustified for requesting an abdominal ultrasound?
| Acute gastroenteritis |
| At the patient's request |
| Asymptomatic obesity |
| Chronic constipation |
| Dyspepsia and gastro-oesophageal reflux |
| Monitoring of stable known benign disease |
| Change in bowel movements |
| Follow-up post-diet for obesity |
| Faecal occult blood |
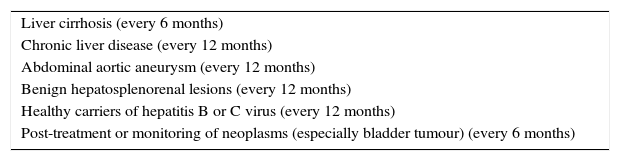
Third question. In which cases do you consider that follow-up abdominal ultrasound should be performed and how often?
| Liver cirrhosis (every 6 months) |
| Chronic liver disease (every 12 months) |
| Abdominal aortic aneurysm (every 12 months) |
| Benign hepatosplenorenal lesions (every 12 months) |
| Healthy carriers of hepatitis B or C virus (every 12 months) |
| Post-treatment or monitoring of neoplasms (especially bladder tumour) (every 6 months) |
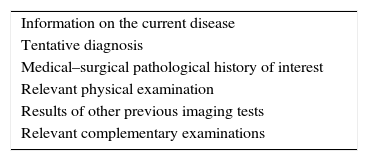
Fourth question. What is the minimal information that you consider should be provided on an abdominal ultrasound request?
| Information on the current disease |
| Tentative diagnosis |
| Medical–surgical pathological history of interest |
| Relevant physical examination |
| Results of other previous imaging tests |
| Relevant complementary examinations |
Please cite this article as: Caballería L, Pera G, Rodríguez L, Casas JD, Miranda D, Auladell MA, et al. Adecuación y calidad de las ecografías abdominales solicitadas por los profesionales de medicina. Gastroenterol Hepatol. 2016;39:516–525.