The objective of the study was to assess home medication data collected at the emergency department in a tertiary hospital. It also aimed to identify whether any possible deficiencies in this collection were translated as reconciliation errors on admission, to analyse and classify these data and identify the pharmacological groups involved.
MethodsA prospective observational study was carried out which analysed the pharmacotherapeutic data collected at the emergency department. Patients who were admitted to the Pneumology and Internal Medicine wards at the Miguel Servet University Hospital in Zaragoza were included. A list of the home drugs taken before the hospital stay was compiled, assessing whether the quality deficiencies in data collected in the emergency department translated as reconciliation errors at admission. Unjustified discrepancies were considered and classified in line with the criteria of the consensus document on terminology, classification and assessment of the drug reconciliation programmes for 2009.
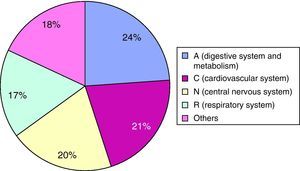
ResultsWe included 136 patients, finding reconciliation errors in 86.8%. The total number of reconciliation errors found was 519. The most frequent types were: omitting a drug, missing dose information, missing administration frequency information. Almost 40% of the reconciliation errors found in the Internal Medicine ward were not resolved, which was double to that of the Pneumology ward. Most discrepancies were found for the Digestive System and Metabolism group (24%).
ConclusionsThe percentage of patients that experienced reconciliation errors was high (86%), observing an important opportunity to improve at patient admission to the emergency department.
El objetivo del estudio fue valorar la calidad de la recogida de información de la medicación domiciliaria en el servicio de Urgencias de un hospital de tercer nivel, e identificar si las posibles deficiencias en esta recogida se tradujeron en errores de conciliación al ingreso, analizar estos y clasificarlos, así como identificar los grupos farmacológicos implicados.
MétodosSe realizó un estudio observacional prospectivo en el que se analizó la información farmacoterapéutica recogida en el servicio de Urgencias. Se incluyeron los pacientes que ingresaron en la Unidad de Neumología y de Medicina Interna del Hospital Universitario Miguel Servet de Zaragoza. Se elaboró un listado con la medicación domiciliaria del paciente antes del ingreso, y se valoró si las deficiencias de calidad en la información recogida en urgencias se tradujeron en errores de conciliación al ingreso. Se tuvieron en cuenta las discrepancias no justificadas y se clasificaron siguiendo los criterios del Documento de consenso sobre terminología, clasificación y evaluación de los programas de Conciliación de la Medicación 2009.
ResultadosSe incluyeron 136 pacientes, hallando errores de conciliación en el 86.8%. El número total de errores de conciliación encontrados fue 519. Siendo los subtipos más frecuentes: omisión de algún medicamento, falta de dosis y falta de frecuencia de administración. Cerca de un 40% de los errores de conciliación encontrados en el servicio de Medicina Interna no fueron resueltos, el doble de los encontrados en el servicio de Neumología. El grupo farmacológico en el que se encontraron más discrepancias fue el de aparato digestivo y metabolismo, con un 24%.
ConclusionesEl porcentaje de pacientes con errores de conciliación es elevado (86%), observándose una importante oportunidad de mejora al ingreso de los pacientes en el servicio de Urgencias.
The Institute for Healthcare Improvement (IHI) defines medication reconciliation as a formal process to compile a list of all the medications a patient is taking before admission, and comparing it with the doctor's admission, transfer and discharge orders.1 Discrepancies found should be reported to the prescriber, and where appropriate, should be corrected. The changes made should be appropriately documented and communicated to the following health provider and the patient.
In 2007, the Joint Commission on Accreditation of Healthcare Organizations (JCAHO) acknowledged that reconciliation errors compromise the safety of drug use and recommended hospitals to develop a system for obtaining patients’ complete pharmacotherapeutic records, to ensure they receive the necessary drugs for the new situation.2
In the Documento de consenso sobre terminología y clasificación en Conciliación de la Medicación3 (Consensus document on terminology, classification and assessment of the drug reconciliation programmes) endorsed by the Spanish Society of Hospital Pharmacy, discrepancies are defined as any difference between the chronic medication that the patient was taking before admission and the medication prescribed in the hospital. One discrepancy does not necessarily mean an error. In fact, most discrepancies are due to adapting chronic medication to the patient's newly diagnosed condition, or because the examinations and/or interventions performed could interfere with their usual medication. However, there are often differences that do constitute errors in the healthcare process, which could affect the patient's pharmacotherapeutic results.
Performing tasks that promote an adequate reconciliation has proven to be a powerful strategy for reducing medication errors when a patient's healthcare level changes. Over a period of 7months, Whittington and Cohen4 found that a series of interventions for a 7-month period, including medication reconciliation, would reduce medication errors by 70% and the frequency of adverse effects by 15%. Within this framework, the supplementary pharmacist programme was started in the region of Aragón in 2007. It involved two Hospital Pharmacy Specialists who develop medication reconciliation activities upon admission and discharge and various pharmacy-care tasks for the patient.
The aim of the study was to assess home medication data collected at the emergency department in a tertiary hospital. It also aimed to identify whether any possible deficiencies in this collection were translated as reconciliation errors on admission, to analyse these data and classify them, and to identify the pharmacological groups involved.
MethodsA prospective observational study was carried out, which analysed the pharmacotherapeutic data collected upon admission at the emergency department.
Patients who were admitted from 15 April 2009 until 14 May 2009 to the Pneumology and Internal Medicine wards at the Hospital Universitario Miguel Servet in Zaragoza, were included. The number of patients admitted to the hospital was obtained from hospital admission program, considering that those admitted on a bank holiday or at the weekend were recorded the following day. Patients in a life-threatening situation, those who had not been admitted through the emergency department, planned admissions, or those transferred from outside units, were not included. Nor did we include those patients who had no prescription billing data available from the pharmacy offices, given that the health insurance card number was not available in the hospital admission program.
The information sources used to elaborate the usual pharmacotherapeutic records were: (1) electronic emergency department reports created using the PCH-Urgencias program, available through the hospital's Intranet; (2) the patient's clinical records, from the Internal Medicine or Pneumology wards, collected in paper format; (3) information from prescriptions invoiced by pharmacy offices to the Servicio Aragonés de Salud (Aragon health service) during the past 6months, which are obtained using the Farmasalud® database, using the patient's health insurance card number; (4) the outpatient unit from the Pharmacy department from where the information about medication withdrawn in the last 6months, which together with the treatment of the admitted patients, was collected from the pharmacy department management program (Savac Integración®); (5) discharge reports for patients admitted were obtained using the HP-Doctor® program.
Given that the study aims to assess home medication collected, we excluded any acute condition treatment (antibiotics, analgesics, etc.), drugs administered on one-off occasions (less than one dose every 48h), dietary supplements, medicinal plants and parapharmacy.
With this information, the pharmacist compiled a list of the patient's home drugs prior to admission. The patient interview was not considered, as it could not be conducted adequately for all patients. This information was compared to that collected in the emergency department.
Only the discrepancies considered as unjustified (reconciliation error) were collected, and categorised in accordance with the criteria from the Documento de consenso sobre terminología, clasificación y evaluación de los programas de Conciliación de la Medicación 2009, endorsed by the Spanish Society of Hospital Pharmacy.
We collected information on demographic variables (sex and age), pharmacotherapeutic variables (number of home drugs, number of drugs in the emergency department records), and type and number of unjustified discrepancies.
We analysed the drugs affected by unjustified discrepancies, observing the therapeutic groups and subgroups. We quantified/identified the drugs that had unjustified discrepancies which should have been reconciled during the first 4h, in accordance with the recommendations from the Massachusetts Hospital Association's Medication Error Prevention project.5
We examined the differences between the Pneumology and Internal Medicine wards and determined the prescription's quality indicators. We used the following as prescription quality indicators: the number of patients with reconciliation errors (defined as the coefficient between the number of patients with ≥1 reconciliation errors and the number of reconciled patients), drugs with reconciliation errors (defined as the coefficient between the number of reconciliation errors and the number of reconciled drugs) and the reconciliation errors per patient (defined as the coefficient between the number of reconciliation errors and the number of patients with ≥1 reconciliation errors.) To measure the quality of the pharmacist's activity, we assessed which discrepancies were resolved within 48h without the pharmacist's participation. Therefore, we recorded the resolved reconciliation errors between the first drug order available in the Pharmacy Department and the pharmacotherapeutic data from the emergency department, within the first 48h.
Statistical AnalysisWe performed a descriptive statistical analysis of the variables studied, calculating the central tendency and dispersion for quantitative variables and percentages for qualitative variables. The chi-square test was used to show dependency or independency between the qualitative variables. When the expected values were less than 5, we used Fisher's exact test for correction. We used Student's t test or the Mann–Whitney U test (according to the Kolmogorov–Smirnov test) to compare means for quantitative variables.
We performed a logistic regression analysis, applying the entry method, using the Hosmer–Lemeshow test to analyse the model's goodness to fit. A dependent variable was defined as having or not having unjustified discrepancies, and independent variables were sex, ward, age and number of drugs, considering the last two to be continuous variables. A negative binomial regression model was performed defining the number of unjustified discrepancies as a dependent variable and sex, ward, age and number of drugs as independent variables.
We assumed that the differences found had statistical significance when P<.05.
ResultsA total of 170 patients were identified during the study period. Of them, 18 Internal Medicine and 16 Pneumology patients were excluded because they did not meet the inclusion criteria, resulting in 136 patients in the study.
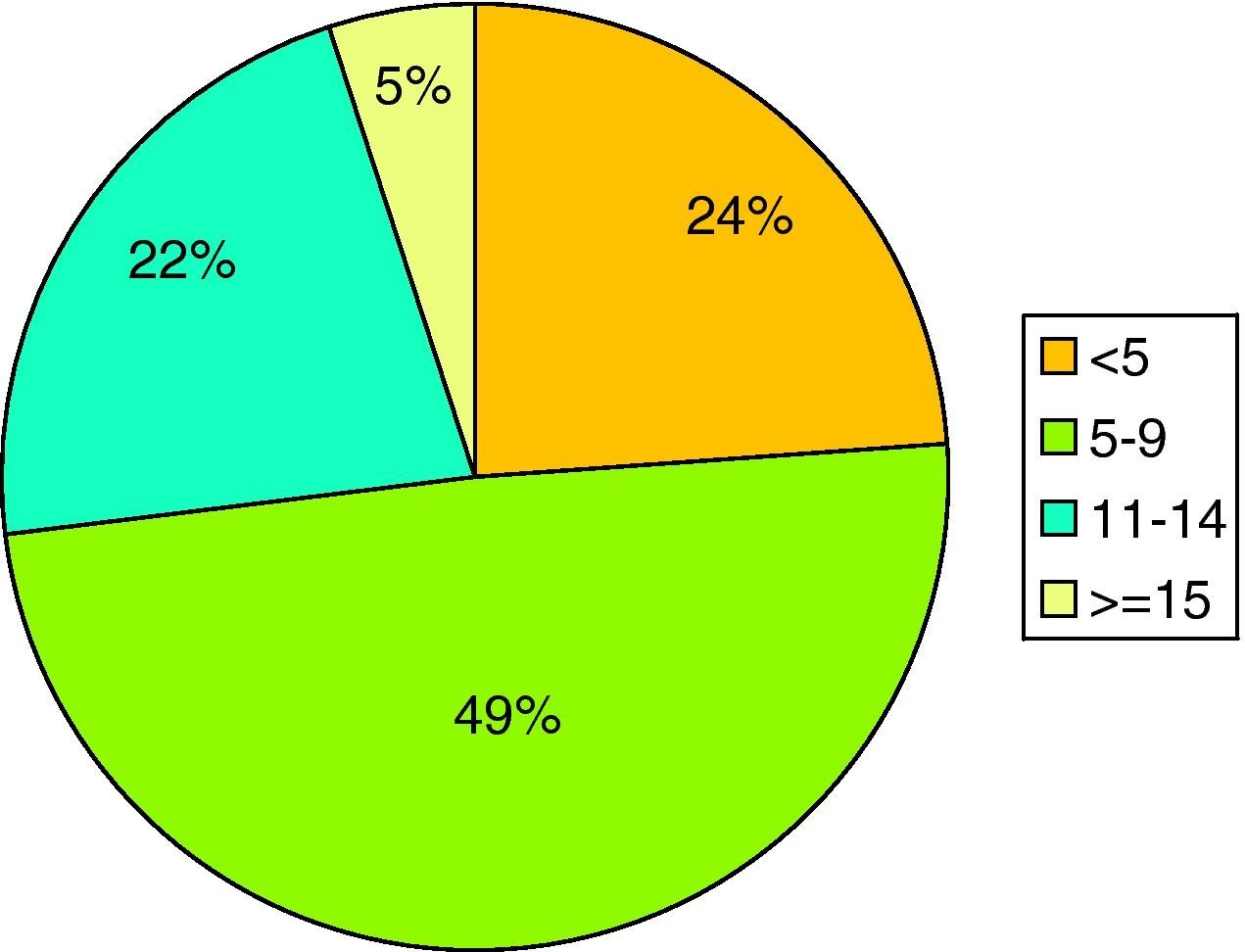
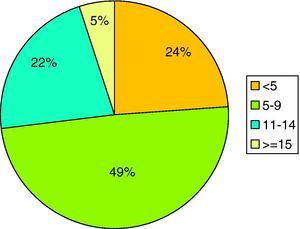
Of the total, 64.7% (n=88) were men and 35.3% (n=48) were women. The average age was 75.9±12.5years. About 45.7% (n=62) were admitted to Internal Medicine and 54.4% (n=74) to Pneumology. Patients presented with an average of 7.4±4.0 drugs in their home treatment, with a maximum of 20 and a minimum of 0. Fig. 1 shows that the usual pharmacotherapy included 5 or more drugs in 76% of patients. The average number of drugs collected in the emergency department was 6.7±3.9, with a maximum number of 20 and a minimum of 0.
Of the 136 subjects studied, 118 (86.8%) showed reconciliation errors upon admission to the relevant wards. No differences were found due to sex for the reconciliation errors (P=.474). About 83.9% (n=52) of all the patients admitted to the Internal Medicine ward presented with reconciliation errors, and 89.2% (n=66) of those admitted to Pneumology (P=.362). With regard to patients with unjustified discrepancies, the Internal Medicine ward patients were older (77years) than those in the Pneumology ward (74years).
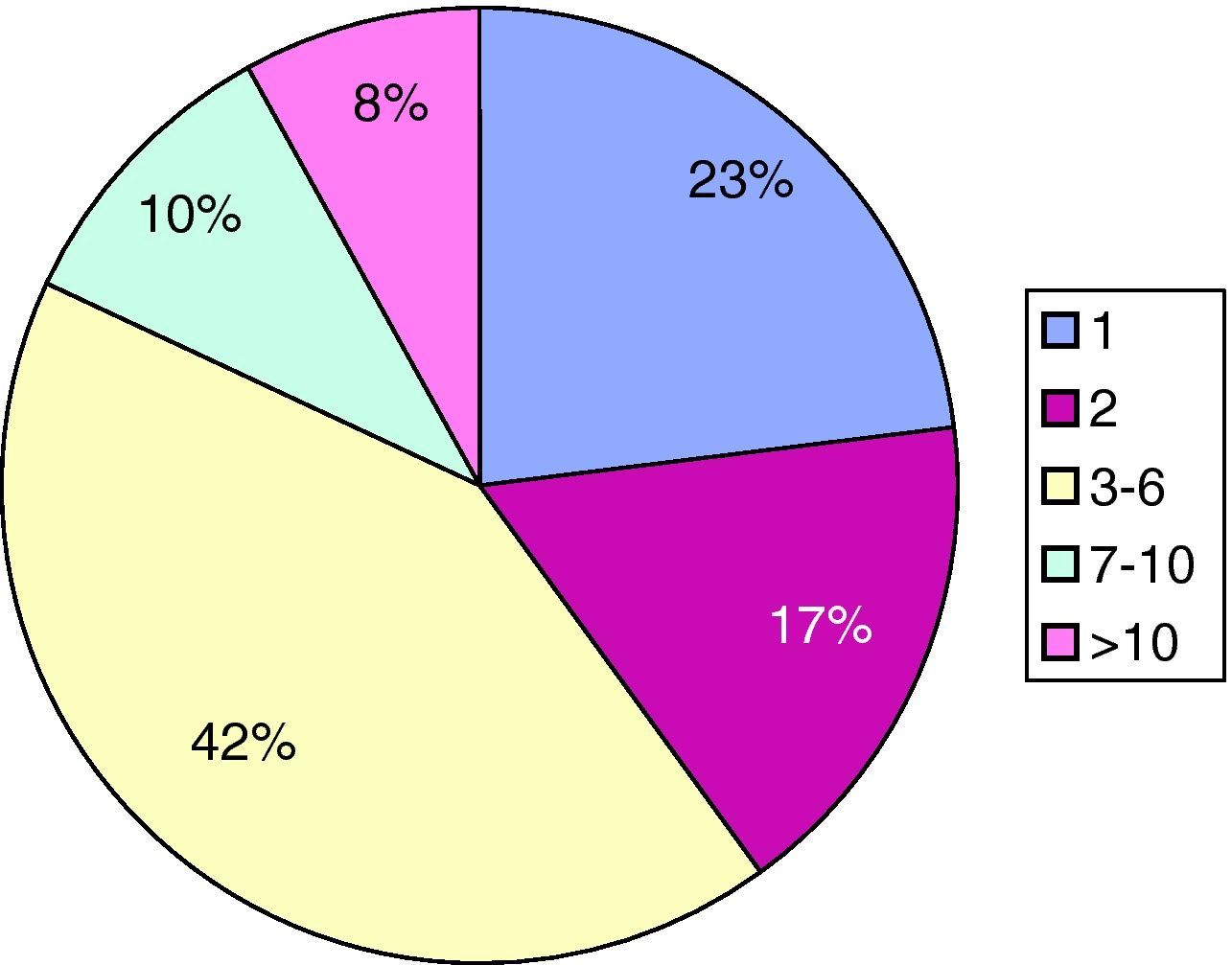
Patients with unjustified discrepancies usually had 5 or more drugs (92.3%), compared with 68.7% of patients without discrepancies (P=.004). For 118 patients with at least one reconciliation error, the average was 4.4±3.7 reconciliation errors, and 41.5% (n=49) of patients had between 3 and 6 reconciliation errors (Fig. 2). Reconciliation errors of 4.38 were found per patient.
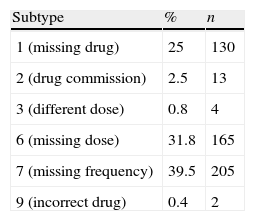
In total, 519 unjustified discrepancies were found. Among these, the most common subtypes were: subtype 1 (missing drug), subtype 6 (missing dose) and subtype 7 (missing frequency), as shown in Table 1. No discrepancy was found in the subtype 4 (different frequency), 5 (different route) and 8 (missing route).
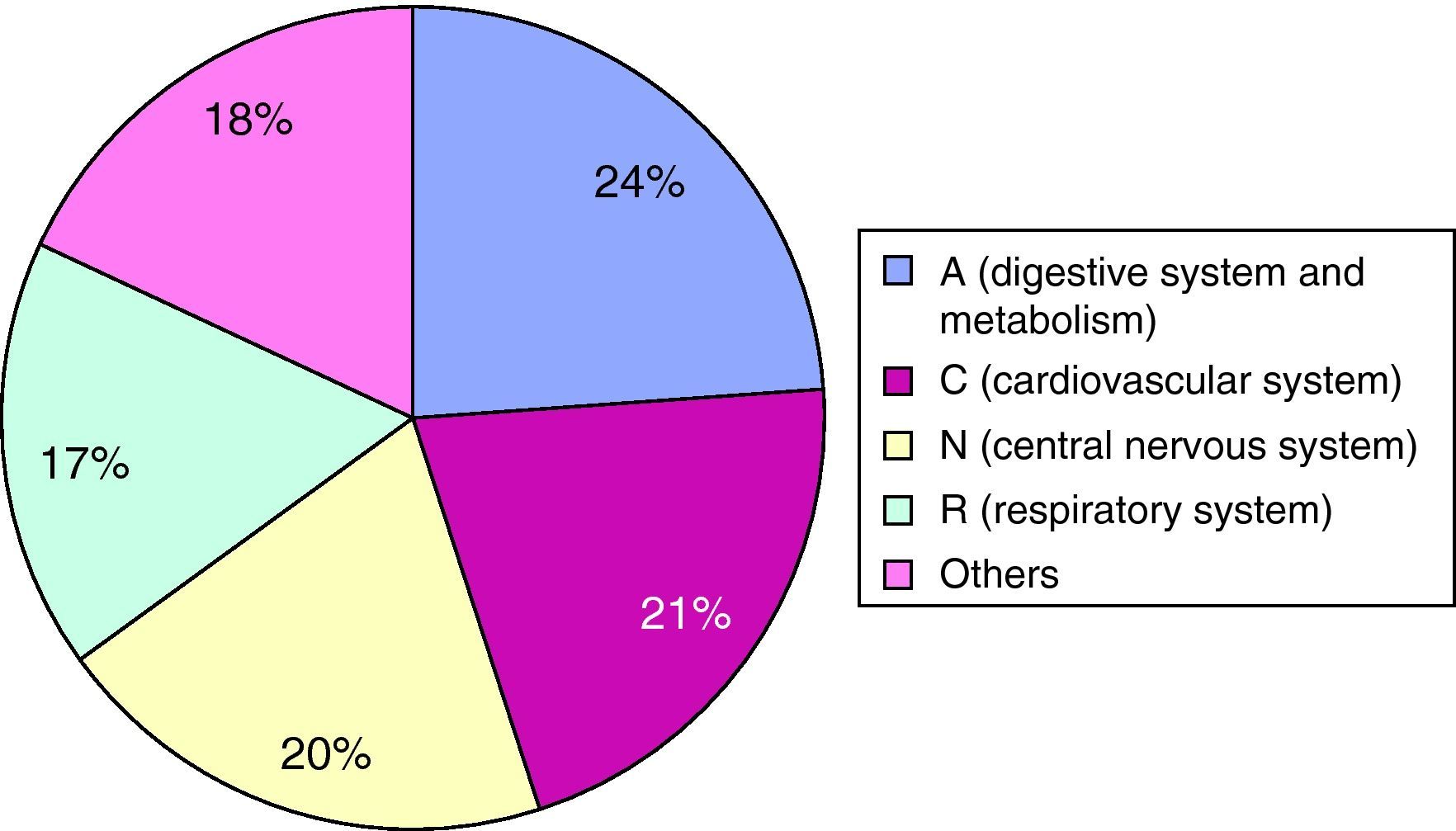
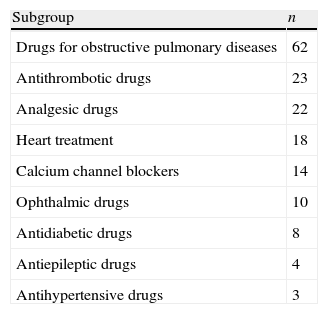
The drugs involved in these discrepancies would be included more frequently among the pharmacological groups that are included in Fig. 3. The drug subgroups that had the most discrepancies were drugs for acid related disorders (93 cases), drugs for obstructive airway disorders (62), psycholeptic drugs (35), psychoanaleptic drugs (33) and diuretic drugs (33). The drugs that were not reconciled in the first 4h are shown in Table 2.
Discrepancies Detected in the Drug Subgroups That Must Be Reconciled During the First 4h.
| Subgroup | n |
| Drugs for obstructive pulmonary diseases | 62 |
| Antithrombotic drugs | 23 |
| Analgesic drugs | 22 |
| Heart treatment | 18 |
| Calcium channel blockers | 14 |
| Ophthalmic drugs | 10 |
| Antidiabetic drugs | 8 |
| Antiepileptic drugs | 4 |
| Antihypertensive drugs | 3 |
n: number of cases.
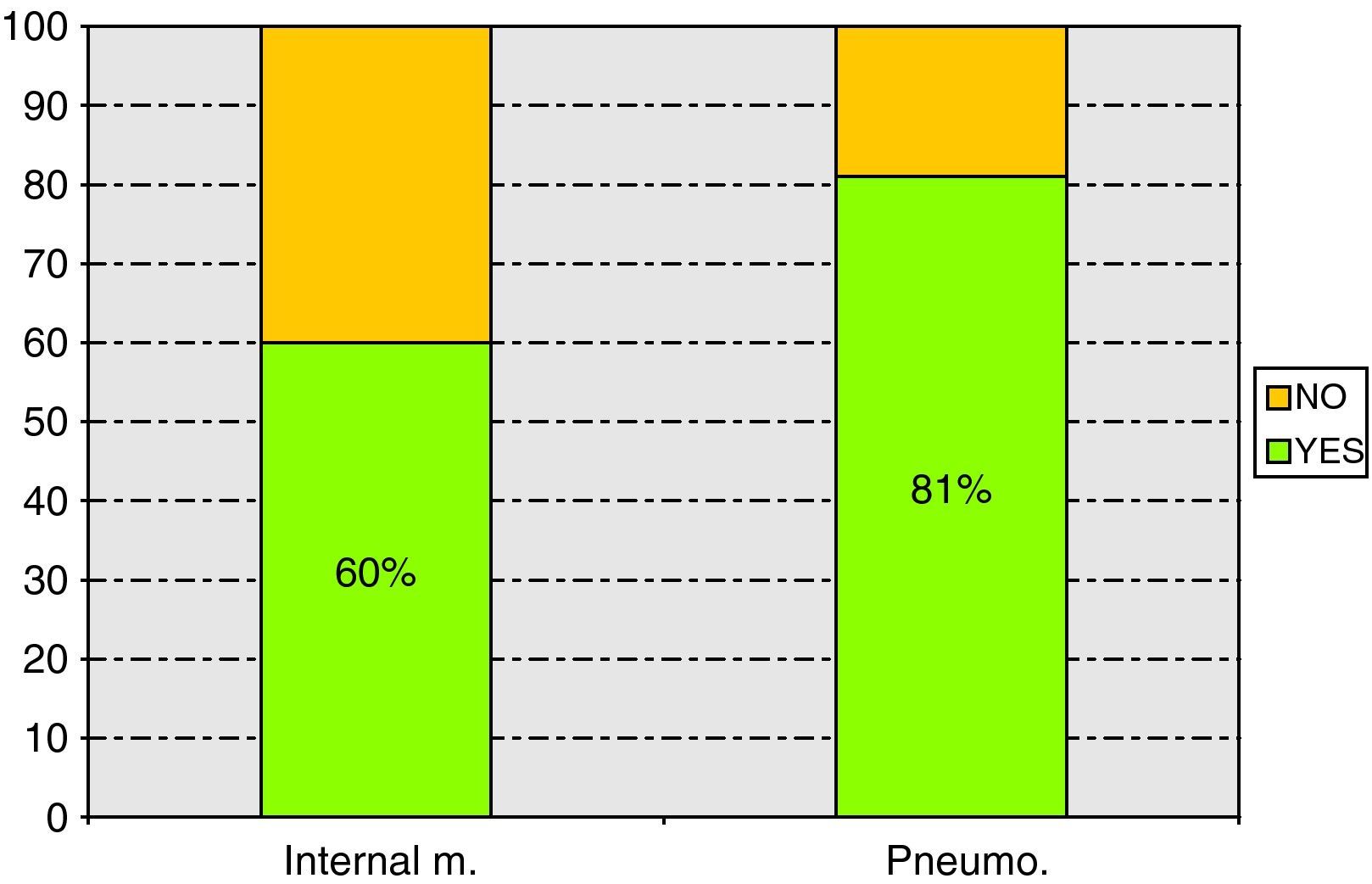
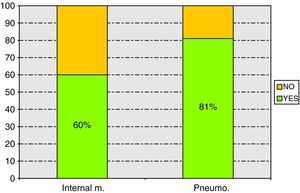
Of the 519 discrepancies found, 27.9% were not resolved during the first 48h following admission. A statistical relationship was found between the discrepancies that were resolved and the ward involved (P<.001) as is shown in Fig. 4.
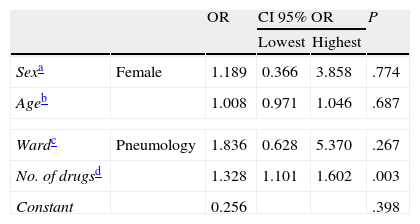
We created a logistic regression model to examine the possible variables associated with the presence of unjustified discrepancies. Table 3 shows the results obtained. Only the number of drugs taken by the patient was found to be a significant variable. The probability that a discrepancy would arise increased by 32.8% when more drugs were taken. Although it was not statistically significant, it was more likely that women, older patients and pneumology patients had discrepancies.
Variables Associated to a Discrepancy. Logistic Regression.
| OR | CI 95% OR | P | |||
| Lowest | Highest | ||||
| Sexa | Female | 1.189 | 0.366 | 3.858 | .774 |
| Ageb | 1.008 | 0.971 | 1.046 | .687 | |
| Wardc | Pneumology | 1.836 | 0.628 | 5.370 | .267 |
| No. of drugsd | 1.328 | 1.101 | 1.602 | .003 | |
| Constant | 0.256 | .398 | |||
CI, 95% confidence interval; OR, odds ratio; P, statistical significance.
We chose the patients who had discrepancies (n=118) and created a negative binomial regression model so as to examine the possible patient variables associated with the number of discrepancies. We chose this model as there was overdispersion for the variable ‘number of discrepancies’. The variance exceeded the average and the Poisson regression was therefore not advisable. Only the association between the actual number of drugs that the patient takes and the number of discrepancies was found to be significant. That is, the number of discrepancies increases as the patient takes more drugs. We could assert with a probability of 95% that for every extra drug, the number of discrepancies increases between 1.003 and 1.019. The number of discrepancies increases with age and is greater for women and Internal Medicine patients, although these relationships were not significant.
DiscussionMedication errors are one of the main causes of morbidity for hospitalised patients. Reviewing the clinical records showed that half of the medication errors are produced in processes related to changes in the healthcare level and when the healthcare professional responsible for the patient is changed.6 Discrepancies produced between the drugs that the patient was taking before admission and those prescribed in the hospital has been demonstrated in various studies.7,8 The heavy workload healthcare professionals, the increased number of admissions and staff rotation means that less time is dedicated to looking at the patients’ records. On many occasions, staff are not able to fill out pharmacotherapeutic records in detail, causing discrepancies to be produced in the information registered, which although does not cause serious harm in most cases, but may cause moderate or severe harm to 39% of the patients.7
Of the 136 subjects studied, 86.6% (118) presented with a type of reconciliation error, which is similar to various national,9 and international10 studies, as is shown in a 2005 meta-analysis11 where it is concluded that more than 50% of pharmacotherapeutic records presented some type of reconciliation error. These data also match a recent multicentre study performed in four hospitals on the Balearic Islands, which reported that 52.7% of the patients had reconciliation errors. This data varies depending on each hospital's environment, given that there was a range between 43.9% and 66.9%, depending on the study centre.12
The patients included were mainly men, which is different from what we found in other studies.9,13 This could be because different wards were examined in the studies. The average age was 75.9years, as both of the wards that were examined care for elderly patients.
In our study, 98.5% of the patients took drugs for chronic conditions upon admission, which is different to the Societat Catalana de Farmàcia Clínica study,9 which reported that only 72.8% of patients took chronic medication. This could be because the Catalonian study only included surgical patients, with an average age of 61.9, 14years less than our patients, which reduced the probability that patients would take chronic home medication.
Of the 118 patients with discrepancies, the average was 4.38, and more than 70% had 3 or more discrepancies. This average was higher than in other wards such as that in the study of Moriel et al.13 and Gutiérrez Pauls et al.,14 which detected an average of 2 discrepancies per patient. This could be due to differences between the studies, given that our study examines medical departments and not surgical departments.
The most common discrepancies were missing drug, missing dose and missing frequency. These data do not match with the other studies,9,12,13,15 given that only 25% corresponded to missing drugs, compared with 53.5% in the Moriel et al.13 study, 58% in the multicentre study of the Balearic Islands, and 56% for omission in a 2007 American study.
In our study we differentiate between missing dose (31.8%) and missing frequency (39.5%); however, in the Moriel et al.13 study, they are grouped together as incomplete prescription, obtaining 18.3% of discrepancies. We must highlight that we did not find any discrepancies for missing route, incorrect frequency or incorrect route, as is reflected in other studies9,13 which could lead to significant medication errors depending on the drug involved.
Most of the discrepancies were in the following pharmacological subgroups: digestive system and metabolism, cardiovascular system, nervous system and respiratory system. These data were similar to that of other studies9,13 except for the cardiovascular group and the respiratory group, with a greater frequency in our study than in the others. We must consider, however, that it is common for patients from Internal Medicine and Pneumology to take home medication for respiratory and cardiovascular systems, given the most prevalent illnesses that are cared for in these wards and the average age of the patients in the study. This is similar to the Balearic Island study (76.27).
With regards to the relevance of the discrepancies found, as an indirect measure, we counted the discrepancies that should have been reconciled during the first 4h following admission, in accordance with the recommendations.5 As such, we found drugs for obstructive airway disorders (n=62), antithrombotic drugs (n=23), heart treatment drugs (n=18) and antidiabetic drugs (n=8). This could be due to the fact that the emergency department handles a heavy workload,16 the delay in admission to the hospitalisation units, and lack of pharmacists in the emergency department, who could have participated in collecting data for the pharmacotherapeutic records and in treatment reconciliation.17,18
When comparing the wards, we must point out that the differences found between age and the drugs involved in the discrepancies is possibly because Internal Medicine patients’ average age was greater than those from the Pneumology ward, and therefore they had a different drug prescription profile. We did not observe any differences between the wards concerning the percentage of patients with discrepancies.
On the other hand, patients with more drugs had more discrepancies for missing items, probably because when the number of home drugs increased, the probability that the patient would forget to transmit this information also increased, especially for elderly patients, which was the majority of patients included in the study.16
We were able to check this aspect using the multivariate analysis, given that the number of drugs had an impact on the number of discrepancies. Although this association was not significant, we also observed a relationship between the number of discrepancies and increased age, women and the Internal Medicine ward.
Almost 40% of the reconciliation errors found in the Internal Medicine ward were not resolved, which was double to that of the Pneumology ward. This could be related to the tasks that a supplementary pharmacist performed during the study period in the Pneumology ward, which were not performed in the Internal Medicine one. This result was similar to the study conducted by NICE,18 which found that when the pharmacist participated in medication, reconciliation errors reduced from 44% to 19%. However, this meant that 20% of the reconciliation errors were still unresolved, although it is possible that some of them would have been resolved after the 48h following the patient's admission or discharge. It is important to implement measures so that they can be resolved as quickly as possible when patients are admitted to the emergency department.
The percentage of patients with reconciliation errors is high (86%), which implies an important improvement opportunity in collecting pharmacotherapeutic information when patients are admitted to the emergency department. The lowest number of discrepancies was found in the department where a pharmacist was present, which confirms that a pharmacist's presence is relevant when writing pharmacotherapeutic records, and in improving the quality of this process.
The main study limitation was that there was no clinical interview with the patient, which would have been extremely interesting as it would have provided us with more exhaustive information about assessing the adherence to prescribed treatment or possible adverse effects.
It would be interesting if future studies were to assess the possible impact that reconciliation errors could have on the patient.
Despite the limitations, the study reveals that there is a serious problem concerning the lack of detail in collecting information on the patient's previous medication at emergency departments. Given the high percentage of patients with reconciliation errors (86%), the opportunity for improvement is important.
Ethical ConsiderationsThis project received approval from the Comité Ético de Aragón (Ethics Committee of Aragón) on 17 June 2009.
Conflict of InterestThe authors affirm that they have no conflicts of interest.
Please cite this article as: Soler-Giner E, et al. Calidad de la recogida de la medicación domiciliaria en urgencias: discrepancias en la conciliación. Farm Hosp. 2011;35(4):165–171.
Preliminary results accepted as a presentation in the 27 Congreso de la Sociedad Española de Calidad Asistencial, Seville, 2009 (Record No C-791).