The Team Strategies and Tools to Enhance Performance and Patient Safety (TeamSTEPPS®) programme has been shown to improve interprofessional work among healthcare professionals by enhancing teamwork. Intensive care professionals were trained in this methodology through the course “Simulation Trainer: Improving Teamwork through TeamSTEPPS®”.
ObjectivesTo analyse the teamwork performance and good practice in simulation of the intensive care professionals attending the course and to explore their perceptions of the training experience carried out during the course.
MethodsA cross-sectional descriptive and phenomenological study was carried out using a mixed methodology. The 18 course participants were administered the questionnaires “TeamSTEPPS™ 2.0 Team Performance Observation Tool” to evaluate teamwork performance and “Educational Practices Questionnaire” for good practices in simulation after the simulated scenarios. Subsequently, a group interview was conducted through a focus group with 8 attendees using the Zoom™ videoconferencing platform. A thematic and content analysis of the discourses was carried out using the interpretative paradigm. Quantitative and qualitative data were analysed using IBM SPSS Statistics™ 27.0 and MAXQDA Analytics Pro™ respectively.
ResultsBoth the level of teamwork performance (mean = 96.25; SD = 8.257) and good practice in simulation (mean = 75; SD = 1.632) following the simulated scenarios were adequate. The following main themes were identified: satisfaction with the TeamSTEPPS® methodology, usefulness of the methodology, barriers to methodology implementation and non-technical skills improved through TeamSTEPPS®.
ConclusionsTeamSTEPPS® methodology can be a good interprofessional education strategy for the improvement of communication and teamwork in intensive care professionals, both at the care level (through on-site simulation strategies) and at the teaching level (through its inclusion in the students' curriculum).
El programa Team Strategies and Tools to Enhance Performance and Patient Safety (TeamSTEPPS®) ha demostrado mejorar el trabajo interprofesional entre los profesionales sanitarios mejorando el trabajo en equipo. Se formó a profesionales de cuidados intensivos en esta metodología mediante el Curso “Instructor/a en simulación: Mejorando el Trabajo en Equipo a Través de TeamSTEPPS®”.
ObjetivosAnalizar el desempeño del trabajo en equipo y las buenas prácticas en simulación de los profesionales de cuidados intensivos asistentes al curso y explorar sus percepciones sobre la experiencia formativa llevada cabo durante el mismo.
MétodosSe llevó a cabo un estudio descriptivo transversal y fenomenológico mediante una metodología mixta. Se aplicaron a los 18 asistentes al curso los cuestionarios “TeamSTEPPS™ 2.0 Team Performance Observation Tool” para evaluar el desempeño del trabajo en equipo y “Educational Practices Questionnaire” para las buenas prácticas en simulación tras los escenarios simulados. Posteriormente se realizó una entrevista grupal a través de un grupo focal a 8 asistentes mediante la plataforma de videoconferencias Zoom™. Se realizó un análisis temático y de contenido de los discursos desde el paradigma interpretativo. Los datos cuantitativos y cualitativos se analizaron mediante los programas IBM SPSS Statistics™ 27.0 y MAXQDA Analytics Pro™ respectivamente.
ResultadosTanto el nivel de desempeño del trabajo en equipo (media = 96,25; DT = 8,257) como las buenas prácticas en simulación (media = 75; DT = 1,632) tras los escenarios simulados fueron adecuados. Se identificaron los siguientes temas principales: satisfacción con la metodología TeamSTEPPS®, utilidad de la metodología, barreras de implementación de la misma y habilidades no técnicas mejoradas a través del TeamSTEPPS®.
ConclusionesLa metodología TeamSTEPPS® puede ser una buena estrategia de educación interprofesional para la mejora de la comunicación el trabajo en equipo en profesionales de cuidados intensivos, tanto a nivel asistencial (mediante estrategias de simulación in situ), como a nivel docente (mediante su inclusión en el curriculum de los estudiantes).
Adverse events, defined as situations that result in unintended patient harm, are one of the major problems facing healthcare systems worldwide.1,2 Since it is impossible to completely eliminate the probability of errors in any human activity, it is necessary to understand and intervene in the conditions in which human beings work in order to minimise the risk, thus improving prevention mechanisms.3 The Joint Commission identifies errors in communication and teamwork as one of the most frequent causes of sentinel events, when severe harm to the patient's health or life occurs, with the risk of death and serious consequences, or the possibility of serious consequences in the future.4 Consequently, a growing body of research has focused on recognising and analysing the mediation of some human factors in patient safety, such as teamwork skills.2,5
One of the most important interventions in this area is the programme designed by the Agency for Healthcare Research and Quality (AHRQ), a quality and safety organisation of the US federal government, called Team Strategies and Tools to Enhance Performance and Patient Safety (TeamSTEPPS®) which has been developed in collaboration with the patient safety programme of the US Department of Defense. The TeamSTEPPS®-based programme was created in 2006, updated to version 2.0 in 2012, and is designed to improve the work dynamic among healthcare professionals and help improve the working environment among healthcare team members, encouraging a culture of patient safety and teamwork.6 Information on the programme is available in Spanish on the AHRQ website (https://www.ahrq.gov/es/informacion-en-espanol/index.html).
The TeamSTEPPS®-based training programme develops five teamwork competencies7:
- •
Team structuring: organisation of the team in the definition of roles and responsibilities within a unit or for a specific action.
- •
Leadership: ability to lead and coordinate other team members, evaluate their behaviour, assign tasks, motivate subordinates, plan and organise work to achieve a good atmosphere and encourage continuous improvement processes.
- •
Mutual support: ability to give appropriate and effective feedback to improve team members' behaviour or when a lapse is detected; assisting a colleague in time and completing or supporting another colleague's task when he/she is overloaded.
- •
Situational awareness: constant observation of the execution of tasks, to anticipate possible errors, follow the behaviour of team members, ensure that work is being done according to plan and that procedures and objectives are being followed.
- •
Communication: effective transmission of messages in health care, including conveying important messages to the team, checking that the receiver receives and understands them properly, exchanging all necessary information in a care process, and using appropriate language so that the message is received.
The review by Parker et al.8 showed that TeamSTEPPS®-based training programmes decrease the number of errors in healthcare, improve communication between healthcare professionals and increase patient satisfaction. Furthermore, other reviews have shown that these programmes enhance interprofessional work among healthcare professionals by improving teamwork and communication among team members9,10 These results have also been observed in nursing students, describing improvements in their attitudes towards teamwork11,12 especially interprofessional work between medical and nursing students to work as a team.13,14
In terms of previous studies of nurses caring for critically ill patients, TeamSTEPPS®-based training programmes have been found to improve communication skills, patient safety and teamwork in emergency nurses15–17 and in neonatal,18 paediatric19 and adult intensive care nurses.20,21
However, it should be highlighted that these positive effects have been found mainly when the teaching methodology of clinical simulation is used as a teaching methodology for training and coaching in the TeamSTEPPS® programme.9,10 According to the Dictionary of Health Simulation,22 clinical simulation is defined as “a technique that creates a situation or environment to allow people to experience a representation of a real event in order to practice, learn, evaluate, test or understand human systems or actions”. Clinical simulation has been shown to be an effective teaching methodology to improve the acquisition of nursing competencies.23,24 This methodology is effective in improving learning outcomes in nursing education25 and clinical nursing reasoning.26 Clinical simulation has also been shown to develop the acquisition of both technical24 and non-technical skills needed in the nursing profession, such as empathy,27 communication,28 interprofessional work29 and teamwork.30
To date, no experience had been carried out to educate and train intensive care professionals in Spain in a programme based on TeamSTEPPS® using clinical simulation as a teaching methodology. However, the Simulation Working Group of the Spanish Society of Intensive Care Nursing and Coronary Units (SEEIUC) organised the course “Simulation Instructor: Improving Teamwork through TeamSTEPPS®”, accredited with 15 ECTS by the University of Barcelona and by the Spanish Society of Clinical Simulation and Patient Safety (SESSEP). This course was aimed at intensive and critical care professionals, both in healthcare and teaching, and was held as a pre-congress course within the framework of the XLVI National Congress of the SEEIUC held from 30 May to 2 June 2021 in Barcelona. In this way, this training allowed attendees to develop a new line of interventions and research in Spain, intended to provide them with knowledge not only to improve their own competencies, but also to train these skills in healthcare professionals, as well as to lead change management processes based on TeamSTEPPS®, aimed at improving teamwork, well-being at work and improving the quality and safety provided to patients.
Therefore, the objectives of our study were to analyse the teamwork performance and good practice in simulation of the intensive and critical care professionals attending the course, as well as to explore their perceptions of the training experience carried out during the course.
MethodDesignA cross-sectional descriptive and phenomenological study was carried out using a mixed methodology in which both quantitative and qualitative data were analysed with the intention of evaluating teamwork, good simulation practices and participants' perceptions.
ScopeThe study was carried out in the classroom session of the course “Simulation Instructor: Improving teamwork through TeamSTEPPS®” on 29 and 30 May 2021 in Barcelona. One week later, a videoconference was held through the platform Zoom™ with those attending the course who wished to participate voluntarily.
SubjectsThe 18 intensive and critical care professionals (assistants and teachers) who attended the course were included in the study for the collection of quantitative data. Subsequently, eight course attendees voluntarily participated in a focus group for the collection of qualitative data and were contacted by e-mail.
Course structure and clinical simulation sessionsThe course included four thematic blocks, the first three of which were taught online through a Moodle platform and the last one in person:
Thematic block 1: Basic concepts for being an instructor. Simulation-based learning methodology. It included the basics of clinical simulation teaching methodology to become a clinical simulation instructor.
Thematic block 2: Interprofessional team training based on TeamSTEPPS®. It included six modules, each of which consisted of two 7−10 min videos and practical activities on the tools included in the TeamSTEPPS® programme, and which were taught by a psychologist who is an AHRQ-accredited expert in the programme.
Thematic block 3: Design your own scenario. Course participants designed a simulated clinical scenario using a validated GRISANE31 grid, focused on the training of non-technical skills.
Thematic block 4: Applied simulation: practical scenario. From the simulated clinical scenarios designed by the course participants, four were selected and staged in the classroom session of the course. These scenarios were as follows:
Scenario 1: Adverse event during the hygiene of the critical patient when the orderly faints and accidentally pulls out the endotracheal tube and the central line.
Scenario 2: Medication error when confusing vasoactive drugs in a post-surgical patient after cardiac surgery.
Scenario 3: Weaning process of a patient addicted to drugs and manifesting hyperactive delirium after extubation.
Scenario 4: Management of intracranial hypertension due to accidental closure of external ventricular drainage in a neurocritical patient.
Four clinical simulation sessions (two hours and 20 min each) were held during the classroom session of the course with the following structure:
Prebriefing (20 min): role description, environment and equipment, confidentiality, fictional contract, roles within the simulated scenario, psychological safety and session structure.
Simulated clinical scenario (30 min): the previous simulated clinical scenarios were staged. It should be noted that in the first two scenarios the high-fidelity simulator SimMan Essential® from Laerdal Medical AS (USA) was used to represent the critically ill patient, while in the last two scenarios an actor, also called a standardised patient, played the role of the critically ill patient. Each scenario involved four to five course participants, including the course designer, who acted as the course instructor. In addition, all the above scenarios involved actors, also called confederates, representing a health professional (doctor, orderly or auxiliary nursing care technician). While a group of participants were acting out a scenario, the rest of the participants were observing it in the same simulation room.
Debriefing (90 min): after the staging of each simulated clinical case, participants' clinical performance was analysed and reflected upon, based on teamwork and communication using the TeamSTEPPS® programme.
Measurement toolsTeam workThe TeamSTEPPS® 2.0 Team Performance Observation Tool (TPOT) questionnaire was used to assess the teamwork performance of participants in each simulated clinical scenario. This questionnaire was designed by AHRQ.32 The TeamSTEPPS® 2.0 TPOT consists of 23 items assessing team structure (four items) and the four competencies included in teamwork: communication (four items), leadership (six items), situational awareness (five items) and mutual support (four items). Each item is assessed on a Likert-type scale with five response options (from 1 = very poor to 5 = excellent). The total score of the questionnaire ranges from 23 to 115 points. The higher the score, the better the teamwork performed by the participants. Maguire33 obtained a Cronbach's coefficient α of .98 for the total score of the questionnaire. The original version of the AHRQ32 translated and back-translated by the research team was used in this study.
Good practices in simulationThe Educational Practices Questionnaire (EPQ) was used to assess the presence of good practice in simulation as perceived by the participants in each of the clinical simulation sessions conducted. This questionnaire was developed by the National League for Nursing34 in collaboration with Laerdal Medical AS. The EPQ consists of 16 items divided into four dimensions: active learning (10 items), collaboration (two items), diversity of learning (two items) and expectations (two items). Each item is assessed on a Likert-type scale with five response options (from 1 = strongly disagree to 5 = strongly agree). The total score of the questionnaire ranges from 16 to 80 points. The higher the score, the higher the recognition and presence of good teaching practices in simulation. The same questionnaire not only makes it possible to evaluate the presence of good practices in simulation, but also their importance for simulation. Regarding the reliability of the EPQ, the original authors obtained a Cronbach's coefficient α of .86. The EPQ has been cross-culturally adapted and validated in Spanish,35 obtaining a Cronbach's α of .89.
Data collectionThe TeamSTEPPS® 2.0 TPOT and EPQ questionnaires were administered during the face-to-face session of the course on 29 and 30 May 2021 and were collected by a member of the research team after the completion of each of the simulated clinical scenarios. Subsequently, course attendees were contacted via personal email to ask for their voluntary participation in the second part of the study. One week later, a focus group interview was conducted with eight course participants via the videoconferencing platform Zoom™, to gather their perceptions after the TeamSTEPPS®-based clinical simulation training programme. All participants attended voluntarily and were informed in advance of the study and the recording of the session, giving their verbal consent. The four open-ended questions that guided the focus group interview were: 1) What is your level of satisfaction with the course? 2) Why do you think the TeamSTEPPS® programme through clinical simulation is useful? 3) What difficulties, barriers or limitations do you think you will have when implementing this programme in your workplace; and 4) What non-technical skills have you learned to improve through this programme? The group interview lasted 75 min and was conducted by a member of the research team.
Data analysisFirst, the quantitative data were analysed using IBM SPSS Statistics version 28.0 software (IBM Corp., Armonk, NY, USA), obtaining descriptive statistics for both the socio-demographic data of the participants and the items of the two questionnaires administered. Secondly, qualitative data were extracted from the responses to the four open-ended questions posed to the focus group. Participants' responses were coded and participants were labelled numerically in order of the appearance of their responses in the group interview, with their narratives preceded by the letter P (participant). A content analysis of the discourses extracted from the interpretative paradigm,36 was carried out, with a thematic analysis of the discourses following Braun and Clarke's proposal.37,38 These analyses were assisted by MAXQDA 18 software (VERBI Software, Berlin, Germany). Two researchers transcribed the group interview material, coded the data, identified categories and subcategories that emerged during the analysis process, eliminated data that provided redundant information, and reviewed the data again to identify new and emerging subcategories.36 The categories identified at the outset corresponded to the four open-ended questions asked in the group interview. Subsequently, new Subcategories emerged from the participants' perceptions. Finally, the emerging subcategories were saturated during the content analysis.
Ethical considerationsThis study was conducted in accordance with the ethical principles and international recommendations of the Declaration of Helsinki.39 The principles of beneficence, non-maleficence, autonomy and justice were adhered to. All participants did so voluntarily and the confidentiality of their data and responses was safeguarded throughout the process. The questionnaires, databases and focus group recordings are stored in digital folders with a password by the lead researcher of the project. It should be noted that the quantitative data collected through the questionnaires were part of the course evaluation and learning outcomes, while the qualitative data collected in the focus group interview were part of the measurement of attendees' satisfaction after the course.
ResultsThe course was attended by a total of 18 intensive and critical care professionals (16 nursing professionals and two medical professionals) from Catalonia, the Basque Country, the Balearic Islands, the Community of Madrid and the Community of Valencia. Most of the participants were women (n = 10; 55.6%), and the rest were men (n = 8; 44.4%) aged between 24 and 54 years (mean = 38; SD = 8.026). Most of the professionals were working in intensive and critical care units (n = 15; 83.3%), while the rest were teaching at the university (n = 3; 16.7%). Of the total number of course attendees, 8 (44.4%) voluntarily participated in the focus group interview.
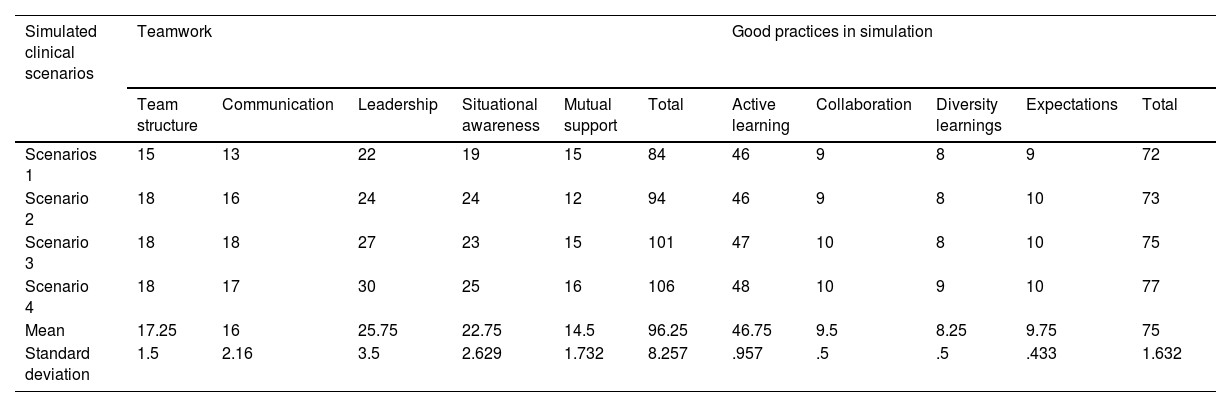
Regarding the quantitative analysis of the data, Table 1 shows the descriptive statistics obtained in the analysis of the TeamSTEPPS® 2.0 TPOT and EPQ questionnaires in each of the four simulated clinical scenarios. This table shows that in all of them, participants obtained high scores, both in the dimensions and in the total scores of both questionnaires that assessed teamwork (mean = 96.25; SD = 8.257) and good practice in simulation (mean = 75; SD = 1.632). It should be noted that, in most cases, the scores obtained after the simulated clinical scenario are higher in both questionnaires as the questionnaires progress, both in their respective dimensions and in their total scores. In this sense, the total scores from the first to the last simulated clinical scenario went from 84 to 106 points in teamwork, while in good practice in simulation they went from 72 to 77 points.
Descriptive statistics obtained in the questionnaires that measured teamwork and good practice in simulation in the four simulated clinical scenarios.
| Simulated clinical scenarios | Teamwork | Good practices in simulation | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Team structure | Communication | Leadership | Situational awareness | Mutual support | Total | Active learning | Collaboration | Diversity learnings | Expectations | Total | |
| Scenarios 1 | 15 | 13 | 22 | 19 | 15 | 84 | 46 | 9 | 8 | 9 | 72 |
| Scenario 2 | 18 | 16 | 24 | 24 | 12 | 94 | 46 | 9 | 8 | 10 | 73 |
| Scenario 3 | 18 | 18 | 27 | 23 | 15 | 101 | 47 | 10 | 8 | 10 | 75 |
| Scenario 4 | 18 | 17 | 30 | 25 | 16 | 106 | 48 | 10 | 9 | 10 | 77 |
| Mean | 17.25 | 16 | 25.75 | 22.75 | 14.5 | 96.25 | 46.75 | 9.5 | 8.25 | 9.75 | 75 |
| Standard deviation | 1.5 | 2.16 | 3.5 | 2.629 | 1.732 | 8.257 | .957 | .5 | .5 | .433 | 1.632 |
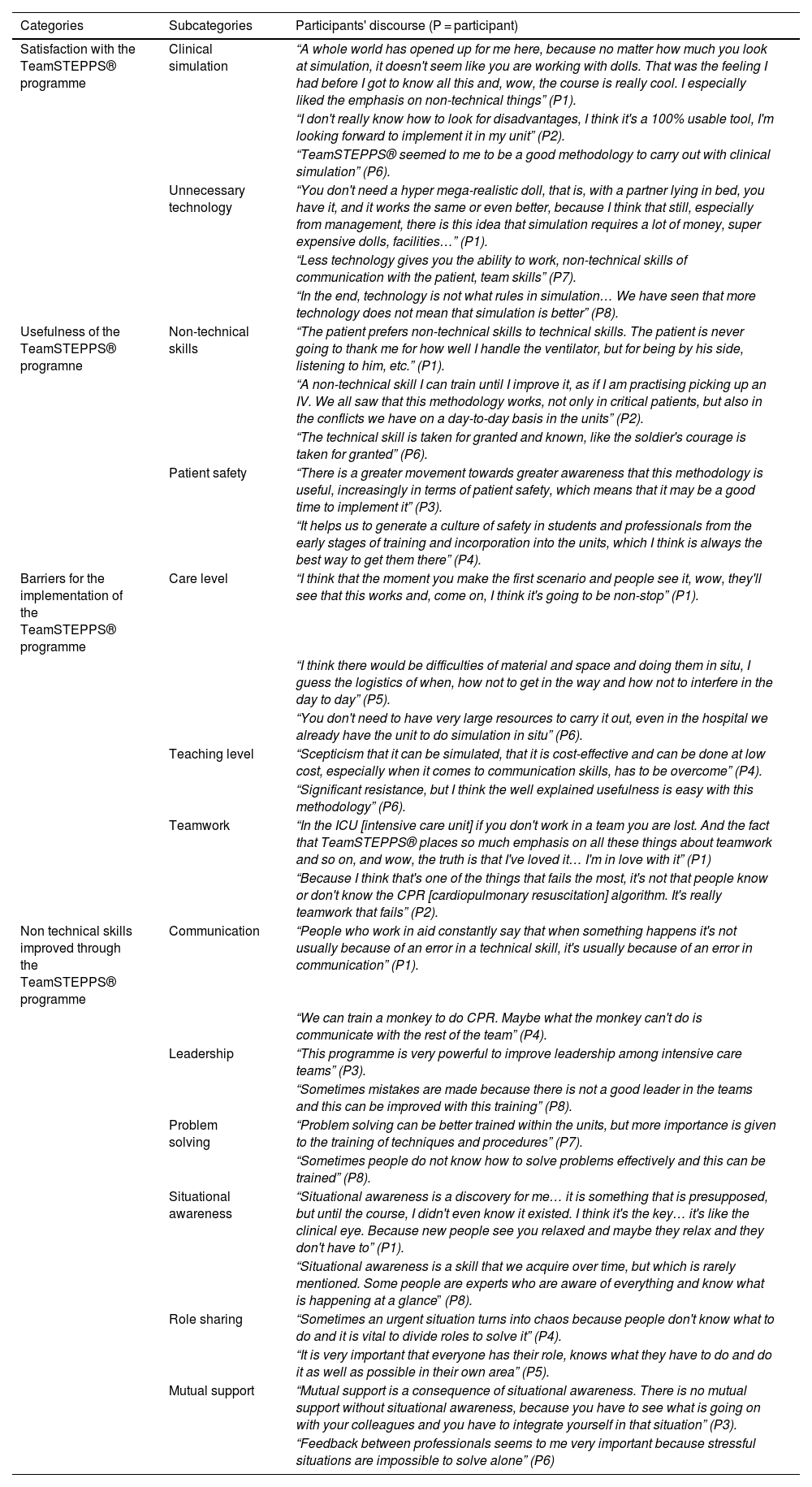
Regarding the qualitative analysis of the data, four main thematic categories and their corresponding 13 subcategories emerged from the four open-ended questions asked to the focus group, all of them supported by the participants' narratives (Table 2).
Main thematic categories and their corresponding subcategories supported by the most relevant narratives collected from participants' discourse.
| Categories | Subcategories | Participants' discourse (P = participant) |
|---|---|---|
| Satisfaction with the TeamSTEPPS® programme | Clinical simulation | “A whole world has opened up for me here, because no matter how much you look at simulation, it doesn't seem like you are working with dolls. That was the feeling I had before I got to know all this and, wow, the course is really cool. I especially liked the emphasis on non-technical things” (P1). |
| “I don't really know how to look for disadvantages, I think it's a 100% usable tool, I'm looking forward to implement it in my unit” (P2). | ||
| “TeamSTEPPS® seemed to me to be a good methodology to carry out with clinical simulation” (P6). | ||
| Unnecessary technology | “You don't need a hyper mega-realistic doll, that is, with a partner lying in bed, you have it, and it works the same or even better, because I think that still, especially from management, there is this idea that simulation requires a lot of money, super expensive dolls, facilities…” (P1). | |
| “Less technology gives you the ability to work, non-technical skills of communication with the patient, team skills” (P7). | ||
| “In the end, technology is not what rules in simulation… We have seen that more technology does not mean that simulation is better” (P8). | ||
| Usefulness of the TeamSTEPPS® programne | Non-technical skills | “The patient prefers non-technical skills to technical skills. The patient is never going to thank me for how well I handle the ventilator, but for being by his side, listening to him, etc.” (P1). |
| “A non-technical skill I can train until I improve it, as if I am practising picking up an IV. We all saw that this methodology works, not only in critical patients, but also in the conflicts we have on a day-to-day basis in the units” (P2). | ||
| “The technical skill is taken for granted and known, like the soldier's courage is taken for granted” (P6). | ||
| Patient safety | “There is a greater movement towards greater awareness that this methodology is useful, increasingly in terms of patient safety, which means that it may be a good time to implement it” (P3). | |
| “It helps us to generate a culture of safety in students and professionals from the early stages of training and incorporation into the units, which I think is always the best way to get them there” (P4). | ||
| Barriers for the implementation of the TeamSTEPPS® programme | Care level | “I think that the moment you make the first scenario and people see it, wow, they'll see that this works and, come on, I think it's going to be non-stop” (P1). |
| “I think there would be difficulties of material and space and doing them in situ, I guess the logistics of when, how not to get in the way and how not to interfere in the day to day” (P5). | ||
| “You don't need to have very large resources to carry it out, even in the hospital we already have the unit to do simulation in situ” (P6). | ||
| Teaching level | “Scepticism that it can be simulated, that it is cost-effective and can be done at low cost, especially when it comes to communication skills, has to be overcome” (P4). | |
| “Significant resistance, but I think the well explained usefulness is easy with this methodology” (P6). | ||
| Teamwork | “In the ICU [intensive care unit] if you don't work in a team you are lost. And the fact that TeamSTEPPS® places so much emphasis on all these things about teamwork and so on, and wow, the truth is that I've loved it… I'm in love with it” (P1) | |
| “Because I think that's one of the things that fails the most, it's not that people know or don't know the CPR [cardiopulmonary resuscitation] algorithm. It's really teamwork that fails” (P2). | ||
| Non technical skills improved through the TeamSTEPPS® programme | Communication | “People who work in aid constantly say that when something happens it's not usually because of an error in a technical skill, it's usually because of an error in communication” (P1). |
| “We can train a monkey to do CPR. Maybe what the monkey can't do is communicate with the rest of the team” (P4). | ||
| Leadership | “This programme is very powerful to improve leadership among intensive care teams” (P3). | |
| “Sometimes mistakes are made because there is not a good leader in the teams and this can be improved with this training” (P8). | ||
| Problem solving | “Problem solving can be better trained within the units, but more importance is given to the training of techniques and procedures” (P7). | |
| “Sometimes people do not know how to solve problems effectively and this can be trained” (P8). | ||
| Situational awareness | “Situational awareness is a discovery for me… it is something that is presupposed, but until the course, I didn't even know it existed. I think it's the key… it's like the clinical eye. Because new people see you relaxed and maybe they relax and they don't have to” (P1). | |
| “Situational awareness is a skill that we acquire over time, but which is rarely mentioned. Some people are experts who are aware of everything and know what is happening at a glance” (P8). | ||
| Role sharing | “Sometimes an urgent situation turns into chaos because people don't know what to do and it is vital to divide roles to solve it” (P4). | |
| “It is very important that everyone has their role, knows what they have to do and do it as well as possible in their own area” (P5). | ||
| Mutual support | “Mutual support is a consequence of situational awareness. There is no mutual support without situational awareness, because you have to see what is going on with your colleagues and you have to integrate yourself in that situation” (P3). | |
| “Feedback between professionals seems to me very important because stressful situations are impossible to solve alone” (P6) |
This category was related to satisfaction with both the simulation teaching methodology as perceived by the course participants and the lack of need for technology to carry out the TeamSTEPPS® programme.
Subcategory 1.1: clinical simulationMost of the participants expressed their satisfaction with the fact that the TeamSTEPPS® programme was conducted through the clinical simulation methodology, especially the first-time users, who had preconceived ideas about this methodology and were pleasantly surprised.
Subcategory 1.2: unnecessary technologyCourse attendees reported that they were satisfied that it was not necessary to conduct a TeamSTEPPS® based training programme with the technology that is often associated with the clinical simulation methodology. This also came as a surprise to participants who associated this methodology with technology, having a preconceived idea of clinical simulation.
Category 2: usefulness of the TeamSTEPPS® programmeThis category related to the usefulness of this programme both for acquiring non-technical skills and for promoting patient safety.
Subcategory 2.1: non-technical skillsMost participants expressed that the TeamSTEPPS® based training programme was useful for learning non-technical skills, underlining the fact that non-technical skills can also be trained as well as technical and procedural skills, which are the most important skills in the clinical setting.
Subcategory 2.2: patient safetyParticipants also stated that this programme is useful in fostering a culture of patient safety, not only among students, but also among nursing professionals.
Category 3: barriers for implementation of the TeamSTEPPS® programmeThose attending the course identified these barriers at both the care and teaching levels, regardless of whether they were nursing professionals or teachers. However, most of them made proposals to solve these barriers in each area.
Subcategory 3.1: attendee levelThe main barriers identified at this level were related to material, space and not interfering with daily clinical practice. However, conducting the simulations in situ in the units was identified as an advantage.
Subcategory 3.2: teaching levelAt this level, scepticism and resistance were the main barriers identified, although the cost-effectiveness and usefulness of this methodology in overcoming these barriers is underlined.
Category 4: non-technical skills improved through the TeamSTEPPS® programmeThe majority of course attendees expressed that they improved their teamwork, communication, leadership, problem solving, situational awareness, role sharing and mutual support skills through the TeamSTEPPS® based training programme.
Subcategory 4.1: team workParticipants expressed the importance of teamwork in intensive care units and its improvement through this programme, as it is an aspect that often fails in clinical practice.
Subcategory 4.2: communicationThe participants also stressed that communication errors often occur in practice and that this type of training improves communication between team members so that these errors do not occur.
Subcategory 4.3: leadershipThe course participants expressed that mistakes are also made in intensive care units due to a lack of leadership, but that this can be improved through this training programme.
Subcategory 4.4: problem solvingMost of the course attendees stated that problem-solving skills can also be trained through this programme, as they sometimes know how to solve problems in intensive care units.
Subcategory 4.5: situational awarenessThis dimension of teamwork was a key element for most of the participants, being identified as a skill that expert professionals have and that can be trained through this TeamSTEPPS®-based training programme.
Subcategory 4.6: role sharingFurthermore, the participants stated that this programme allows the training of role sharing which is highly necessary in emergency situations.
Subcategory 4.7: mutual supportFinally, course participants identified this dimension of work as another non-technical skill that they had improved through the programme, highlighting its relevance in coping with stressful situations, but that the skill of situational awareness is necessary to carry it out.
DiscussionTo date, no training programme based on TeamSTEPPS® had been carried out in Spain using clinical simulation methodology aimed at intensive and critical care professionals. Our first training experience with this programme indicates that the professionals attending the course reached adequate levels, both in teamwork performance and in good simulation practices after the staging of the simulated clinical cases. Likewise, these professionals perceived the training experience positively, expressing their satisfaction with the programme, its usefulness, the barriers to its implementation and the non-technical skills improved through the TeamSTEPPS® training programme.
Firstly, the professionals attending the course achieved adequate levels of teamwork after training and coaching with the TeamSTEPPS® programme, as previous studies have found with healthcare professionals,9–14 and specifically with those dedicated to the care of critically ill patients.15–21 All previous studies have shown the importance of interprofessional education in order to train teamwork. In this sense, interprofessional collaboration and training was recommended by the Institute of Medicine40 as an essential element to transform healthcare, because collaboration between different healthcare professionals has been shown to improve the quality of care and reduce costs.41 In addition, fewer errors are made when working in teams than individually, especially if each team member knows his or her responsibilities as well as those of the other team members.6 On the other hand, simulation has been identified as a suitable learning methodology for interprofessional education.42.43 However, interprofessional education has been shown to be more relevant in undergraduate training, as it prevents the early development of negative attitudes between different professions.44,45
Secondly, the professionals attending the course also reached adequate levels of good practice in simulation after the training received in the course, as it included a specific module on basic concepts for being an instructor in the simulation learning methodology. In this sense, the attendees showed their satisfaction after the simulations, valuing them positively. This result is also consistent with other previous studies that have shown good satisfaction and positive perceptions following the staging of simulated clinical cases.46–48
It should be noted that the levels of both teamwork and good simulation practice of the course participants increased progressively as the simulated clinical scenarios progressed. This increase in clinical performance is common in clinical simulation methodology, as participants in the simulations observe the performance of other participants before staging their clinical case, resulting in peer learning that leads to higher performance in the last simulated clinical cases.49,50 This increase may be due to the fact that participants learn from others and, in turn, teach them, wanting to do better than the participants who have already staged the simulated clinical case.50
Thirdly, the perceptions of the professionals attending the course were positive, focusing on various aspects of the training experience carried out. In this sense, participants were satisfied with the TeamSTEPPS® training programme, showing their satisfaction with the clinical simulation methodology and with the unnecessary use of technology. It should be noted that the attendees who were most satisfied were those who had hardly had any simulated experience. On the one hand, satisfaction with clinical simulation has been demonstrated in multiple studies.51 On the other hand, the common belief about this methodology is that in order to carry it out, a high-tech simulator and large technological resources are required. However, in our course we incorporated actors as simulated patients, also called standardised patients, demonstrating that simulation can be carried out with few resources, at low cost and with higher levels of fidelity.52
Likewise, the professionals attending the course expressed that the TeamSTEPPS® training programme was useful both for improving non-technical skills and patient safety, as has been previously demonstrated in studies based on this programme.9–21 This programme is especially useful for improving non-technical skills related to communication,8–10 being one of the skills that course attendees subsequently reported as having improved the most.
Although the professionals attending the course pointed out various barriers to the implementation of the TeamSTEPPS® training programme in their units or teaching centres, they did point out the advantages of carrying it out at these two levels. At the care level, the possibility of carrying out the simulations in situ in the intensive care units themselves, as they have the space and all the necessary material, was pointed out as one of the great advantages of this type of simulation. Previous studies have demonstrated the effectiveness of in situ simulation in improving teamwork53 and reducing patient morbidity and mortality.54 At the teaching level, those attending the course expressed the need to incorporate the TeamSTEPPS® training programme into the curriculum of health science students, overcoming the barrier to its implementation by demonstrating its cost-effectiveness and low cost to improve mainly non-technical skills (also known as soft skills), which are not usually trained in depth in healthcare degrees. The need for the implementation of such skills in the curriculum of healthcare students has already been proposed by several studies.55
Regarding the non-technical skills that the professionals attending the course perceived as having improved through the TeamSTEPPS® training programme, teamwork was the most highly valued, being perceived as one of the non-technical skills that most commonly fail in clinical healthcare practice. As already mentioned, this result is consistent with previous studies.9–21 The four teamwork competencies developed by the TeamSTEPPS®-based programme, i.e. communication, leadership, situational awareness and mutual support, were also perceived as improved non-technical skills by the course participants. This improvement is also documented by previous available evidence.8–10 Of note is the improvement in situational awareness skills, which course participants identified as the level reached by an expert nurse following Patricia Benner's model56 from intuitive to expert knowledge through critical reasoning.57 Finally, problem solving and role sharing were the other non-technical skills reported by course attendees to have improved, this result being congruent with previous studies previos.8–10
Regarding the four competencies developed by the TeamSTEPPS®-based programme for teamwork, i.e. communication, leadership, situational awareness and mutual support, these were also perceived as non-technical skills improved by the course participants. This improvement is also documented by previous available evidence.8–10 Of note is the improvement in situational awareness skills, which course attendees identified with the level reached by an expert nurse following Patricia Benner's model56 from intuitive to expert knowledge through critical reasoning.57 Finally, problem solving and role sharing were the other non-technical skills reported by course attendees to have improved, this result being congruent with previous studies.8–10
It should be noted that during the focus group interview, the TeamSTEPPS® training programme was compared with another teamwork training programme, the Crew Resource Management (CRM) programme.58 CRM is a more widespread training programme, mainly for training teams of emergency healthcare professionals.58 However, there is no universal CRM programme and it is based on the hierarchies found in healthcare organizations.59 However, the TeamSTEPPS® programme is a more complete tool for teamwork training in healthcare professionals in general, as the five skills trained in it include all the components of CRM, even adding new ones. Furthermore, TeamSTEPPS® is a universal and uniform training programme and is not based on hierarchical healthcare structures, with leadership being horizontal and not vertical.59
Finally, our study is not free of limitations, as it is the first pilot study carried out in Spain on the TeamSTEPPS® training programme aimed at intensive and critical care healthcare professionals. The main limitation is the small sample size, both in terms of quantitative and qualitative data collection. As for the questionnaires used, although both show high reliability, only the EPQ has been validated in Spanish, while the TeamSTEPPS® 2.0 TPOT is in the process of being validated in our language, despite the original version having been translated and back-translated. Future studies in intensive and critical care professionals in our country should increase the sample size to confirm the quantitative results of our study and increase the number of participants in the focus groups to achieve greater saturation of the qualitative data. Likewise, we recommend using the validated Spanish version of TeamSTEPPS® 2.0 TPOT, as well as conducting quasi-experimental pre-post studies (preferably with a control group) or even experimental studies, to which follow-up periods could be added, using the TeamSTEPPS® training programme as an intervention to confirm both the quantitative and qualitative results of our study.
ConclusionsTeamSTEPPS®-based programme training through teaching methodology of clinical simulation improves teamwork and good simulation practices in intensive and critical care professionals.
The TeamSTEPPS® methodology can be a good interprofessional education strategy for the improvement of teamwork communication in intensive and critical care professionals, both at the care level (through in situ simulation strategies) and at the teaching level (through its inclusion in the curriculum of students).
FundingThis project did not receive any type of funding.
Conflict of interestsThe authors have no conflict of interests to declare.
To the company Laerdal España for providing us with the high-fidelity manikin to carry out the simulation sessions in the classroom sessions of the course.