The pharmacist must work with the clinical team across the continuum of care to develop and therefore improve the patient's quality of life. In this study, we present the results from a continuous pharmaceutical care programme for patients admitted to an angiology and vascular surgery department.
Material and methodsA 5-month prospective study to evaluate the results of a pharmaceutical care programme in an angiology and vascular surgery department. The pharmacist went on the rounds with the clinical team from Monday to Friday and helped make decisions on treatment, and detect and resolve conciliation discrepancies upon admission and discharge, and drug-related problems during the hospital stay.
ResultsWe detected and resolved 273 conciliation discrepancies in 99 patients and 76 drug-related problems in 46 patients. Global acceptance of pharmacist interventions was 96%.
ConclusionsSeventy-four percent of patients presented conciliation discrepancies. Efficiency of pharmaceutical activity across the continuum of care is demonstrated by the high acceptance of the interventions.
La actuación conjunta del farmacéutico con el resto del equipo sanitario durante todo el proceso asistencial es necesaria para el desarrollo de la atención farmacéutica y así mejorar la calidad de vida del paciente. En este estudio se presentan los resultados de un modelo continuo de atención farmacéutica en pacientes ingresados en un servicio de Angiología y Cirugía Vascular (ACV).
Material y métodoEstudio prospectivo realizado durante 5 meses para evaluar el resultado de la actividad de un farmacéutico clínico en un servicio de ACV. El farmacéutico participa en el pase de visita de lunes a viernes y en la toma de decisiones con el equipo multidisciplinar, detectando y resolviendo errores de conciliación (EC) al ingreso y al alta y problemas relacionados con la medicación (PRM) durante la estancia hospitalaria.
ResultadosSe han detectado y resuelto 273 EC en 99 pacientes y 76 PRM en 46 pacientes. La aceptación global de las intervenciones farmacéuticas ha sido del 96%.
ConclusionesUn 74% de los pacientes han presentado EC. La eficiencia de la actividad farmacéutica a lo largo del proceso hospitalario queda recogida en el alto grado de aceptación de las intervenciones realizadas.
Adverse effects in hospitalised patients are a very significant health problem.1 Nearly half of them are preventable, and more than 15% are medication-related.2 Medication-related problems (MRPs) are defined as situations in which medication use causes or may cause the appearance of an unwanted results associated with that drug.3 Review of clinical histories shows that most medication errors occur in processes having to do with healthcare transfer and changing the patient's lead doctor.4 Medication reconciliation is defined as a complete, precise evaluation of the drugs taken by the patient before admission to the hospital and comparison of these drugs with those prescribed in the hospital. Any discrepancies, duplications or interactions that may be discovered must be discussed with the prescribing doctor and shared with the new care provider and the patient in order to guarantee that proper treatment is received.5 A discrepancy is considered to be a medication reconciliation error (MRE) when the prescribing doctor decides to modify treatment as soon as he/she is made aware of the discrepancy.5 This new process has made it necessary to reach a consensus with regard to terminology and classifications.6
MRE significance is reflected by initiatives and documents elaborated by such organisations as the Joint Commission on Accreditation of Health Care Organisations (JCAHO), the World Health Organisation (WHO) and the National Institute for Health and Clinical Excellence (NICE),7 all of which state that medication reconciliation is a key point for improving patient safety. Although pharmacists are recognised as the professionals best suited to compiling a complete drug treatment history, only NICE states that this process must be carried out by a pharmacist with clearly defined responsibilities that may vary depending on the clinical field.7
The aim of this study is to present the results of pharmacy activity integrated in an Angiology and Vascular Surgery (AVS) department, including MRPs detected and avoided during the hospital stay and reconciliation processes upon admission and discharge.
MethodA prospective, descriptive study was done to evaluate the result of a pharmacist's activities within the Angiology and Vascular Surgery department in a tertiary hospital over a 5-month time span (November 2008–March 2009).
From Monday to Friday, the pharmacist went on rounds with the doctors and nurse responsible for each of the patients. All patients hospitalised during the study period were included. We made use of four computer programs for record-keeping:
- •
Patient care information system (Sistema de Información de Atención al Paciente, eSIAP): obtaining chronic medications prescribed by the primary care doctor and detecting any possible risk factors not accounted for in the hospital medical history.
- •
Infowin (Grifols): creation of a timetable and list of prescriptions upon discharge
- •
Hospiwin (Baxter):
- ∘
Prescriwin application (Spain): monitoring of drug treatments during current and previous hospital stays, recording and keeping track of all procedures performed.
- ∘
Paciwin (Spain): follow-up on outpatients (dispensing services for outpatients from the hospital pharmacy department).
- ∘
- •
Hp Doctor (Hewlett-Packard, Spain): displays patient's hospital history (previous admissions, discharge reports, hospital tests and external consultations).
Completed interventions were classified as accepted, not accepted, and informative or dispensing. Interventions were considered accepted when they led to a treatment modification in less than 48h. Interventions were considered informative, or dispensing interventions were not intended to change the prescription.
Reconciliation discrepancies were recorded upon admission and discharge. They were classified according to the reconciliation terminology and classification consensus document.7 MRPs were recorded during the hospital stay according to an adapted version of the Tercer Consenso de Granada3 (Third Granada Consensus), which grouped them into 8 types: untreated indication, unnecessary drug, ineffective, underdosing, overdosing, adverse effect, side effects or interactions, medication error or incomplete prescription.
ResultsOf the 382 patients admitted between 1 November 2008 and 31 March 2009, 149 were subjected to interventions (77% male, mean age 62 years; range between 21 and 95 years). A total of 481 interventions were performed, meaning 1.26 interventions per patient out of the total of patients admitted and 3.23 interventions per patient in the intervention group.
The degree of acceptance was broken down as follows: 409 accepted (85%), 17 not accepted (3.5%), and 55 not applicable (11.5%). If we do not consider interventions that were not intended to modify the initial prescription, the acceptance rate rises to 96% (409/426).
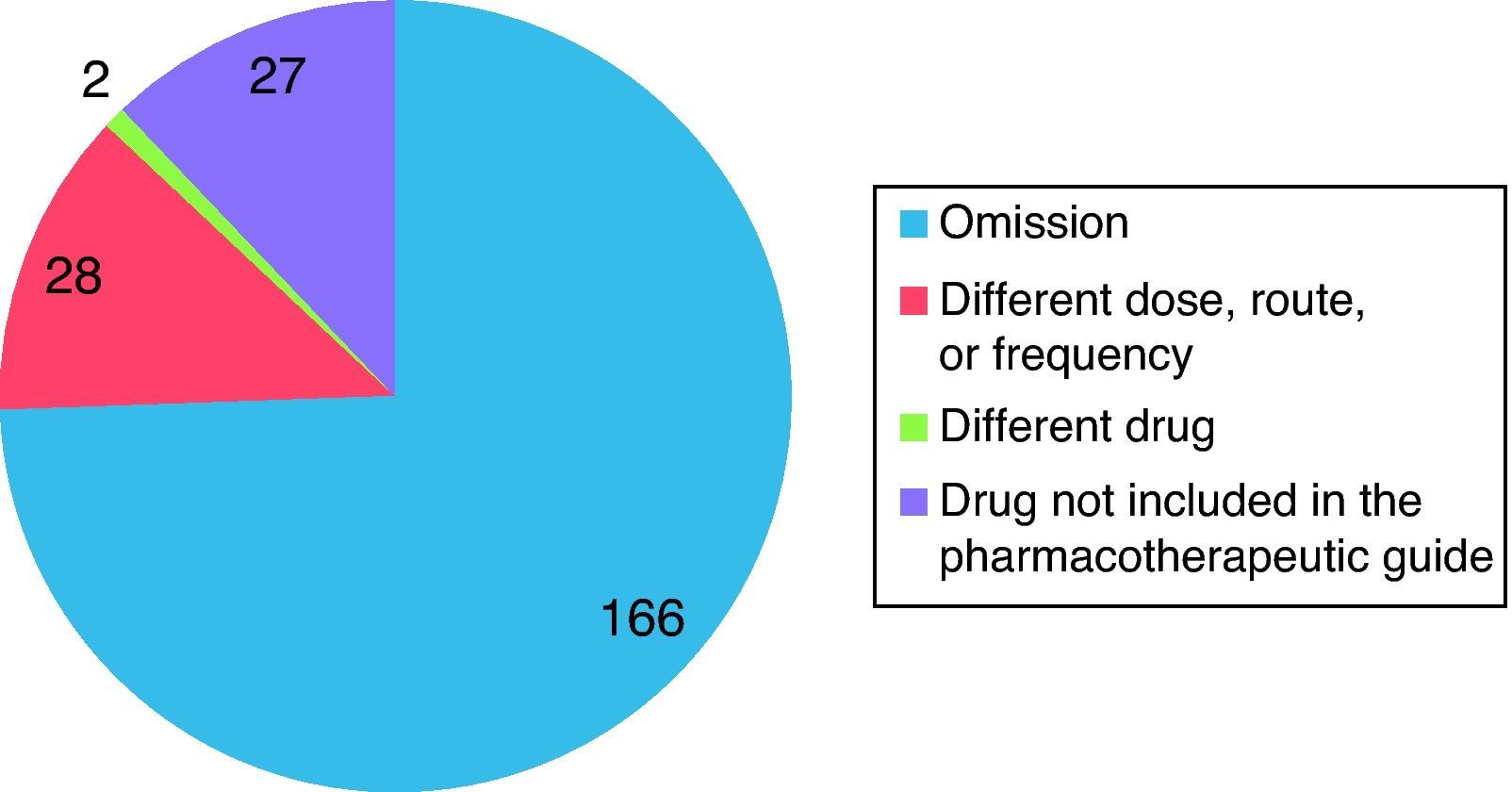
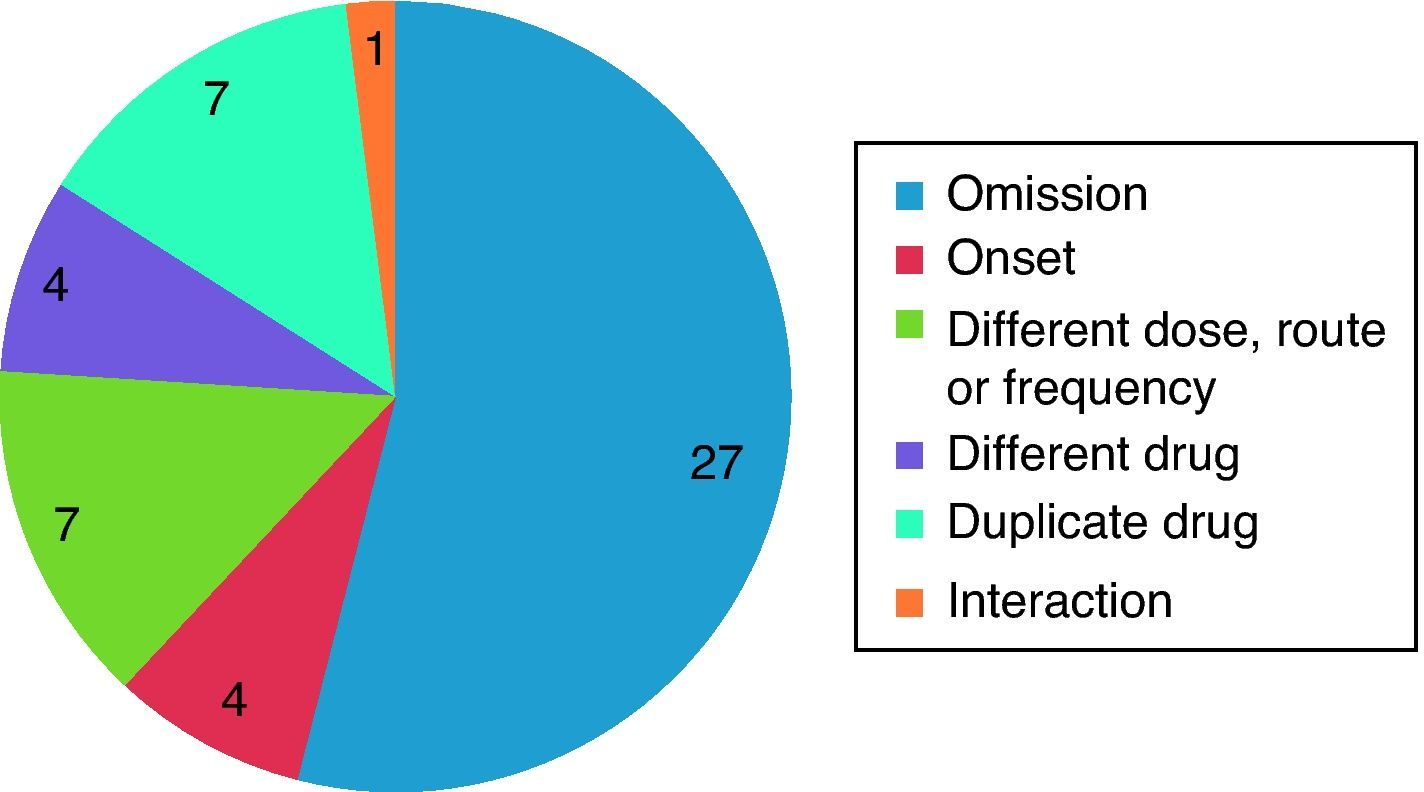
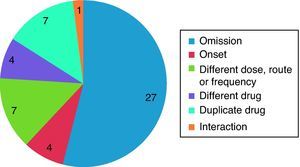
Interventions Associated With Medication ReconciliationOf the total of interventions completed, 403 were recorded during hospital admission or discharge. Some 71.2% of all interventions corresponded to discrepancies that required clarification; 11% corresponded to justified discrepancies, and the other interventions did not constitute discrepancies. Figs. 1 and 2 show the breakdown of MREs during hospital admission and discharge.
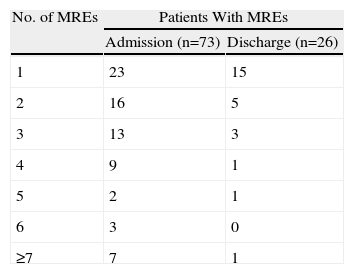
In the case of 123 patients, some sort of intervention was undertaken at the time of admission and/or discharge. A total of 273 MREs were detected in 87 patients, meaning 22.7% of the patients with reconciliation of MREs, 3.1 MREs per patient with at least 1 MRE, and a 95% acceptance rate.
Among the 237 unjustified discrepancies upon admission, we detected 223 MREs in the treatment applied to 73 patients. Based on these figures, 19.1% of patients had at least one MRE upon admission; 3 MREs per patient and a 94% acceptance rate. Upon discharge, we detected 50 discrepancies requiring clarification. All were MREs, and among patients with medication reconciliation, 26 had at least one MRE, meaning 6.8% of patients with MRE at discharge, 1.92 MREs per patient, and an acceptance rate of 100%. Table 1 shows the number of patients and MREs.
Interventions Linked to MRPsDuring their hospital stays, 76 MRPs were identified in 46 patients. We detected 30 MRPs having to do with an untreated indication, 24 overdoses, 8 adverse reactions, side effects or interactions between prescribed medications, 6 unnecessary drug, 4 underdoses, 2 unnecessary drugs and another 2 drug errors. The acceptance rate was 100%.
DiscussionSome MRE was present in 22.7% of the hospitalised patients (73 upon admission and 26 upon discharge). The degree of acceptance for discrepancies requiring clarification was 94% upon admission and 100% upon discharge. During their hospital stays, 76 MRPs were detected in 46 patients. All were resolved.
Montesinos Ortí et al.8 presented the results from a drug treatment monitoring programme in a surgical service where pharmacy interventions were performed at admission, during the stay and at discharge. For the 85 interventions having to do with effectiveness or safety, the acceptance rate was 97%, which was similar to that for the 76 MRPs found in our study. That study also took place in a surgical ward,9 where 63 MREs were detected upon admission in 84 patients older than 65 and with at least 1 chronic disease. This figure is lower in our study because drug reconciliation was provided for 100% of the hospitalised patients, compared with only 23.5% in that study. Its acceptance rate was close to 90%, similar to the 94% recorded at the time of admission. In the study completed by Delgado Sánchez et al.,10 52.7% of patients presented at least one MRE at the time of admission or discharge, with a statistically significant difference between the two times (admission, 66.8%; discharge, 39%). The number of detected MREs is lower due to using a selection of elderly and polymedicated patients, but they also found nearly double the rate of MREs upon admission.
The MRE distribution found here matches with that in the literature, with omission being the most frequent type of error.
To conclude, the acceptance rate for interventions is high regardless of when they are undertaken. We found a lower number of MREs than that of similar studies because rather than selecting patients during a specific period, we performed this activity continuously for all hospitalised patients.
Conflict of InterestThe authors have no conflicts of interest to declare.
Please cite this article as: Martínez López I, et al. Atención farmacéutica integral a los pacientes de un servicio de Cirugía Vascular. Farm Hosp. 2011;35:260–3.
Preliminary results from this study were presented in poster form at the 54th Congress for the Spanish Society of Hospital Pharmacy, held in Zaragoza in September of 2009.