Most patients admitted to intensive care units have alterations in their usual state of consciousness, with the family or relatives serving as substitutes. It is important to determine the knowledge, as well as the attitudes adopted by patients and their representatives as regards the decision-making process at the end of life.
ObjetivesTo determine and examine the knowledge and attitudes of critically ill patients and their families about advance directives and know how family involvement in decision making at the end of life.
MethodA review was conducted using 9 integrated databases with a combination DeCs and MeSH, limiting the search to 11 years. Relevant documents that dealt with knowledge and attitudes of critically ill patients and their families about advance directives and the decision-making process were selected. Critical reading was performed using CASPE lists.
ResultsTwenty articles were selected, of which 8 were descriptive studies, 5 analytical, and 7 were studies performed using qualitative methodology. In these articles, it was found that both the knowledge and the rate of signing of advance directives (AD) are low, and that the decisions of the family is a stress factor that is alleviated by the existence of AD, as well as communication between health professionals and family.
ConclusionsAD are poorly understood by both patients and their relatives, although both showed interest in learning about this tool that can help in decision-making at the end of life. Health professionals also see the AD, along with good communication, as tools for decision making.
La mayoría de los pacientes ingresados en las Unidades de Cuidados Intensivos presentan alteración de su estado de consciencia habitual siendo sus familiares o allegados los que ejercen como sustitutos. Resulta importante conocer los conocimientos y actitudes que adoptan los pacientes y sus representantes respecto al proceso de toma de decisiones al final de la vida.
ObjetivosExplorar los conocimientos y las actitudes del paciente crítico y sus familiares respecto a las directivas anticipadas y conocer la forma de participación de la familia en la toma de decisiones al final de la vida.
MétodoSe realizó una revisión integrada en nueve bases de datos, con una combinación DeCs y MeSH, limitando la búsqueda a once años. La selección se realizó sobre documentos relevantes que trataban de los conocimientos y actitudes del paciente crítico y de sus familiares sobre las directivas anticipadas, así como del proceso de toma de decisiones. La lectura crítica se realizó mediante listas CASPE.
ResultadosSe seleccionaron veinte artículos, de los cuales ocho son estudios descriptivos, cinco son analíticos y siete son estudios realizados con metodología cualitativa. En ellos se encuentra que tanto los conocimientos como el índice de otorgamientos de las directivas anticipadas (DA) son bajos y que la toma de decisiones de los familiares resulta un factor estresante que se ve aliviado por la existencia de DA y la comunicación entre profesionales sanitarios y familiares.
ConclusionesLas DA son poco conocidas, tanto por los pacientes como por sus familiares, aunque ambos muestran interés por conocer este instrumento que puede ayudar en la toma de decisiones al final de la vida. Los profesionales sanitarios también ven las DA junto con la comunicación, como buenas herramientas para la toma de decisiones.
Advance directives (ADs) allow a person to previously express their willingness on how to be taken care of their health. Therefore, this will be fulfilled if, in certain clinical situations, they are unable to express their will. Many patients admitted to the Intensive Care Unit (ICU) suffer from altered state of consciousness. Therefore, surrogate decisions are frequent. Knowing the will of the patient facilitates decision-making at the end of life to both family members and health professionals.
The conclusions of this study lead us to point out that ADs are very helpful in respecting the autonomy of the critically ill patient, but they are not sufficient, especially when complex decisions have to be made, such as those in the ICU.
Implications of the studyIt is evident that the existence of ADs improves decision making by surrogates in the field of critical care. ADs include patients’ preferences. Therefore, the decision burden decreases and trust of patients, representatives and health care teams improves. Studies like this are aimed at promoting visibility and knowledge about ADs.
Critically ill patient decision-making has become very important in our society. On the one hand, the advances of medicine and other related sciences always allow to prolong life to limits unsuspected a few years ago. Life-support techniques can significantly delay the dying process.1 Also, the implementation of the value of personal autonomy has markedly altered the clinical relationship, which must now be adapted to the individuality of the patient. Thus, respect for the principle of autonomy must be maintained during the disease and until the death process.2
Advance directives (ADs), prior instructions are defined as the will that a person reports in advance about their health care and treatment or use/destination of their body, so that that will is fulfilled if certain clinical situations prevent them from expressing their will personally.3
Before proceeding further, it should be noted that in this work the reference to ‘advance directives’ also includes the terms ‘previous instructions’ and ‘living will’. The semantic diversity is due to the fact that the Spanish legislation uses the last two terms.
When patients are referred to an Intensive Care Unit (ICU) their family relationships are interrupted, causing emotional and communication deficiency both in patients and relatives, leading to a situation of crisis.4 ICUs are units where problems around decision-making often arise.
Several authors have studied the needs of relatives of patients admitted to the ICU by grouping them into five areas: information, safety, proximity, support and well-being.5 Information and safety ensure the family that the patient will be well cared for and that, if necessary, will have a dignified death process.6 Therefore, understanding the patient's wishes is particularly relevant. Ensuring that the patient's preferences are respected is very important, especially when many of the patients are in an incapacity situation and therefore they are at a higher risk of autonomy violation.7
In the United States and several countries of the European Union, including Spain, the document of previous instructions includes the option of appointing a representative to be the spokesperson dealing with the health team and seek compliance with the instructions stated by the grantor.3
In critical situations where patients are shown to be unable to make decisions, it is their relatives or next of kins who are appointed as their surrogates. That is why in ICUs it is particularly important to know the current state of the problems that arise in the decision-making process, more specifically the knowledge that patients and relatives have about previous instructions and how the family's participation is performed In this decision making.
Therefore, the objectives of this review are to explore the knowledge and attitudes of the critically ill patients and their family members regarding the previous instructions and to know how the family participates in the decision making at the end of life.
MethodIn order to determine the current understanding about the attitudes of critically ill patients and their relatives regarding previous instructions and decision-making at the end of life, integrative literature review is performed. This type of review allows the search, critical evaluation and synthesis of available evidence.8
The research question is: What knowledge and attitudes do the patients admitted to the ICU and their families have about advance directives? And, how do family members or surrogates make decisions at the end of life? For responding to these issues the phases below are followed:
- 1.
Establishing the study inclusion and exclusion criteria. Participants: patients admitted to the ICU and their relatives or surrogates. Interventions: knowledge and attitudes of critically ill patients and their relatives about advance directives and decision making by relatives or surrogates. The review will include quantitative and qualitative methodology studies.
- 2.
The search strategy. The search will be performed in the following databases: MEDLINE-PUBMED (U.S. National Library of Medicine), LILACS (Latin-American and Caribean Health Science Literature), EMBASE (Excerpta Medica Database), Bibliotheca Cochrane Plus, Science-Direct, IME (Spanish medical index) MEDES (Medicine in Spanish) and CUIDEN (Nursing Index Foundation). A secondary search of gray literature was also carried out in the Open Gray and TESEO databases. For obtaining the full texts, we used the catalog of electronic journals from the Prince of Asturias University Hospital Library in Alcalá de Henares (Madrid) and the Alcalá University Library.
The search time period was 11 years. The search has been performed in Spanish and English. The keywords were identified through the Medical Subject Headings (MeSH) descriptors and Health Sciences Descriptors (HSDe). The keywords used to perform the search were: advance directives, living will, critical patient, critical care, end-of-life care, family, surrogates and decision making.
- 3.
Reading and analyzing the abstracts of the studies found. The article abstracts must contain at least two of the indicated keywords.
- 4.
Selection of studies according to the inclusion criteria.
- 5.
Reading and critical evaluation of the methodology quality of the selected studies through the critical evaluation tool suggested by the Critical Appraisal Skills Program (CASPe)9 and the Critical Appraisal and Evaluation Tool for Cross-Sectional Epidemiological Studies of Berra.10 The Grading of Recommendations Assessment and Evaluation (GRADE) system has been used to evaluate the quality of evidence.11
- 6.
Interpreting results and synthesis by categories.
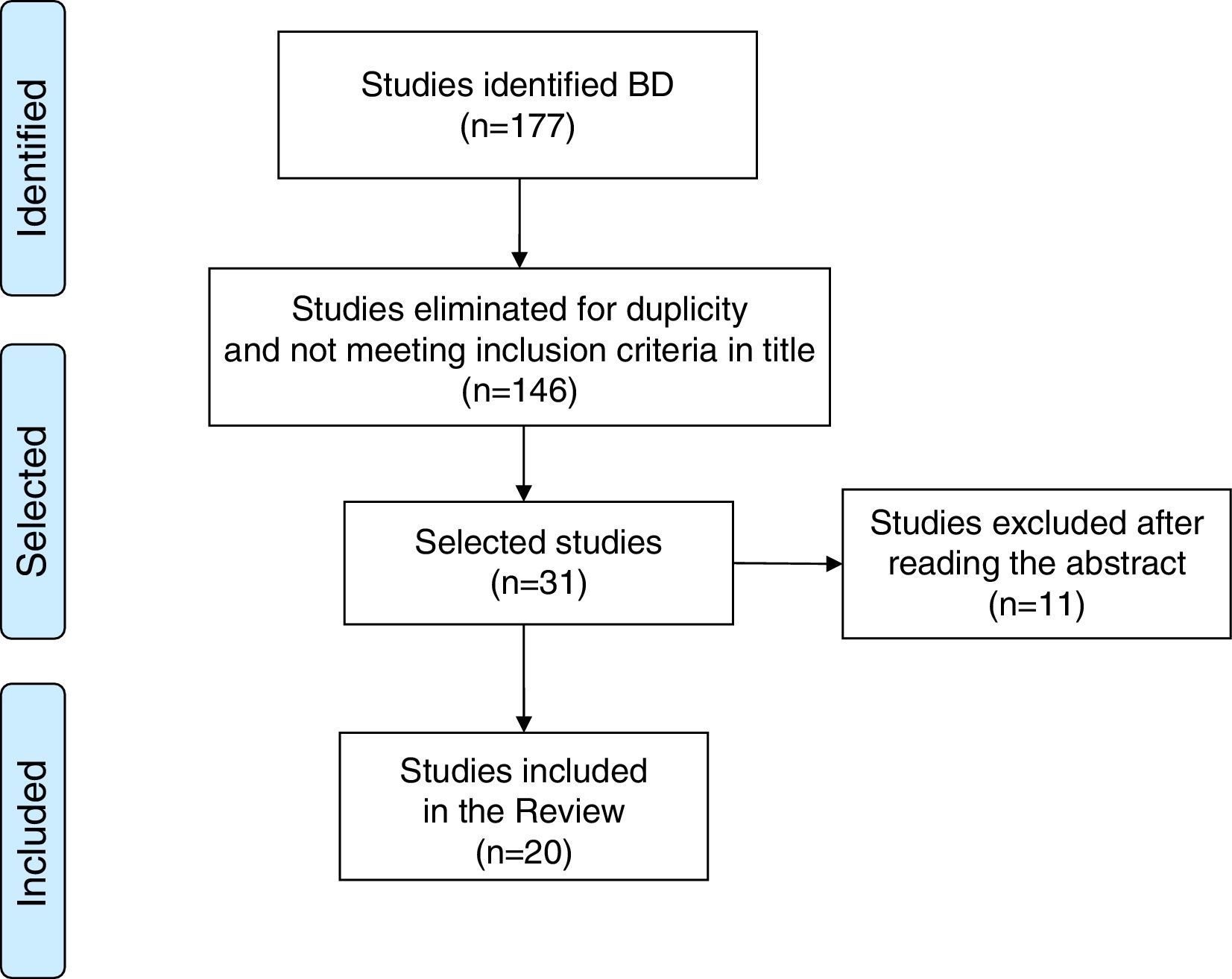
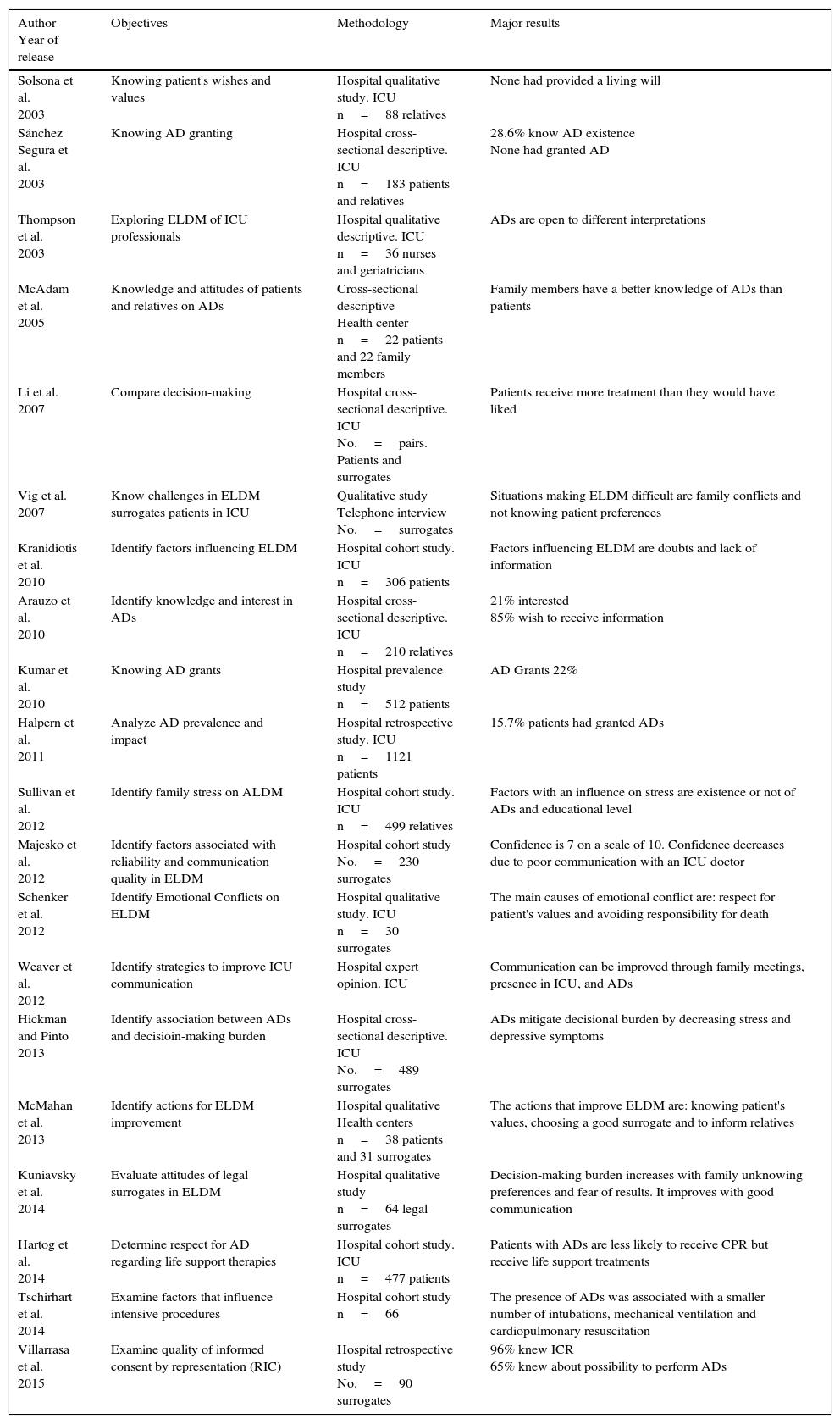
In the first search 177 articles were obtained from the 31 met the inclusion criteria. After reading the original articles, the final selection was limited to 20 articles (Fig. 1).12 Five of the articles found are cohort studies with a moderate-low quality of evidence, 8 are descriptive studies with low evidence quality, and 7 use qualitative methodology resisting the hierarchy of the traditional levels of evidence.13 Consistent with the objective results of the study, the selected articles are divided into two categories: advance directives (8 studies) and family participation in decision-making at the end of life (12 studies). The articles are reported in chronological order in Table 1.
Description of articles reviewed.
| Author Year of release | Objectives | Methodology | Major results |
|---|---|---|---|
| Solsona et al. 2003 | Knowing patient's wishes and values | Hospital qualitative study. ICU n=88 relatives | None had provided a living will |
| Sánchez Segura et al. 2003 | Knowing AD granting | Hospital cross-sectional descriptive. ICU n=183 patients and relatives | 28.6% know AD existence None had granted AD |
| Thompson et al. 2003 | Exploring ELDM of ICU professionals | Hospital qualitative descriptive. ICU n=36 nurses and geriatricians | ADs are open to different interpretations |
| McAdam et al. 2005 | Knowledge and attitudes of patients and relatives on ADs | Cross-sectional descriptive Health center n=22 patients and 22 family members | Family members have a better knowledge of ADs than patients |
| Li et al. 2007 | Compare decision-making | Hospital cross-sectional descriptive. ICU No.=pairs. Patients and surrogates | Patients receive more treatment than they would have liked |
| Vig et al. 2007 | Know challenges in ELDM surrogates patients in ICU | Qualitative study Telephone interview No.=surrogates | Situations making ELDM difficult are family conflicts and not knowing patient preferences |
| Kranidiotis et al. 2010 | Identify factors influencing ELDM | Hospital cohort study. ICU n=306 patients | Factors influencing ELDM are doubts and lack of information |
| Arauzo et al. 2010 | Identify knowledge and interest in ADs | Hospital cross-sectional descriptive. ICU n=210 relatives | 21% interested 85% wish to receive information |
| Kumar et al. 2010 | Knowing AD grants | Hospital prevalence study n=512 patients | AD Grants 22% |
| Halpern et al. 2011 | Analyze AD prevalence and impact | Hospital retrospective study. ICU n=1121 patients | 15.7% patients had granted ADs |
| Sullivan et al. 2012 | Identify family stress on ALDM | Hospital cohort study. ICU n=499 relatives | Factors with an influence on stress are existence or not of ADs and educational level |
| Majesko et al. 2012 | Identify factors associated with reliability and communication quality in ELDM | Hospital cohort study No.=230 surrogates | Confidence is 7 on a scale of 10. Confidence decreases due to poor communication with an ICU doctor |
| Schenker et al. 2012 | Identify Emotional Conflicts on ELDM | Hospital qualitative study. ICU n=30 surrogates | The main causes of emotional conflict are: respect for patient's values and avoiding responsibility for death |
| Weaver et al. 2012 | Identify strategies to improve ICU communication | Hospital expert opinion. ICU | Communication can be improved through family meetings, presence in ICU, and ADs |
| Hickman and Pinto 2013 | Identify association between ADs and decisioin-making burden | Hospital cross-sectional descriptive. ICU No.=489 surrogates | ADs mitigate decisional burden by decreasing stress and depressive symptoms |
| McMahan et al. 2013 | Identify actions for ELDM improvement | Hospital qualitative Health centers n=38 patients and 31 surrogates | The actions that improve ELDM are: knowing patient's values, choosing a good surrogate and to inform relatives |
| Kuniavsky et al. 2014 | Evaluate attitudes of legal surrogates in ELDM | Hospital qualitative study n=64 legal surrogates | Decision-making burden increases with family unknowing preferences and fear of results. It improves with good communication |
| Hartog et al. 2014 | Determine respect for AD regarding life support therapies | Hospital cohort study. ICU n=477 patients | Patients with ADs are less likely to receive CPR but receive life support treatments |
| Tschirhart et al. 2014 | Examine factors that influence intensive procedures | Hospital cohort study n=66 | The presence of ADs was associated with a smaller number of intubations, mechanical ventilation and cardiopulmonary resuscitation |
| Villarrasa et al. 2015 | Examine quality of informed consent by representation (RIC) | Hospital retrospective study No.=90 surrogates | 96% knew ICR 65% knew about possibility to perform ADs |
ICR: informed consent to representation; AD: advance directives; CPR: cardiopulmonary resuscitation; ELDM: end of life decision-making; ICU: Intensive Care Unit; AD: advance directives.
One of the first studies on decision-making at the end of life and attitude toward the death of the critical patient was conducted in 2000 by Solsona et al.1 who carried out 88 interviews to first-degree relatives of patients admitted to an ICU in Barcelona. Family members were asked about the patient's preparation for death, more specifically about the granting of IP by their relative. As a result, none of the 88 patients admitted had provided this grant, although the youngest had appointed a surrogate.
With a similar methodology, from 2002 to 2003 Sánchez et al.14 with the purpose of identifying their knowledge about the advance directives, they interviewed 183 relatives of patients admitted to the ICU. Fewer than half of those interviewed knew the existence of advance directives, and only 30% had heard of them. At the time of this study no patient had provided any advance directives.
In 2005 McAdam et al.15 conducted a study regarding the knowledge and attitudes of patients and relatives to ADs, Noting that ADs were poorly used. Only 2 of 22 patients had ADs, and only 27.3% of the relatives knew it. Relatives had a better knowledge compared to patients. Family members with a higher educational level had a more positive attitude toward ADs.
In the same line, but in Spain, Arauzo et al.16 conducted a survey of 210 family members of patients admitted to an ICU intended to identify the degree of their knowledge on the advance directives. Most of the family members surveyed considered it very interesting and were grateful to receive information about the advance directive document, since many of them were unaware of its existence. In addition, they considered that having a family member in an ICU invited reflection and that the granting of will might be very useful to respect the patient's preferences.
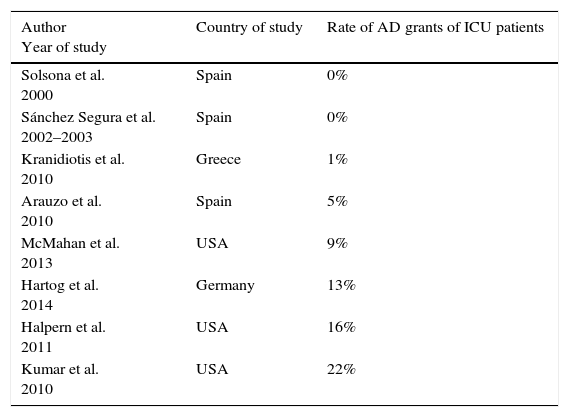
In the study by Halpern et al.17 in 1121 patients admitted to the oncology ICU, 15.7% had performed a living will and 47.6% had granted health care proxy. Similar results are reported in the Kumar et al.18 study conducted in 512 patients admitted to a cardiology ICU. The AD grants were 22%. Vital wills were 5%, granting a surrogate reached 35%. In Table 2 it can be seen that the grant rates in USA are somewhat higher than in the European countries studied.
Rate of advance directive grants in ICU patients.
| Author Year of study | Country of study | Rate of AD grants of ICU patients |
|---|---|---|
| Solsona et al. 2000 | Spain | 0% |
| Sánchez Segura et al. 2002–2003 | Spain | 0% |
| Kranidiotis et al. 2010 | Greece | 1% |
| Arauzo et al. 2010 | Spain | 5% |
| McMahan et al. 2013 | USA | 9% |
| Hartog et al. 2014 | Germany | 13% |
| Halpern et al. 2011 | USA | 16% |
| Kumar et al. 2010 | USA | 22% |
AD: advance directives; ICU: Intensive Care Unit.
Regarding respect for treatment preferences contained in the ADs such as non-resuscitation requests and limited therapeutic effort, Hartog et al.19 concluded that all AD patients were less likely to receive cardiopulmonary resuscitation, but otherwise they received the same life support treatments as patients without advance directives. In another study it is shown that ADs are associated with a lower number of intubations and mechanical ventilation, as well as lower number of cardiopulmonary resuscitations.20
Family participating on decision-makingThompson et al.21 in their study on qualitative design among health professionals, point out the need for the critical patient's family to participate in decision-making. The results show that health care providers see ADs as a good tool for legal protection when their decisions can go against their family's wishes.
Those who had been appointed as surrogates in the decision-making of their family members identified two important facilitating factors in decision-making, such as the existence of ADs and having had previous conversations with the patient about the end of life. On the other hand, the situations that were most difficult for surrogate's decision-making were the existence of a family conflict, the inability to understand the patient's preferences and the physical distance between the patients and their surrogates. The decisions that reduced patient suffering were the easiest to make by their surrogate. Sullivan et al.23 detected higher levels of stress in families with lower educational level. Referring to eight ICUs from different Greek hospitals, Kranidiotis et al.24 studied families of 306 patients, participating in decision-making. Participation occurred in 20% of the cases and was more frequent when it came to deciding the possibility of subjecting the patient to life support techniques. Participation included discussions with physicians about the measures to be taken regarding patient treatment. The reasons why the family members did not participate in decision making were: the family was not sure about the decision to make (60%), relatives were not available to talk to them (25%), family consultation was considered unnecessary by the doctor (10%) and the family did not want to participate in the decision making (4%).
In critical situations where patients have lost the ability to decide and there are no ADs, relatives and next of kin should act as surrogates of the patient. However, various studies point out the existence of discrepancies between patients’ decisions and those their representatives made for them.25
Majesko et al.26 conducted a prospective study to determine whether or not ADs and end-of-life preference discussions facilitate decision-making in the families of ICU patients. The authors concluded that family members with no previous experience as surrogates and those who had not had previous conversations with the patient about their preferences were less confident in deciding the best therapeutic approach for the patient. It was also associated that an increased communication between physician and family causes best confidence in the family members appointed as surrogates and best collaboration in participating in a limited therapeutic effort. As Schenker et al.27 point out, in order to find the personal and emotional reconciliation of the family with the requirements and wishes of loved ones, family should be provided with coping strategies to reduce the interpersonal stresses occurring during the decision-making at the end of life. Recently Hickman and Pinto28 have analyzed psychological aspects of stress and depressive symptoms that involve the decision-making of family members and caregivers of critical patients, finding that the presence of ADs helps to mitigate stress in decision-making. Thus, the health team should try to relieve the burden of decision making, specifically by improving communication with families, with an emphasis on education and the importance of providing ADs.29 McMahan et al.30 have pointed out that ADs are not enough to prepare patients and their surrogates for complex medical decisions at the end of life. ADs are very helpful, but the representative must be properly prepared. In their qualitative study, they identified four important categories regarding family preparation in decision making: (1) identifying patient's values and preferences, (2) choosing the right surrogate, and verifying that they understand their role, (3) deciding freedom of action granted to the surrogate, (4) keep other family members informed about the patient's preferences regarding the care they want to receive. This extended information can prevent from any conflicts. Weaver et al.31 in their study come to similar conclusions regarding support for the family being crucial. This support includes communication as a significant part that can be improved with meetings with the family and the participation of the family in the care of the patient.
A recent study by Villarrasa-Clemente et al.32 on consent for representation in ICU shows that the representatives assumed their acts, preferring not to delegate the decision making in another person or in the existence of ADs, stating in almost all cases, that the decision made agreed with that of their representative.
DiscussionThe bibliographical review carried out shows that the knowledge of critical patients and their relatives about ADs is generally low, even though the legislation on advance directives has been in force for years. Lack of knowledge by patients and family members may be an important cause of the low rate of AD grants that exist in most countries where the studies have been conducted. The low grant rate in patients admitted to the ICUI1,19–24 agrees with studies conducted in other health areas that also have a low number of grants.33–35 In addition the occurrence of serious diseases seems to be a factor discouraging the granting of previous instructions.36,37 The rate of ADs in the adult population in the United States38 ranges from 18 to 36%. However, the number of critical patients with ADs range from 5 to 11%. In patients with hematological cancers the number of grants is 32% despite the possibility of admission to ICU.39
Despite the low development of ADs, the attitudes of critical patients and their relatives toward these documents are favorable. Relatives are receptive to receiving information on ADs and are very interested in this document after information is provided on the subject.1,15 This is in line with the results reported by other studies in primary care, in which over half of the users surveyed showed a high probability of granting previous instructions in the near future, with a high preference for their family members to grant as well.40
Health professionals should take into account this predisposition of relatives and patients to receive information, playing a supportive and guiding role in decision-making,1,14 particularly when physicians and nurses are also favorable to have their patients plan their decisions at the end of life.40–42 In this sense, despite the previously reported failure of the SUPPORT study, different studies have shown that information on AD increases the number of grants.43,44
It seems clear that ADs facilitate decision-making at the end of life because they reduce the decision-making burden on family members and health professionals, both in critically ill areas and in other health areas.35,36
In patients with prolonged periods in the ICU, conflicts may arise within the health team, the patient's relatives, or among each other, the latter being the most frequent, approximately 10%.45,46 In these situations, ADs can facilitate the resolution of the problem. Therefore, some authors have pointed out that they can be used as legal protection for health professionals in actions against the wishes of relatives, if it is considered that these do not act on behalf of the patient.21,45 Nebot et al.47 report that 81% physicians from intensive care and emergency department are aware of the existence of previous instructions in the medical records, but only 5.9% state to have the habit of consulting these records. Most professionals do not verify if the critically ill patients have provided previous instructions and when they know it is because the family has reported it. It is important for the health professionals involved to modify these attitudes to meet the preferences expressed by the patient in the AD document. It should also be noted that family members are not always aware of the patient's preferences and they can make decisions against the best interest of the patient. Some studies have shown that the opinion of the family members is not a reflection of the patient's wishes. In a systemic review Shalowitz et al.48 point out that the degree of concordance between the patient's decision and that of their relatives was 68%.25,39,45 ADs are very helpful in decision-making under the criterion of substituted judgment, but they are not sufficient when complex decisions have to be made. Thus, patients and families need to be trained and educated in decision-making.15
What has been said so far contrasts with what was stated by the representatives of the study by Villarrasa et al. most of these representatives stated that they did not need the ADs to know the preferences of the patient and all stated that their decision had agreed with that of the patient.32
Preparing for the decision making should start by improving the communication between the healthcare team, the patients and their relatives. Since 2004, it has been agreed among US professional associations that a shared approach in decision-making between doctors and family members is best. In this decision-making model, physicians and nurses work with patients and their families to determine the patient's values and preferences regarding their health care.45 Health professionals recommend the patient and their family in the decision-making process, having as main reference the principles of autonomy and beneficence.
Thus, the advance planning of decisions is very interesting, which is a voluntary process of reporting and discussing between a capable person and the health professionals involved in their care.49 Therefore, these professionals can know the patients’ values and plan the care they want to receive. In this planning the health professionals, the patient and their relatives would participate if the patient wants them to. In the United States interesting experiences have been developed on this issue, such as Respecting Choices, which represented an important increase in granting ADs.50 The best time to carry out this planning would be after the diagnosis of a progressive health problem and before this condition becomes critical.32 The nurse should play an important role in the development of early decision planningboth in day-to-day care practice and in special situations, providingsupport to people in decision making about future treatments, care and, particularly, on the treatments related to the artificial maintenance of life. From her advocacy role, the nurse can help draft the AD documents, and will respect, and make be respected, the patients’ preferences.51
The limitations of this study include the heterogeneity of the studies found and a low level of scientific evidence, since a large part of them were observational studies, and another part of the studies presented a qualitative design. Therefore, results cannot be generalized without due precautions.
The reviewed studies help generate hypotheses for future research in fields that need further study, such as the study of the reasons why the number of grants do not increase in the area of critical care and the analysis of the effectiveness of the interventions promoting ADs.
ConclusionsRegarding the knowledge and attitudes of patients and relatives to ADs, the results of the literature review show that ADs are poorly understood by the critical patient and their relatives. However, an important number of patients and families consider their knowledge interesting and identify them as a facilitator of decision making, as it mitigates the decision burden and reduces the stress in these situations.
Health professionals also see ADs as a good tool for decision making at the end of life. Respect for the preferences of the patient by the professionals increases with the existence of ADs.
The factors facilitating the participation of the family in decision making are the existence of conversations between relatives and patients and the existence of good communication between surrogates and the health team assisting the patient. On the contrary, the doubts and lack of information about the preferences of the patient are negative factors.
Conflict of interestsThe authors declare that they have no conflict of interest.
Please cite this article as: Toro-Flores R, López-González R, López-Muñoz JA. Conocimientos y actitudes de los pacientes críticos y sus familiares respecto a las directivas anticipadas y la toma de decisiones al final de la vida. Enferm Intensiva. 2017;28:21–30.