Limitation of life-sustaining treatment is increasingly common in critical care units, and controlled donation after circulatory death is starting to be included as an option within patient care plans. Lack of knowledge and misunderstandings can place a barrier between healthcare professionals.
ObjectiveTo determine the perceptions, knowledge and attitudes of physicians and nurses working in intensive care units regarding Limitation of life-sustaining treatment and controlled donation after circulatory death.
Design, settings and participantsCross-sectional study carried out in 13 Spanish hospitals by means of an ad hoc questionnaire.
MethodsContingency tables, Pearson's chi-squared test, Student's t-test and the Mann–Whitney U-test were used to carry out descriptive, bivariate and multivariate statistical analyses of responses.
ResultsAlthough limitation of life-sustaining treatment is a widespread practice, the survey revealed that nurses feel excluded from the development of protocols and the decision-making process, whilst the perception of physicians is that they have greater knowledge of the topic, and decisions are reached in consensus.
ConclusionsMulti-disciplinary training programs can help critical healthcare providers to work together with greater coordination, thus benefitting patients and their next of kin by providing excellent end-of-life care.
La limitación del tratamiento de soporte vital es cada vez más frecuente en las unidades de críticos, y la donación en asistolia controlada se está empezando a incluir como una opción dentro del plan de cuidados de los pacientes. La falta de conocimientos y los malos entendidos pueden suponer una barrera entre los profesionales sanitarios.
ObjetivoDeterminar la percepción, conocimientos y actitud de los médicos y enfermeras que trabajan en las unidades de críticos sobre la limitación del tratamiento de soporte vital y donación en asistolia controlada.
Diseño, ajustes y participantesSe llevó a cabo un estudio transversal en 13 hospitales españoles utilizando un cuestionario diseñado a tal efecto.
MétodosPara analizar las respuestas se utilizaron tablas de contingencia, el test de Chi cuadrado de Pearson, la «t» de Student y el test de Mann-Whitney para el análisis estadístico descriptivo bivariante y multivariante.
ResultadosAunque la limitación del tratamiento de soporte vital es una práctica muy extendida, el trabajo muestra cómo los enfermeros se sienten excluidos tanto del desarrollo de protocolos como de los procesos de decisión, mientras que la percepción de los médicos es que tienen mayores conocimientos y que las decisiones se toman conjuntamente.
ConclusionesPara solventar estas diferencias, los programas formativos multidisciplinares pueden ayudar a los profesionales de la salud a trabajar conjuntamente, con mayor coordinación, beneficiando tanto a pacientes como a sus familias, y proporcionando cuidados de calidad al final de la vida.
LLST practices are perceived differently by critical healthcare providers, whose respective roles and participation seem to lack definition. This can lead to workplace conflicts that may affect quality of care and next-of-kin perception of confidence in the process.
What is the contribution of this?This is the first multi-center survey on LLST and DCD carried out in a self-governing region of Spain. It reveals differences in perception between nurses and physicians, particularly with regard to the application of LLST and DCD. Multi-disciplinary training programs are the key to providing knowledge, avoiding misunderstandings and promoting teamwork among critical care nurses and physicians in order to provide high quality end-of-life care.
Implications of the studyThe study has found a lack of symmetry between health care professionals regarding knowledge of the legal, clinical and ethical aspects of LLST and of DCD when relevant. Nurses, although willing to increase their knowledge, receive insufficient training in these aspects and feel excluded from the process. Physicians, although better trained, fail to properly contextualize nurses’ role in the process. It is therefore necessary to find common ground between the two in order to provide higher standards of end of life care for patients and the next of kin.
Multidisciplinary training involving both categories will help to harmonize attitudes, as will the creation of common protocols clearly reflecting their respective roles.
Changing attitudes amongst healthcare professionals, moving away from a paternalistic standpoint and toward greater respect for patient autonomy, have led to limitation of life-sustaining treatment (LLST) being seen as an increasingly common option in end-of-life care when treatment has proved futile and care is no longer oriented toward recovery but to making patients as comfortable as possible and allowing them to die with dignity.
Decisions regarding LLST should be reached by consensus between all the healthcare professionals responsible for carrying out the procedure.1–3 However, nursing personnel are not always included in this decision-making process. This can lead to conflict between Intensive Care Unit (ICU) staff involved in end-of-life care, which can be considered “serious” in up to 53% of cases.4 A number of published studies describe the differences in perception between nursing and medical personnel regarding LLST and the problems that can ensue as a result.5
This is even more prominent if LLST procedures are followed by the option of controlled donation after circulatory death, traditionally referred to as Maastricht Category III (donation after circulatory death DCD,) a situation that can give rise to legal, ethical and moral dilemmas amongst healthcare professionals, encouraging conflict.
One of the biggest hurdles to overcome is the lack of knowledge regarding the procedure, which can create misperception that in turn lead to negative attitudes and/or unease, even discontent, amongst healthcare providers,6 this being one of the major limitations to the application of protocols of this nature.
In the case of Spain, where the introduction of DCD programs is a recent and clearly expanding phenomenon, knowledge of the attitudes of healthcare providers to controlled asystole is nevertheless hard to come by.7 Considering donation as an integral part of end of life care is clearly included in the recently publish guidelines on donation-oriented intensive care.8
The purpose of this study is therefore, to determine the perceptions, knowledge and attitudes of critical care physicians and nurses regarding LLST and DCD.
MethodsAn online training course was given in 2013 to 143 physicians (MD) and nurses (RN) working in intensive care units of 13 hospitals in Catalonia. The 150 places available were offered to staff working in ICUs strictly on a first come, first served basis assuring heterogeneity. Participants were asked to fulfill a voluntary survey about their perceptions, knowledge and attitude regarding LLST and DCD. A search was made of the literature related to specific course content. No published validated questionnaires were found that met the requirements of the study, either because they did not apply to the appropriate health care professional profile or to the content of the study. For this reason an ad-hoc questionnaire was devised.
This evaluation was performed by means of an ad hoc questionnaire consisting of 29 multiple choice items divided into 3 sections: demographics and questions about perceptions, attitude and knowledge regarding LLST and DCD, respectively.
Statistical analysisInternal consistency of the survey, which was answered by 133 participants who fulfilled the survey (70 MD, 63 RN), was evaluated using Cronbach's alpha. Internal consistency analysis gave a Cronbach's alpha coefficient of 0.736 (a minimum reliability threshold of 0.70 was considered as being adequate.9,10
In order to study the relation between the demographics of the subjects with their attitudes, perceptions and knowledge regarding LLST and DCD, contingency tables, Pearson's chi-squared test, Student's t-test and the Mann–Whitney U-test were used to carry out descriptive and bivariate statistical analyses, assuming a significance level of 0.05 or less. Fisher's exact test was applied to contingency tables when the expected frequency was less than 5. Odds Ratio was calculated when the significance level was reached. Logistic regression models were constructed for every item of attitudes, perceptions and knowledge regarding LLST and DCD to analyze their association to age, sex, prior work experience and demographic characteristics with p<0.2 in bivariate analysis. The software used to perform the analyses was IBM SPSS v21©.
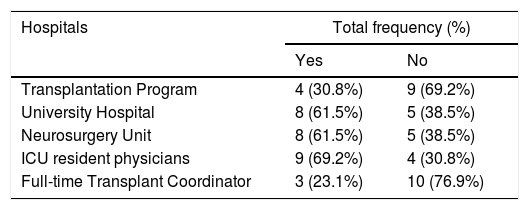
ResultsDemographics133 healthcare providers responded to the survey, giving a response rate of 93% of all those following the training course (n=143). The median number of subjects per hospital was 4, with 73.7% of the total sample coming from non-transplantation hospitals and the remaining 26.6% from hospitals that perform organ transplantation. The characteristics and profile of the hospitals taking part in the survey are shown in Table 1.
Types of hospital taking part in the survey.
| Hospitals | Total frequency (%) | |
|---|---|---|
| Yes | No | |
| Transplantation Program | 4 (30.8%) | 9 (69.2%) |
| University Hospital | 8 (61.5%) | 5 (38.5%) |
| Neurosurgery Unit | 8 (61.5%) | 5 (38.5%) |
| ICU resident physicians | 9 (69.2%) | 4 (30.8%) |
| Full-time Transplant Coordinator | 3 (23.1%) | 10 (76.9%) |
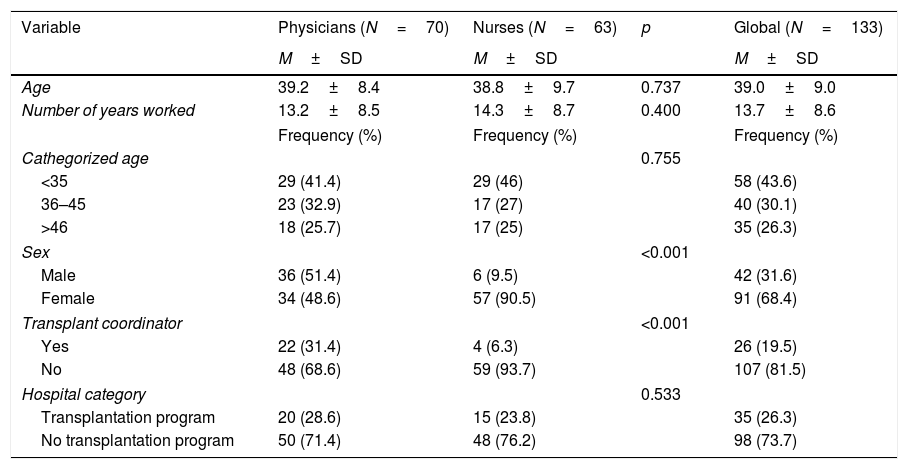
31.6% of respondents were male and 68.4% female, with 52.6% (n=70) being MD and 47.4% (n=63) RN. Demographics are shown in full in Table 2.
Demographic data.
| Variable | Physicians (N=70) | Nurses (N=63) | p | Global (N=133) |
|---|---|---|---|---|
| M±SD | M±SD | M±SD | ||
| Age | 39.2±8.4 | 38.8±9.7 | 0.737 | 39.0±9.0 |
| Number of years worked | 13.2±8.5 | 14.3±8.7 | 0.400 | 13.7±8.6 |
| Frequency (%) | Frequency (%) | Frequency (%) | ||
| Cathegorized age | 0.755 | |||
| <35 | 29 (41.4) | 29 (46) | 58 (43.6) | |
| 36–45 | 23 (32.9) | 17 (27) | 40 (30.1) | |
| >46 | 18 (25.7) | 17 (25) | 35 (26.3) | |
| Sex | <0.001 | |||
| Male | 36 (51.4) | 6 (9.5) | 42 (31.6) | |
| Female | 34 (48.6) | 57 (90.5) | 91 (68.4) | |
| Transplant coordinator | <0.001 | |||
| Yes | 22 (31.4) | 4 (6.3) | 26 (19.5) | |
| No | 48 (68.6) | 59 (93.7) | 107 (81.5) | |
| Hospital category | 0.533 | |||
| Transplantation program | 20 (28.6) | 15 (23.8) | 35 (26.3) | |
| No transplantation program | 50 (71.4) | 48 (76.2) | 98 (73.7) | |
M: mean.
SD: standard deviation.
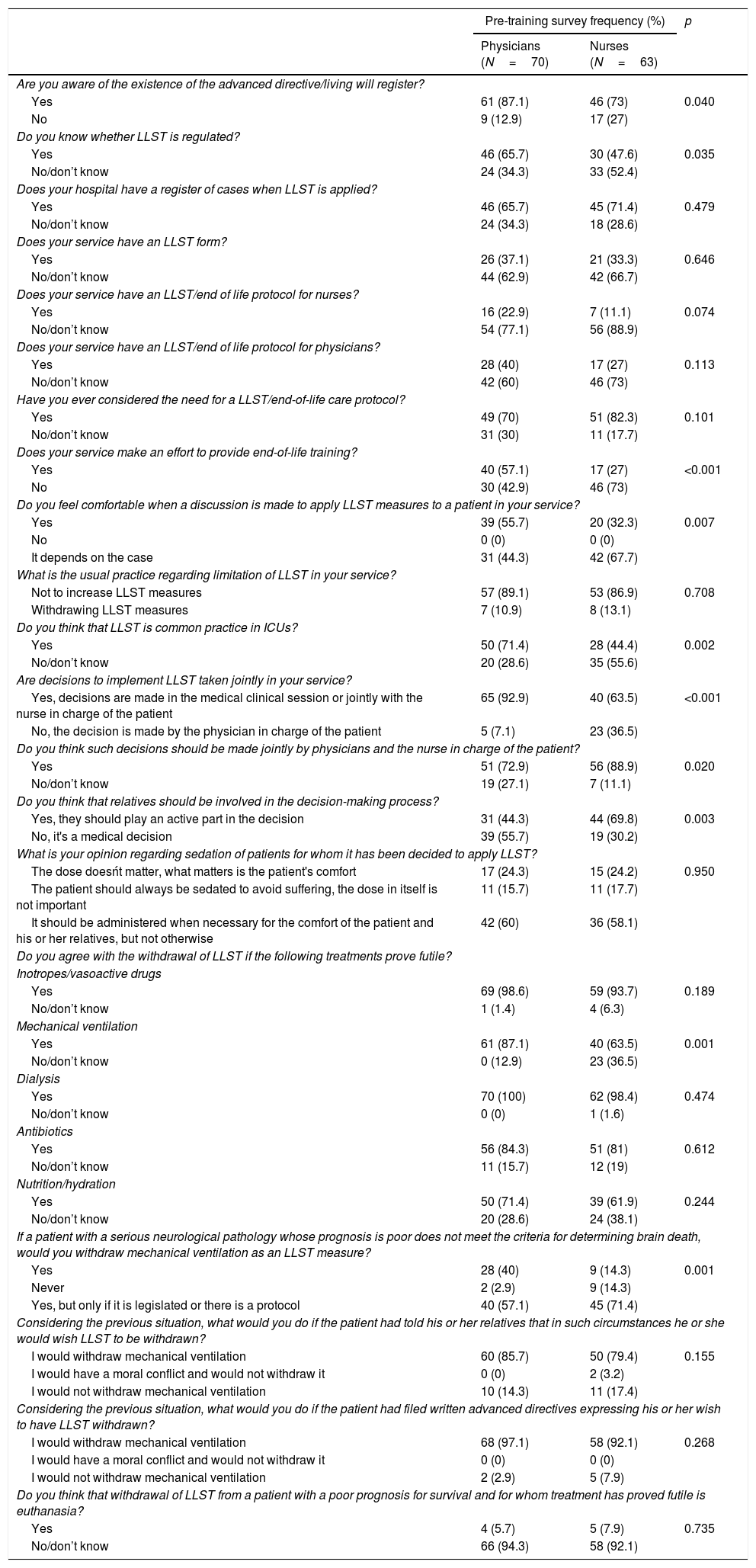
80.5% of respondents said they were aware of the existence of a register of advance directives, representing 87.1% of the MD and 73% of the RN (OR 2.5 (CI 95% 1.02–6.12) p=0.040) who took part in the survey. The results comparing MD and RN are summarized in Table 3
Results of the survey on Limitation of Life-Sustaining Treatment.
| Pre-training survey frequency (%) | p | ||
|---|---|---|---|
| Physicians (N=70) | Nurses (N=63) | ||
| Are you aware of the existence of the advanced directive/living will register? | |||
| Yes | 61 (87.1) | 46 (73) | 0.040 |
| No | 9 (12.9) | 17 (27) | |
| Do you know whether LLST is regulated? | |||
| Yes | 46 (65.7) | 30 (47.6) | 0.035 |
| No/don’t know | 24 (34.3) | 33 (52.4) | |
| Does your hospital have a register of cases when LLST is applied? | |||
| Yes | 46 (65.7) | 45 (71.4) | 0.479 |
| No/don’t know | 24 (34.3) | 18 (28.6) | |
| Does your service have an LLST form? | |||
| Yes | 26 (37.1) | 21 (33.3) | 0.646 |
| No/don’t know | 44 (62.9) | 42 (66.7) | |
| Does your service have an LLST/end of life protocol for nurses? | |||
| Yes | 16 (22.9) | 7 (11.1) | 0.074 |
| No/don’t know | 54 (77.1) | 56 (88.9) | |
| Does your service have an LLST/end of life protocol for physicians? | |||
| Yes | 28 (40) | 17 (27) | 0.113 |
| No/don’t know | 42 (60) | 46 (73) | |
| Have you ever considered the need for a LLST/end-of-life care protocol? | |||
| Yes | 49 (70) | 51 (82.3) | 0.101 |
| No/don’t know | 31 (30) | 11 (17.7) | |
| Does your service make an effort to provide end-of-life training? | |||
| Yes | 40 (57.1) | 17 (27) | <0.001 |
| No | 30 (42.9) | 46 (73) | |
| Do you feel comfortable when a discussion is made to apply LLST measures to a patient in your service? | |||
| Yes | 39 (55.7) | 20 (32.3) | 0.007 |
| No | 0 (0) | 0 (0) | |
| It depends on the case | 31 (44.3) | 42 (67.7) | |
| What is the usual practice regarding limitation of LLST in your service? | |||
| Not to increase LLST measures | 57 (89.1) | 53 (86.9) | 0.708 |
| Withdrawing LLST measures | 7 (10.9) | 8 (13.1) | |
| Do you think that LLST is common practice in ICUs? | |||
| Yes | 50 (71.4) | 28 (44.4) | 0.002 |
| No/don’t know | 20 (28.6) | 35 (55.6) | |
| Are decisions to implement LLST taken jointly in your service? | |||
| Yes, decisions are made in the medical clinical session or jointly with the nurse in charge of the patient | 65 (92.9) | 40 (63.5) | <0.001 |
| No, the decision is made by the physician in charge of the patient | 5 (7.1) | 23 (36.5) | |
| Do you think such decisions should be made jointly by physicians and the nurse in charge of the patient? | |||
| Yes | 51 (72.9) | 56 (88.9) | 0.020 |
| No/don’t know | 19 (27.1) | 7 (11.1) | |
| Do you think that relatives should be involved in the decision-making process? | |||
| Yes, they should play an active part in the decision | 31 (44.3) | 44 (69.8) | 0.003 |
| No, it's a medical decision | 39 (55.7) | 19 (30.2) | |
| What is your opinion regarding sedation of patients for whom it has been decided to apply LLST? | |||
| The dose doesńt matter, what matters is the patient's comfort | 17 (24.3) | 15 (24.2) | 0.950 |
| The patient should always be sedated to avoid suffering, the dose in itself is not important | 11 (15.7) | 11 (17.7) | |
| It should be administered when necessary for the comfort of the patient and his or her relatives, but not otherwise | 42 (60) | 36 (58.1) | |
| Do you agree with the withdrawal of LLST if the following treatments prove futile? | |||
| Inotropes/vasoactive drugs | |||
| Yes | 69 (98.6) | 59 (93.7) | 0.189 |
| No/don’t know | 1 (1.4) | 4 (6.3) | |
| Mechanical ventilation | |||
| Yes | 61 (87.1) | 40 (63.5) | 0.001 |
| No/don’t know | 0 (12.9) | 23 (36.5) | |
| Dialysis | |||
| Yes | 70 (100) | 62 (98.4) | 0.474 |
| No/don’t know | 0 (0) | 1 (1.6) | |
| Antibiotics | |||
| Yes | 56 (84.3) | 51 (81) | 0.612 |
| No/don’t know | 11 (15.7) | 12 (19) | |
| Nutrition/hydration | |||
| Yes | 50 (71.4) | 39 (61.9) | 0.244 |
| No/don’t know | 20 (28.6) | 24 (38.1) | |
| If a patient with a serious neurological pathology whose prognosis is poor does not meet the criteria for determining brain death, would you withdraw mechanical ventilation as an LLST measure? | |||
| Yes | 28 (40) | 9 (14.3) | 0.001 |
| Never | 2 (2.9) | 9 (14.3) | |
| Yes, but only if it is legislated or there is a protocol | 40 (57.1) | 45 (71.4) | |
| Considering the previous situation, what would you do if the patient had told his or her relatives that in such circumstances he or she would wish LLST to be withdrawn? | |||
| I would withdraw mechanical ventilation | 60 (85.7) | 50 (79.4) | 0.155 |
| I would have a moral conflict and would not withdraw it | 0 (0) | 2 (3.2) | |
| I would not withdraw mechanical ventilation | 10 (14.3) | 11 (17.4) | |
| Considering the previous situation, what would you do if the patient had filed written advanced directives expressing his or her wish to have LLST withdrawn? | |||
| I would withdraw mechanical ventilation | 68 (97.1) | 58 (92.1) | 0.268 |
| I would have a moral conflict and would not withdraw it | 0 (0) | 0 (0) | |
| I would not withdraw mechanical ventilation | 2 (2.9) | 5 (7.9) | |
| Do you think that withdrawal of LLST from a patient with a poor prognosis for survival and for whom treatment has proved futile is euthanasia? | |||
| Yes | 4 (5.7) | 5 (7.9) | 0.735 |
| No/don’t know | 66 (94.3) | 58 (92.1) | |
57.1% of the sample were familiar with LLST regulations in Spain, accounting for 65.7% MD and 47.6% RN (OR 2.1 (CI 95% 1.08–4.4) p=0.035).
68.4% of participants acknowledged the existence of some kind of register of LLST practice in their hospital, of whom 50.5% (35.5% of the total) declared that this register consisted of a form specifically designed for this purpose and included in the patient's clinical record.
However, 76.4% of those taking part in the survey, MD (70%) and RN (82.3%) expressed the need to have an end-of-life care and LLST protocol in place (p=0.101). However, for those working in hospitals with no transplantation activity, statistically significant differences were observed between MD (66%) and RN (85.4%) (OR 3 (CI 95% 1.18–8.14) p=0.025).
Only 44.3% of participants said they felt comfortable with the application of LLST, fewer problems being reported in this respect by MD (55.7%) than RN (32.3%) (OR 2.64 (CI 95% 1.29–5.38) p=0.007).
58.6% of subjects said that LLST is frequently carried out in ICUs (71.4% MD vs. 44.4% RN (OR 3.12 (CI 95% 1.52–6.40) p=0.002), the most commonly used procedure, being not to increase life-support measures (withholding) (88%) as opposed to stopping them (withdrawing) (12%). Withholding life-sustaining measures was more frequently used in hospitals with no transplantation program (93.5%) than in those where transplantations are performed (72.7%) (OR 5.37 (CI 95% 1.74–16.60) p=0.004). Multivariate analysis identified working in a hospital with no transplantation activity (p=0.017) as the factor associated with withholding.
88.9% of those taking part in the survey considered that the decision to apply LLST should be taken jointly by the MD(s) and RN(s) responsible for the patient, although the difference in response between the two branches of healthcare providers (physicians 72.9%, nurses 88.9%) were found to be statistically significant (OR 2.92 (CI 95% 1.15–7.67) p=0.020). However, when asked about the situation in their own hospital, the percentage was somewhat lower (78.9%), although once again differences were noted between the two branches of healthcare providers (MD 92.6%, RN 63.5%) (OR 7.47 (CI 95% 2.63– 21.23) p<0.001).
56.4% of respondents said they agreed that relatives should be active participants in the LLST decision-making process, with RN (69.8%) supporting this view to a greater extent than MD (44.3%) (OR 2.91 (CI 95% 1.25–9.4) p=0.003).
58.6% of survey participants (MD 60%, RN 58.1%) were in agreement with limiting the administration of sedatives in a LLST context to those cases in which it was necessary in order to guarantee the comfort of patients and their relatives, thereby avoiding any unnecessary application of this measure, whilst the remaining considered that sedatives should be administered in a pre-emptive manner to all patients to whom LLST procedures are applied.
When asked to state to which life-sustaining measures they thought should be withdrawn after being considered futile, as part of the LLST process, 99.2% of respondents said dialysis, 96. 2% said inotropes, 82.7% said antibiotics, 75.9% mechanical ventilation and 66.9% said nutrition and/or hydration. The only differences between physicians and nurses in this respect involved mechanical ventilation (MV) (MD 87.1% vs. RN 63.5%) (OR 3.89 (CI 95% 1.63–9.28) p=0.001),
The percentage in favor of withdrawing MV increased if patients had previously informed relatives of their wish to have futile treatment discontinued (MD 85.7% vs. RN 79.4%) or had registered their advance directives (MD 97.1% vs. RN 92.1%), respectively.
Only 6.8% of respondents equated application of withdrawing futile life-sustaining treatment from patients with a poor survival to euthanasia, with no differences being found between healthcare provider categories (MD 5.7%, RN 7.9%).
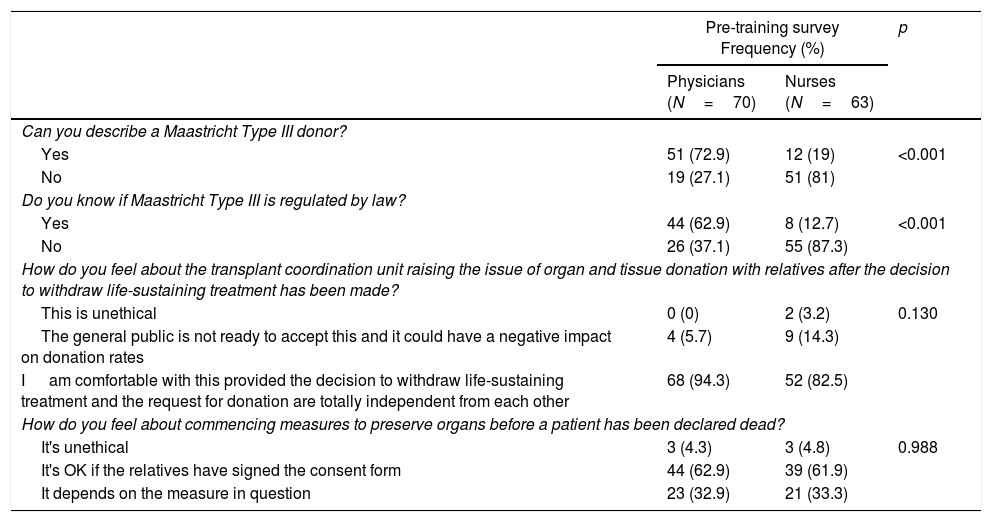
Donation after circulatory death (DCD)The results comparing MD and RN are summarized in Table 4. 47.4% of subjects said they could describe DCD, although there was an extremely high degree of difference in this respect between MD (72.9%) and nurses (19%) (OR 11.40 (CI 95% 5.02–25.91) p<0.001), regardless of the type of hospital they worked in.
Results of the surveys on Donation in Cardiac Death.
| Pre-training survey Frequency (%) | p | ||
|---|---|---|---|
| Physicians (N=70) | Nurses (N=63) | ||
| Can you describe a Maastricht Type III donor? | |||
| Yes | 51 (72.9) | 12 (19) | <0.001 |
| No | 19 (27.1) | 51 (81) | |
| Do you know if Maastricht Type III is regulated by law? | |||
| Yes | 44 (62.9) | 8 (12.7) | <0.001 |
| No | 26 (37.1) | 55 (87.3) | |
| How do you feel about the transplant coordination unit raising the issue of organ and tissue donation with relatives after the decision to withdraw life-sustaining treatment has been made? | |||
| This is unethical | 0 (0) | 2 (3.2) | 0.130 |
| The general public is not ready to accept this and it could have a negative impact on donation rates | 4 (5.7) | 9 (14.3) | |
| I am comfortable with this provided the decision to withdraw life-sustaining treatment and the request for donation are totally independent from each other | 68 (94.3) | 52 (82.5) | |
| How do you feel about commencing measures to preserve organs before a patient has been declared dead? | |||
| It's unethical | 3 (4.3) | 3 (4.8) | 0.988 |
| It's OK if the relatives have signed the consent form | 44 (62.9) | 39 (61.9) | |
| It depends on the measure in question | 23 (32.9) | 21 (33.3) | |
33.3% of participants were aware that DCD is regulated under Spanish law, with MD (62.9%) being better informed than RN (12.7%) (p<0.001, OR 11.63 (CI 95% 4.79–28.22)), regardless of the kind of hospital they worked in.
91% of those taking part in the survey said they agreed that relatives should be approached regarding the possibility of organ and tissue donation after a decision to apply LLST has been reached, provided that there was no overlap between the two processes.
In this regard, 62.9% of respondents agreed with starting organ preservation measures before death is declared above all when relatives had signed a consent form, although for 32.9% the commencement of preservation would depend on the measures applied, the majority being in favor of administering vasodilators (91.9%) or heparin (84.2%) and a smaller number in favor of vascular cannulation (70%), there being no differences between MD and RN.
DiscussionThe aim of this survey is to compare knowledge, attitudes and perception regarding LLST and DCD between physicians and nurses from a number of different hospitals in a large region of Spain.
Previously published studies have analyzed healthcare providers’ perception of DCD on a global level11; that of only nurses,12 or in comparison with the general population.13
Although physicians and nurses are both involved in applying the LLST and DCD measures, there is an obvious difference between their knowledge, attitudes and roles. Although LLST is becoming an increasingly widespread practice in Spain, the findings of this survey reveal that nurses perceive themselves as being overlooked in both the decision-making process and the creation of protocols. The perception of physicians, on the other hand, was that they have greater knowledge of the topic, feel more comfortable with the application of LLST and even work jointly with nurses to make decisions in this regard. It would therefore appear that the two groups of healthcare providers have a different understanding of what deciding by consensus means.
Only one out of three nurses said they feel comfortable when it comes to making a decision to apply LLST, a finding that coincides with those of the study carried out by Gedney et al.,14 revealing that nurses were less satisfied than physicians with the decision-making process.
The findings of our study indicate that 80.5% of participants think that the decision to apply LLST should be taken by physicians and nurses jointly, although a difference was noted between MD (72.9%) and RN (88.9%). Similar results were described by Ferrand et al.,5 this reveals that one of the obstacles in the way of decision-making by consensus is that both professions need to accept that they both have to be part of the process and discuss matters together, a basic premise of any kind of teamwork.
More than half of the respondents thought that the patient's relatives should play an active role in the LLST decision-making process, with nurses being more in favor of this option than physicians (71% vs. 44.3%, respectively). Similar findings were described in the study carried out by Ferrand et al.,5 these findings could be a reflection of the different types of relation that arise between a patient's relatives and the different categories of healthcare provider, since generally speaking nurses develop closer relations with the former as a result of spending more time with them.15
Sedation is one of the pillars of LLST and in overall terms all the healthcare providers surveyed said they agreed that a patient showing signs of distress should be sedated, a figure that is almost identical to that identified by Abizanda et al.,16 who reported that 99% of their sample were in favor of unrestrictedly alleviating a terminally ill patient's distress and anguish. Our study, however, revealed a difference of opinion as to when sedation should be applied, preemptive approach 17 or reactive approach,18 no differences being found between the two professional categories.
Although LLST includes both withdrawal and withholding of life-sustaining treatment, a study of the literature reveals differences in attitude regarding the two. In the study carried out by Abizanda et al.16 agreement with the decision to withhold life-sustaining treatment was less than that to withdraw such treatment as reported in our study, examples being the case of dialysis (76% vs. 99.2%, respectively) or vasopressors (64% vs. 96.2%, respectively), although for other treatments (e.g. mechanical ventilation or nutrition) the percentages are very similar.
Terminal extubation is one of the most conflictive issues in the LLST debate. Our findings show that 75% of respondents are in favor of withdrawing MV if such treatment is considered futile, with physicians (87.1%) being more in favor than nurses (63.5%).
Differences in attitude and perception over the decision to withdraw MV and the extent to which healthcare providers feel comfortable with it are apparent in this study, especially as far as nurses are concerned. Regardless of whether the patient has left advanced directives or whether his or her relatives transmit his wishes, nurses feel less comfortable with such a decision than physicians.
Donation after circulatory deathFirst introduced in Spain in 2012, DCD is currently seen as a complement to donation after brain death and a way to increase the donor pool in the face of ever-growing transplantation waiting lists, a situation that is common to many countries.19
Less than half of the respondents in our survey (47.4%) were familiar with the procedures governing DCD. A possible reason for this is that at the time the survey took place relatively few Spanish hospitals had any experience in this field, only one of which was included in our study.20
This figure increased in the case of nurses, 82.3% of whom said they were unfamiliar with this kind of donation. These results are similar to those reported by Vincent et al.12 referring to Belgium, where in spite of a longstanding tradition of DCD 76% of the nurses who took part in their survey said they thought they were insufficiently informed about donors of this kind and needed more information. Furthermore, 24% of the survey population said they felt uncomfortable with this kind of donation.
In the case of Australia,21 a survey administered to physicians and nurses revealed that only 31.9% of respondents acknowledged that they felt properly informed about the DCD process, as opposed to 47.4% in our survey.
Similarly, in the former study 23.3% of respondents said they were familiar with the law concerning circulatory death versus 39.1% in our survey, findings which reveal the need to make a greater effort to close the knowledge gap in this respect in future training programs.
A further difference between the two studies was that in the former 71% of participants approved of DCD, fewer than the 90.8% of respondents in our study who were in favor of DCD, providing LLST and donation were totally separate processes. They also thought that educational measures needed to be available to healthcare providers so as to prevent misunderstandings and negative attitudes toward donation after circulatory death, with a majority of 61.4% considering that this should be in the form of additional training.
A number of studies have reflected the lack of visibility of the nursing profession in crucial aspects of end-of-life care and the LLST decision-making process.22–24 These authors consider that although nurses are sometimes consulted about a patient's situation by the physician in charge, as are the patient's relatives, nurses are not seen as an essential component of the decision-making process, in spite of the recommendations and guidelines that have been published in the sense1 and the fact that nurses are the healthcare providers who are normally responsible for putting the decision into practice.
The findings of our study clearly reveal the essential need for training amongst critical care providers, especially nurses, in order for them to assume a more visible role in a decision-making process that should involve both professions. The results show that nurses do not feel that their opinion is taken into account when it comes to deciding whether or not to limit life-sustaining treatment, and that when this decision is made, they are reluctant to withdraw MV. This highlights the need to design training programs that will help to reduce the lack of specific knowledge in this area and promote joint consultation and action, the final goal being to improve the quality of the end-of life care being delivered in such situations.
At the same time, physicians would also benefit from receiving training that will allow them to understand the importance not only of the collaborative role played by nurses in the decision-making process but also their position as the first point of contact with patients and their relatives. This would help to ensure that a person's right to donate is protected and guaranteed from both the clinical and ethical point of view by all the healthcare personnel concerned.
ConclusionsThe introduction of training programs that bring physicians and nurses together at the same time would be one way of helping both professions to work together more closely and in better coordination with a view to benefiting patients and their relatives alike by providing excellent levels of care. Similarly, it is impossible to envisage a DCD program in the absence of a good LLST protocol. The latter, however, will not be possible unless there is a meeting of minds between all concerned, nurses as well as physicians, who should necessarily have received sufficient and proper training in both aspects of this end-of-life process.
Conflict of interestsThe authors declare that they have no conflict of interests.
The authors wish to thank Dr. Teresa Seoane Pillado for the statistical support, and Mr. Nick Shaw for his contribution with the English revision. We would also like thank Dr. Jacinto Sánchez-Ibáñez for the unconditional support provided toward the publication of this article.
Please cite this article as: Lomero-Martínez MM, Jiménez-Herrera MF, Bodí-Saera MA, Llauradó-Serra M, Masnou-Burrallo N, Oliver-Juan E, et al. Decisiones en los cuidados al final de la vida. ¿Jugamos en el mismo equipo? Enferm Intensiva. 2018;29:158–167.