To detect, quantify, and compare the medication error produced with manual versus electronically assisted prescription systems.
MethodsA descriptive, observational, prospective study in two traumatology hospitalisation units; one with manual prescriptions and the other with electronically assisted prescriptions. Prescription errors were determined.
ResultsWe analysed 1536 lines of treatment (393 treatment forms) from 164 patients. With manual prescriptions, we detected errors in 19.54% of cases, compared to 9.4% in electronically assisted prescriptions. Omission errors were significantly lower with electronically assisted prescriptions, especially with drugs that act upon the central nervous system.
ConclusionsPrescription error has decreased by 53% since computerising the prescription process. This is particularly useful for omission errors, as prescription is more complete. The decrease in error regarding drugs that act on the central nervous system stands out.
Detectar, cuantificar y comparar los errores de medicación producidos con un sistema de prescripción manual frente a un sistema de prescripción electrónica asistida en la fase de prescripción.
MétodoEstudio prospectivo, descriptivo y observacional en dos unidades de hospitalización de traumatología de un hospital general; una con prescripción manual y otra con prescripción electrónica asistida. Se han valorado los errores de prescripción.
ResultadosSe analizaron 1.536 líneas de tratamiento (393 hojas de tratamiento) de 164 pacientes. Con la prescripción manual se detectaron un 19,54% de errores frente al 9,14% ocasionados con la prescripción electrónica asistida. Los errores de omisión fueron significativamente menores con la prescripción electrónica asistida, principalmente los producidos con fármacos pertenecientes al grupo del sistema nervioso central.
ConclusionesAl informatizar la prescripción han descendido un 53% los errores de prescripción. Los errores que más se corrigen son los de omisión, al hacerse la prescripción de manera más completa; y fue destacable la disminución de errores en los fármacos del grupo del sistema nervioso central.
New technologies in hospitals, and particularly integrated and shared information systems, make it possible to significantly reduce medical errors and provide a high level of information about processes, costs and results. Electronically assisted prescription (EAP) and support systems to make decisions on the use of drugs have been proposed by many organisations and societies as useful tools and safety strategies.1 The 2020 Strategy Plan of the Sociedad Española de Farmacia Hospitalaria (Spanish Society of Hospital Pharmacists, SEFH) states that 80% of hospitals must have electronic prescription by 2020. Most national4,5 and international2,3 studies report a decrease in medication errors (ME) where EAP is implemented to improve patient safety. Specifically, this tool reduces prescription errors,6 and these are the most common ME, with over 50% of errors, according to most published studies.7,8 The incidence of medication errors is estimated between 0.3% and 9.9% of prescriptions in admitted patients.9–12
The aim of the study was to detect, quantify and compare the ME produced in a manual prescription (MP) system with an EAP system in the prescription phase.
MethodsThis was a prospective, descriptive, observational study in a tertiary hospital. Medical orders were selected from a period of 45 days for all patients admitted with drug therapy in two trauma units with 28 beds each: one with MP and the other with a 5-month history of EAP implementation.
The MP in our hospital is done with a carbonless copy sheet or physician's order form (MO), with one of the copies sent to the Pharmacy Unit, where the pharmacist copies and validates the MO with Hospiwin® Prescriwin® software. For EAP, the doctor completes the prescription with this programme, which is then validated by a pharmacist. This software provides real-time support with, for example, the most common dose, maximum and minimum dosages, therapeutic duplication alerts, drug interactions and patient's allergies. It also includes the medicines database of the hospital pharmacotherapeutic guidelines.
Classification of the prescribing errors was performed using the Updated classification for medication errors by the Ruiz-Jarabo 2000 Group from May 2008,13 as follows:
- 1.
Patient and MO misidentification: this type of error was defined for the total number of medical orders reviewed.
- 2.
Treatment line prescription error: where a treatment line is defined as a new prescription for a medicine or modification to an already prescribed drug in a MO. These errors were classified as follows:
- -
Wrong drug: classified as contraindicated due to the patient having a history of allergy, renal or liver failure, or due to patient age, interaction, or because of an unnecessary, duplicated or illegible drug.
- -
Incorrect dosage: dosage is missing or illegible, or for being higher or lower according to the technical data sheet, considering the renal and hepatic function and/or patient's age.
- -
Wrong frequency of administration.
- -
Wrong pharmaceutical form.
- -
Wrong route of administration.
- -
The technical data sheets for all drugs prescribed were reviewed to identify the errors listed above, as well as the medical history of each patient, documenting the age, sex, drug allergies, comorbidity, personal background and renal clearance during admission. Errors were distributed according to the ATC therapeutic groups, differentiating between medication in the Area 4 pharmaceutical guide (MEDG) and those not included (MEDNG). The error in the treatment line was defined considering the total number of lines reviewed.
To avoid any bias, neither the doctors nor the nurses knew of the existence of the study. The transcription and daily validation of the medical orders were carried out by a different pharmacist from the one who did the review. Two more pharmacists considered any questions or discrepancies in the interpretation of results.
The data were analysed using Evaluación software, version 1.0.1, developed by the hospital clinic biostatistics unit (http://www.hrc.es/investigacion/bioest/otras_calculadoras.html) which calculated the error rate, the relative risk reduction (RRR) and the absolute risk reduction (ARR). To find out if the number of treatment lines for a MO or the sex and age of the patient had an impact on the number of errors, a binary logistic regression model was applied with repeated measurements (GEE) using Stata 10.0 software.
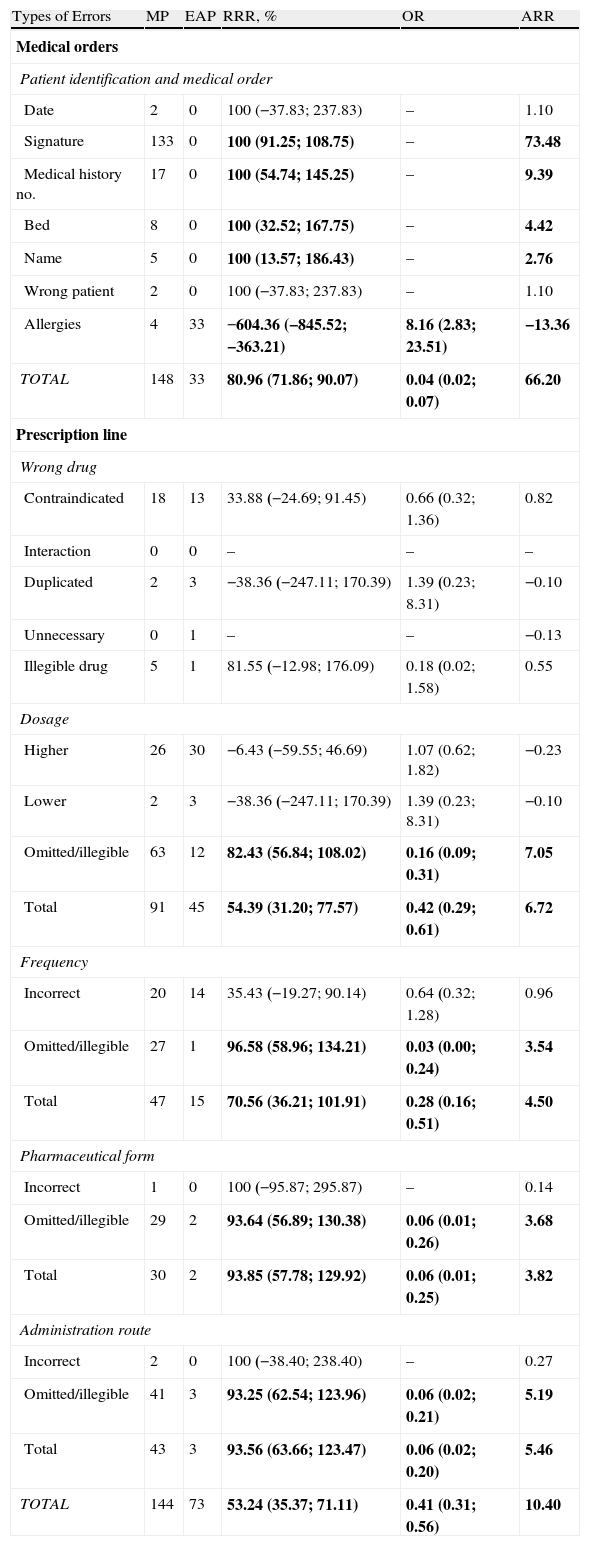
ResultsThere were 393 medical orders analysed (212 EAP and 181 MP) from a total of 164 patients. Only 33 (18.2%) of the MP orders were successfully completed compared to 179 (84.4%) of EAP orders. These orders were distributed over 1536 treatment lines (799 EAP and 737 MP), with 19.54% of errors being detected in the MP compared to 9.14% in the EAP, resulting in a statistically significant RRR of 53.24% after computerisation of the prescription. The patient identification, MO and treatment line errors are shown in Table 1.
Types of Errors Relating to Patient Identification, Medical Orders and Treatment Lines.
| Types of Errors | MP | EAP | RRR, % | OR | ARR |
| Medical orders | |||||
| Patient identification and medical order | |||||
| Date | 2 | 0 | 100 (−37.83; 237.83) | – | 1.10 |
| Signature | 133 | 0 | 100 (91.25; 108.75) | – | 73.48 |
| Medical history no. | 17 | 0 | 100 (54.74; 145.25) | – | 9.39 |
| Bed | 8 | 0 | 100 (32.52; 167.75) | – | 4.42 |
| Name | 5 | 0 | 100 (13.57; 186.43) | – | 2.76 |
| Wrong patient | 2 | 0 | 100 (−37.83; 237.83) | – | 1.10 |
| Allergies | 4 | 33 | −604.36 (−845.52; −363.21) | 8.16 (2.83; 23.51) | −13.36 |
| TOTAL | 148 | 33 | 80.96 (71.86; 90.07) | 0.04 (0.02; 0.07) | 66.20 |
| Prescription line | |||||
| Wrong drug | |||||
| Contraindicated | 18 | 13 | 33.88 (−24.69; 91.45) | 0.66 (0.32; 1.36) | 0.82 |
| Interaction | 0 | 0 | – | – | – |
| Duplicated | 2 | 3 | −38.36 (−247.11; 170.39) | 1.39 (0.23; 8.31) | −0.10 |
| Unnecessary | 0 | 1 | – | – | −0.13 |
| Illegible drug | 5 | 1 | 81.55 (−12.98; 176.09) | 0.18 (0.02; 1.58) | 0.55 |
| Dosage | |||||
| Higher | 26 | 30 | −6.43 (−59.55; 46.69) | 1.07 (0.62; 1.82) | −0.23 |
| Lower | 2 | 3 | −38.36 (−247.11; 170.39) | 1.39 (0.23; 8.31) | −0.10 |
| Omitted/illegible | 63 | 12 | 82.43 (56.84; 108.02) | 0.16 (0.09; 0.31) | 7.05 |
| Total | 91 | 45 | 54.39 (31.20; 77.57) | 0.42 (0.29; 0.61) | 6.72 |
| Frequency | |||||
| Incorrect | 20 | 14 | 35.43 (−19.27; 90.14) | 0.64 (0.32; 1.28) | 0.96 |
| Omitted/illegible | 27 | 1 | 96.58 (58.96; 134.21) | 0.03 (0.00; 0.24) | 3.54 |
| Total | 47 | 15 | 70.56 (36.21; 101.91) | 0.28 (0.16; 0.51) | 4.50 |
| Pharmaceutical form | |||||
| Incorrect | 1 | 0 | 100 (−95.87; 295.87) | – | 0.14 |
| Omitted/illegible | 29 | 2 | 93.64 (56.89; 130.38) | 0.06 (0.01; 0.26) | 3.68 |
| Total | 30 | 2 | 93.85 (57.78; 129.92) | 0.06 (0.01; 0.25) | 3.82 |
| Administration route | |||||
| Incorrect | 2 | 0 | 100 (−38.40; 238.40) | – | 0.27 |
| Omitted/illegible | 41 | 3 | 93.25 (62.54; 123.96) | 0.06 (0.02; 0.21) | 5.19 |
| Total | 43 | 3 | 93.56 (63.66; 123.47) | 0.06 (0.02; 0.20) | 5.46 |
| TOTAL | 144 | 73 | 53.24 (35.37; 71.11) | 0.41 (0.31; 0.56) | 10.40 |
The statistically significant results are in bold.
ARR: absolute risk reduction; EAP: electronically assisted prescription; CI: 95%; MP: manual prescription; OR: odds ratio; RRR: relative risk reduction.
A statistical analysis was performed with Stata 10.0 software to check whether the statistical significance was affected by the number of lines in each MO, sex or age of the patient.
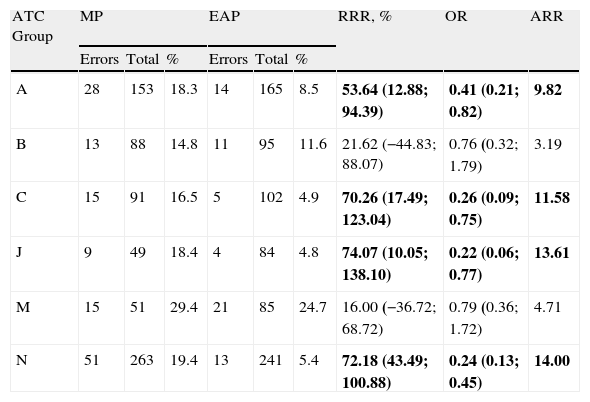
Table 2 shows the errors by therapeutic groups. The high number of drug errors in group N (central nervous system) and the decrease in the error percentage for all therapeutic groups with EAP is noticeable.
Types of Errors According to the ATC Classification.
| ATC Group | MP | EAP | RRR, % | OR | ARR | ||||
| Errors | Total | % | Errors | Total | % | ||||
| A | 28 | 153 | 18.3 | 14 | 165 | 8.5 | 53.64 (12.88; 94.39) | 0.41 (0.21; 0.82) | 9.82 |
| B | 13 | 88 | 14.8 | 11 | 95 | 11.6 | 21.62 (−44.83; 88.07) | 0.76 (0.32; 1.79) | 3.19 |
| C | 15 | 91 | 16.5 | 5 | 102 | 4.9 | 70.26 (17.49; 123.04) | 0.26 (0.09; 0.75) | 11.58 |
| J | 9 | 49 | 18.4 | 4 | 84 | 4.8 | 74.07 (10.05; 138.10) | 0.22 (0.06; 0.77) | 13.61 |
| M | 15 | 51 | 29.4 | 21 | 85 | 24.7 | 16.00 (−36.72; 68.72) | 0.79 (0.36; 1.72) | 4.71 |
| N | 51 | 263 | 19.4 | 13 | 241 | 5.4 | 72.18 (43.49; 100.88) | 0.24 (0.13; 0.45) | 14.00 |
The statistically significant results are in bold.
%: Percentage error; A: digestive and metabolic system; EAP: electronically assisted prescription; ARR: absolute risk reduction; B: blood and haematopoietic organs; C: cardiovascular system; CI: 95%; J: systemic anti-infective therapy; M: musculoskeletal system; MP: manual prescription; N: central nervous system; OR: odds ratio; RRR: relative risk reduction; Total: total number of times this treatment group was prescribed.
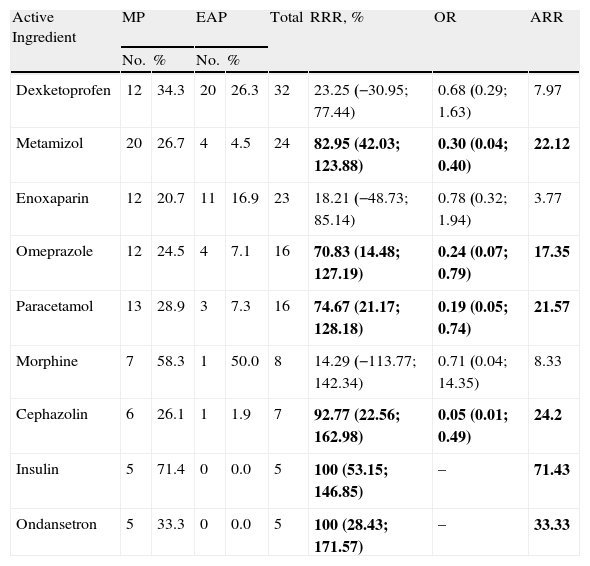
Table 3 shows the prescribing error results by active ingredient.
Prescription Errors by Active Ingredient.
| Active Ingredient | MP | EAP | Total | RRR, % | OR | ARR | ||
| No. | % | No. | % | |||||
| Dexketoprofen | 12 | 34.3 | 20 | 26.3 | 32 | 23.25 (−30.95; 77.44) | 0.68 (0.29; 1.63) | 7.97 |
| Metamizol | 20 | 26.7 | 4 | 4.5 | 24 | 82.95 (42.03; 123.88) | 0.30 (0.04; 0.40) | 22.12 |
| Enoxaparin | 12 | 20.7 | 11 | 16.9 | 23 | 18.21 (−48.73; 85.14) | 0.78 (0.32; 1.94) | 3.77 |
| Omeprazole | 12 | 24.5 | 4 | 7.1 | 16 | 70.83 (14.48; 127.19) | 0.24 (0.07; 0.79) | 17.35 |
| Paracetamol | 13 | 28.9 | 3 | 7.3 | 16 | 74.67 (21.17; 128.18) | 0.19 (0.05; 0.74) | 21.57 |
| Morphine | 7 | 58.3 | 1 | 50.0 | 8 | 14.29 (−113.77; 142.34) | 0.71 (0.04; 14.35) | 8.33 |
| Cephazolin | 6 | 26.1 | 1 | 1.9 | 7 | 92.77 (22.56; 162.98) | 0.05 (0.01; 0.49) | 24.2 |
| Insulin | 5 | 71.4 | 0 | 0.0 | 5 | 100 (53.15; 146.85) | – | 71.43 |
| Ondansetron | 5 | 33.3 | 0 | 0.0 | 5 | 100 (28.43; 171.57) | – | 33.33 |
The statistically significant results are in bold. Results using a confidence interval of 95%.
%: Error percentage of the times prescribed; EAP: electronically assisted prescription; ARR: absolute risk reduction; MP: manual prescription; No.: number of errors; OR: odds ratio; RRR: relative risk reduction; Total: total errors for each active ingredient.
The percentage of errors in the MEDG prescription was less than in the MEDNG prescription (8.9% versus 14.3% with EAP, and 18.5% versus 46.4% with MP). When comparing MEDNG prescription between both systems, there was a statistically significant reduction of errors with EAP (69.23%), with an OR of 0.19 (0.06, 0.60) compared to MP.
DiscussionThis study detected a 53% decrease in treatment line prescribing errors with EAP. The prescription error rate is very variable in different studies, due to differences in the patient sample selected, the field of study and different concepts of error used. Our study was conducted in a surgical unit with a high quantity of transitional care, which we, and other authors,14 believe is a risk factor for increased prescribing errors.
An error in the doctor's signature was the most frequent in the manual MO. Calligaris et al. found that 50% of prescriptions were not signed or dated.15 By introducing EAP, patient identification and MO errors virtually disappeared.4 In our study, the reduction was more moderate, as the doctors probably found it difficult to record the allergies of the patients in the software. This error constituted 100% of the patient identification and MO errors with EAP.
MP treatment line errors were mainly related to incomplete or illegible prescriptions, regarding dose, frequency, route of administration and dosage form, which coincides with those described by Bates et al.16 and other Spanish studies.4 It has been shown that setting a default dose and frequency in EAP can reduce up to 42% of prescribing errors.17
The reduction in the error rate for Group N was very significant with EAP, as analgesics are prescribed in full, with the administration route and pharmaceutical form being specified. In our study, painkillers and some antibiotics were the drugs with more prescribing errors, as found in other studies.7,16
The largest number of errors occurred with dexketoprofen, as the dose was not always adjusted to renal function and/or age as indicated in the technical data sheet. Our EAP system has no support for the dose adjustment according to renal function, and such a system could lead to an improvement in the prescription of nephrotoxic drugs, as indicated by Chertow et al.6 This is an improvement that we must consider in future versions of our prescription system in the short term.
It is also worth noting that 3 of the 9 active ingredients with the most errors (enoxaparin, insulin and morphine) are considered high-risk drugs,18 which has also been published by other authors.19
The error rate in prescribing MEDNG was higher than for MEDG, but this difference was statistically significant only with MP. We believe that using EAP to prescribe MEDNG means that the doctor fills out all the details of dose, frequency, administration route and pharmaceutical form. In short, we must ensure that the prescription of treatments complies with pharmacotherapeutic guidelines, which are constantly being updated by the Pharmacy and Therapeutics Committee.
Furthermore, we strongly believe that the 5 months that elapsed between starting the EAP system and data collection was sufficient to avoid learning curve errors described by some authors,20 especially with the high number of errors found in the study by Delgado et al.5
As a limitation of our study, the number of MO analysed was small. Other studies have included more than 35000 medical orders with data collection between 3 and 5 years.3,7 In addition, we made no study of agreement for the identification of errors, although the data were reviewed by two pharmacists with experience in the field of ME. It must also be noted that it was not reviewed whether these errors reached the patient.
We conclude that EAP is a proven useful tool in reducing prescribing errors in hospitalised surgical patients.
Conflicts of interestThe authors declare they have no conflicts of interest.
We would like to thank the hospital Statistics Department, and especially Dr. Alfonso Muriel, for their assistance in measuring and interpreting the results.
Please cite this article as: Vélez-Díaz-Pallarés M, et al. Análisis de errores de la prescripción manual comparados con la prescripción electrónica asistida en pacientes traumatológicos. Farm Hosp. 2011;35(3):135–139.