This study aims to identify the effects of coaching methods in reducing HbA1c to improve glycemic control.
MethodsThe search for articles in this study was obtained from several databases, namely: PubMed, Cochrane, EBSCO, and Google Scholar. The article criteria were examined in patients with type 2 diabetes mellitus, adult patients (18–60 years), the Randomized Control Trial, a study that measured HbA1c, carried out in the last ten years and reported in English.
ResultsSix studies were selected in this study – those studies showing significant positive results for a decrease in HbA1c after coaching intervention.
ConclusionThe coaching method is promising to improve glycemic control in patients with type 2 diabetes mellitus. It can be seen in the study that face-to-face coaching combined with a telephone, can be recommended.
Diabetes is one of the most common chronic diseases in all countries and continues to increase in significant numbers. The International Diabetes Federation shows that since 2011 people with diabetes continue to increase.1,2 In 2017, people with diabetes increased to 461 million from the previous year in the age range of 18–99 years worldwide and were expected to increase to 693 million in 2045.3 In managing diabetes, self-management coaching is needed in developing skills and confidence for diabetes management, improving health, monitoring symptoms, the impact of the disease, and interpersonal relationships in following medication.4,5 Therefore one effort that can be done is by giving health coaching that has been widely used by individuals and business executives, athletes, and students for career development and changing behavior in social interactions to access the motivation needed to achieve goals, because in the coaching model aims to resolve complex psychosocial factors and lifestyle behaviors that are suitable for managing patients with type 2 diabetes, increasing diabetes control, and increasing adherence to medication.6–8 Thus, coaching can be used as a complementary therapy in diabetes management as an effort to control glycemic. However, limited review regarding the evaluation of coaching in the outcomes of diabetes patients. Therefore, this literature review aims to conduct a recent literature review of RCTs that have evaluated the effectiveness of coaching which is focused on decreasing HbA1c as an indicator of improved glycemic control in patients with type 2 diabetes mellitus.
MethodsPreferred reporting items for systematic review and meta-analysis (PRISMA) were used in this study.9 The selection criteria included in this study are articles with patients (18–70 years), patients who have a history of type 2 diabetes, the randomize control trial, studies that measure the clinical outcome of HbA1c, studies conducted in ten years. In this review, the search was carried out using four databases in the last ten years, namely PubMed, Cochrane, EBSCO, and Google Scholar. Search strategies in several databases use MESH, free titles and terms designed using PICO10 principles, with search keywords consist of (P): diabetes, diabetes mellitus, type 2 diabetes, (I): coaching, health coaching, coaching, (C): none, (O): glycemic control, glycemic management, (T): 3–18 months follow-up.
The number of articles in the database identified as titles and abstracts were 19,174 articles. The process of identifying duplicates from titles/abstracts is 32 duplicate articles and 19,142 articles remaining. Furthermore, screening for the full text was issued 2385 articles and publication years over the past ten years were 7586 articles so that the results obtained were 9171 articles left. Then a more in-depth examination of the full-text article by both authors, where an author determines the selected article and another author validated the article's eligibility based on the inclusion criteria, so as many as six articles are eligible to proceed in this literature review.
In reviewing the article, the Critical Appraisal Skills Program (CASP) tools/guidelines are used. The CASP instrument includes a Randomized Controlled Trial Checklist of 11 questions, including questions of study validity, the validity of the results, and external validity. Steps taken to prevent the risk of bias in a systematic review are carried out by determining data extraction, including the similarity of research in terms of design studies, research objectives, and assessed results.11 Data synthesis was carried out qualitatively by the two authors by discussing and analyzing selected studies. All interventions in the form of coaching methods with various techniques that aim to improve glycemic control in patients with type 2 diabetes mellitus.
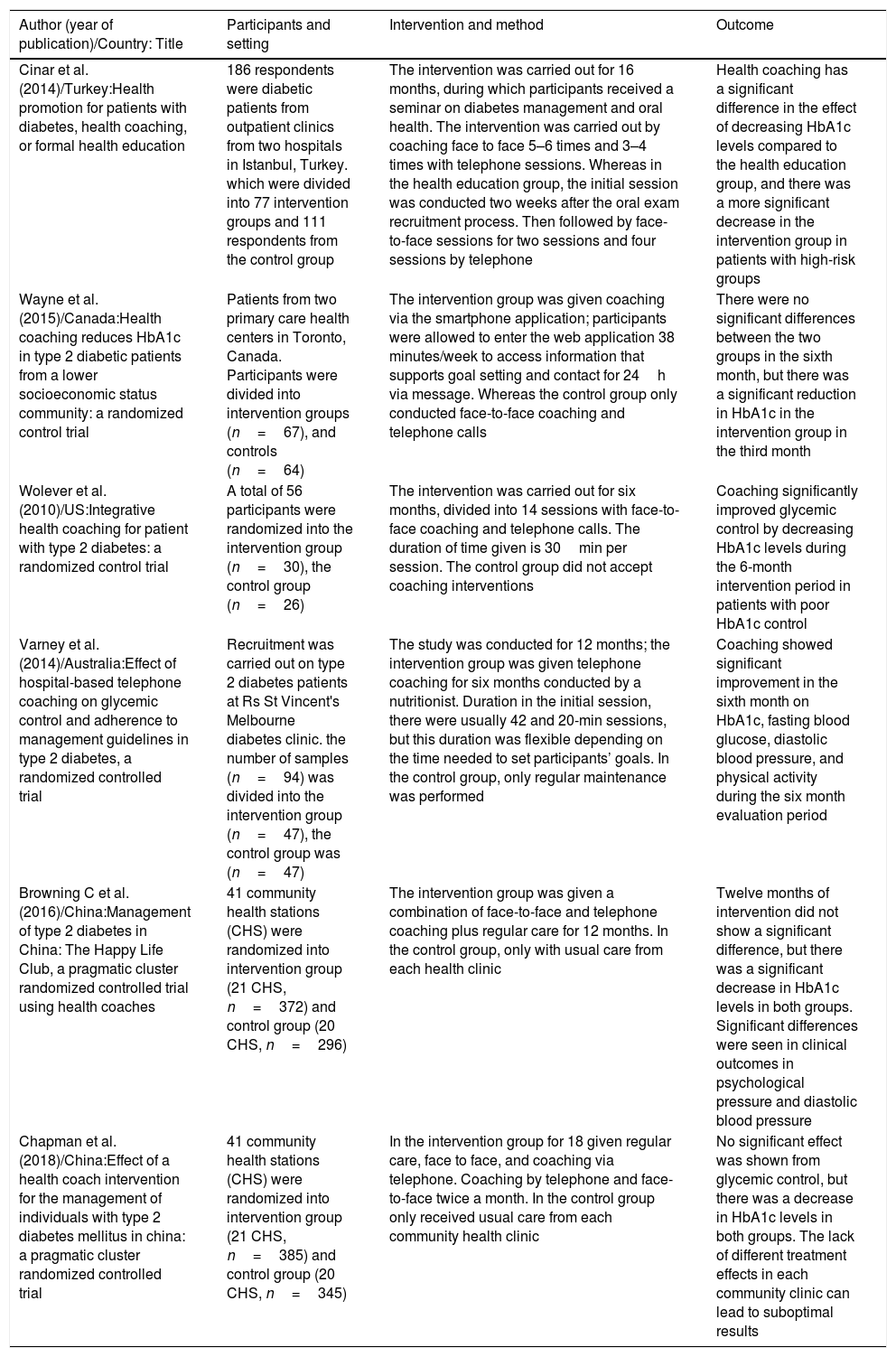
ResultsThe six articles reviewed and summarized in the characteristics associated with coaching interventions in diabetic patients to improve glycemic control as assessed by decreasing HbA1c levels and other clinical results presented in Table 1. The results of the articles included in the literature review show the coaching effect on Clinical improvement results on glycemic control (HbA1c, and other results) in patients with type 2 diabetes mellitus. Based on studies conducted by Wolever et al.6 in the United States found significant results on HbA1c reduction. Fifty-six participants were divided into control groups (usual care) and intervention groups (coaching). Coaching interventions were given for six months face to face and telephone, which were divided into 14 sessions with a duration of 30min in each session. The clinical results of HbA1c levels in the coaching group were significantly reduced by ≥7% (p<0.05), and in the control group, there were no significant changes. Treatment adherence improved (Z=−2.66; p=0.04) in the intervention group, while the control group did not change.
Characteristics and results of included studies.
| Author (year of publication)/Country: Title | Participants and setting | Intervention and method | Outcome |
|---|---|---|---|
| Cinar et al. (2014)/Turkey:Health promotion for patients with diabetes, health coaching, or formal health education | 186 respondents were diabetic patients from outpatient clinics from two hospitals in Istanbul, Turkey. which were divided into 77 intervention groups and 111 respondents from the control group | The intervention was carried out for 16 months, during which participants received a seminar on diabetes management and oral health. The intervention was carried out by coaching face to face 5–6 times and 3–4 times with telephone sessions. Whereas in the health education group, the initial session was conducted two weeks after the oral exam recruitment process. Then followed by face-to-face sessions for two sessions and four sessions by telephone | Health coaching has a significant difference in the effect of decreasing HbA1c levels compared to the health education group, and there was a more significant decrease in the intervention group in patients with high-risk groups |
| Wayne et al. (2015)/Canada:Health coaching reduces HbA1c in type 2 diabetic patients from a lower socioeconomic status community: a randomized control trial | Patients from two primary care health centers in Toronto, Canada. Participants were divided into intervention groups (n=67), and controls (n=64) | The intervention group was given coaching via the smartphone application; participants were allowed to enter the web application 38 minutes/week to access information that supports goal setting and contact for 24h via message. Whereas the control group only conducted face-to-face coaching and telephone calls | There were no significant differences between the two groups in the sixth month, but there was a significant reduction in HbA1c in the intervention group in the third month |
| Wolever et al. (2010)/US:Integrative health coaching for patient with type 2 diabetes: a randomized control trial | A total of 56 participants were randomized into the intervention group (n=30), the control group (n=26) | The intervention was carried out for six months, divided into 14 sessions with face-to-face coaching and telephone calls. The duration of time given is 30min per session. The control group did not accept coaching interventions | Coaching significantly improved glycemic control by decreasing HbA1c levels during the 6-month intervention period in patients with poor HbA1c control |
| Varney et al. (2014)/Australia:Effect of hospital-based telephone coaching on glycemic control and adherence to management guidelines in type 2 diabetes, a randomized controlled trial | Recruitment was carried out on type 2 diabetes patients at Rs St Vincent's Melbourne diabetes clinic. the number of samples (n=94) was divided into the intervention group (n=47), the control group was (n=47) | The study was conducted for 12 months; the intervention group was given telephone coaching for six months conducted by a nutritionist. Duration in the initial session, there were usually 42 and 20-min sessions, but this duration was flexible depending on the time needed to set participants’ goals. In the control group, only regular maintenance was performed | Coaching showed significant improvement in the sixth month on HbA1c, fasting blood glucose, diastolic blood pressure, and physical activity during the six month evaluation period |
| Browning C et al. (2016)/China:Management of type 2 diabetes in China: The Happy Life Club, a pragmatic cluster randomized controlled trial using health coaches | 41 community health stations (CHS) were randomized into intervention group (21 CHS, n=372) and control group (20 CHS, n=296) | The intervention group was given a combination of face-to-face and telephone coaching plus regular care for 12 months. In the control group, only with usual care from each health clinic | Twelve months of intervention did not show a significant difference, but there was a significant decrease in HbA1c levels in both groups. Significant differences were seen in clinical outcomes in psychological pressure and diastolic blood pressure |
| Chapman et al. (2018)/China:Effect of a health coach intervention for the management of individuals with type 2 diabetes mellitus in china: a pragmatic cluster randomized controlled trial | 41 community health stations (CHS) were randomized into intervention group (21 CHS, n=385) and control group (20 CHS, n=345) | In the intervention group for 18 given regular care, face to face, and coaching via telephone. Coaching by telephone and face-to-face twice a month. In the control group only received usual care from each community health clinic | No significant effect was shown from glycemic control, but there was a decrease in HbA1c levels in both groups. The lack of different treatment effects in each community clinic can lead to suboptimal results |
Likewise, a study conducted by Wayne et al.12 showed results that significantly reduced HbA1c in type 2 diabetes mellitus patients. The study sample was diabetic patients who met recruitment criteria with medical records at a primary health clinic in Toronto, Canada. Participants were under 70 years old and had HbA1c ≥7.3% in a month. In this study divided the coaching intervention group with mobile applications (n=67) and the control group with face-to-face coaching and telephone contact (n=64). The intervention was carried out for six months. There were significant differences between the two groups at three months (p=0.03), at six months the results in both groups were found to be significantly reduced by 0.81% in the control group (p=0.01) and 0.8% (p=0.001) in the intervention group.
Another study also found the effect of coaching on glycemic control in Australia.13 The sample of this study was Diabetes mellitus patients in the diabetes clinic of St. Vincent Hospital Melbourne, with an adult age range, has an HbA1c >7%. Participants were randomly divided into coaching groups (n=47) and ordinary care groups (n=47) using block computers. Coaching interventions were carried out by telephone for 12 months with four to nine sessions, a flexible duration of time that at the beginning of the session usually carried out 45min and subsequent sessions for 20min. Coaching content is given focus on helping patients set goals and improve diet, physical activity, medication, and self-care. The results showed that patients showed significant differences in the two groups in reducing HbA1c (p=0.03), fasting blood glucose (p=0.02), diastolic pressure (p=0.03), physical activity (p=0.02). During the six-month evaluation, there were statistically insignificant differences in the two groups.
The study conducted by Cinar and Schou13 found that coaching had a better effect than health education in type 2 diabetes patients. In this study, participants were allocated randomly in the health coaching intervention group (n=77) and health education (n=111). Intervention coaching is carried out for ten months by dividing four sessions for coaching via telephone, and 5–6 sessions face to face. The results in this study coaching group significantly lowered HbA1c 7% compared to the health education group 0% with a significant difference (p<0.05), TBSES in the coaching group 61% and the health education group 25% with a value (p<0.01). While in the other two studies14,15 there was a decrease in HbA1c levels and both groups, but it did not show a significant effect in the intervention group, this could be due to the lack of supervision on the administration of different treatment effects and the lack of monitoring of the treatment given in each clinic. The study reviewed assessed the effect of coaching on glycemic control with HbA1c as a relevant measurement tool, but other clinical outcomes such as fasting blood glucose, self-efficacy, and physical activity can also support efforts to control blood glucose.
DiscussionThis study evaluated the effect of coaching interventions on glycemic levels, which indicated by HbA1c levels. An HbA1c level is a measuring tool for assessing glycemic control, which can be influenced by several factors, namely diabetes management such as diet, physical activity, knowledge, and treatment compliance.16 Coaching interventions are given with the aim of increasing patient positive behavior in diabetes management. This was also emphasized in a study that coaching intervention was the right method in helping patients maintain the results achieved by exploring goals, increasing self-efficacy to change behavior towards glycemic control.17
Coaching interventions with mobile applications may not be applicable in rural areas with network outreach that is not available and not cost-effective. Several coaching techniques used in the reviewed studies, such as face-to-face and telephone coaching can be recommended to be applied as an intervention and can be done by nurses who have attended training for health coaches to be able to facilitate and empower clients to achieve self-determined goals related to health.10 The duration of administration and duration of the intervention also varies; this can be due to the achievement of objectives for each different individual.
ConclusionThis study concluded that coaching interventions in patients with type 2 diabetes could be used as an intervention to control glycemic. The technique of coaching through face to face and telephone can be recommended.
Conflict of interestThe authors declare no conflict of interest.
Peer-review under responsibility of the scientific committee of the International Conference on Women and Societal Perspective on Quality of Life (WOSQUAL-2019). Full-text and the content of it is under responsibility of authors of the article.