The 3rd International Nursing & Health Sciences Students & Health Care Professionals Conference (INHSP) 2019
Más datosAnalyze how the COVID-19 exposure risk level in daily activity in adapting to new habits.
MethodsA cross-sectional online survey of the Indonesian adult population. Administered by an online questionnaire. A total of 497 samples, used a probabilistic sampling, collected between 20th and 24th June 2020. The sample lived in 108 districts across all 32 provinces in Indonesia.
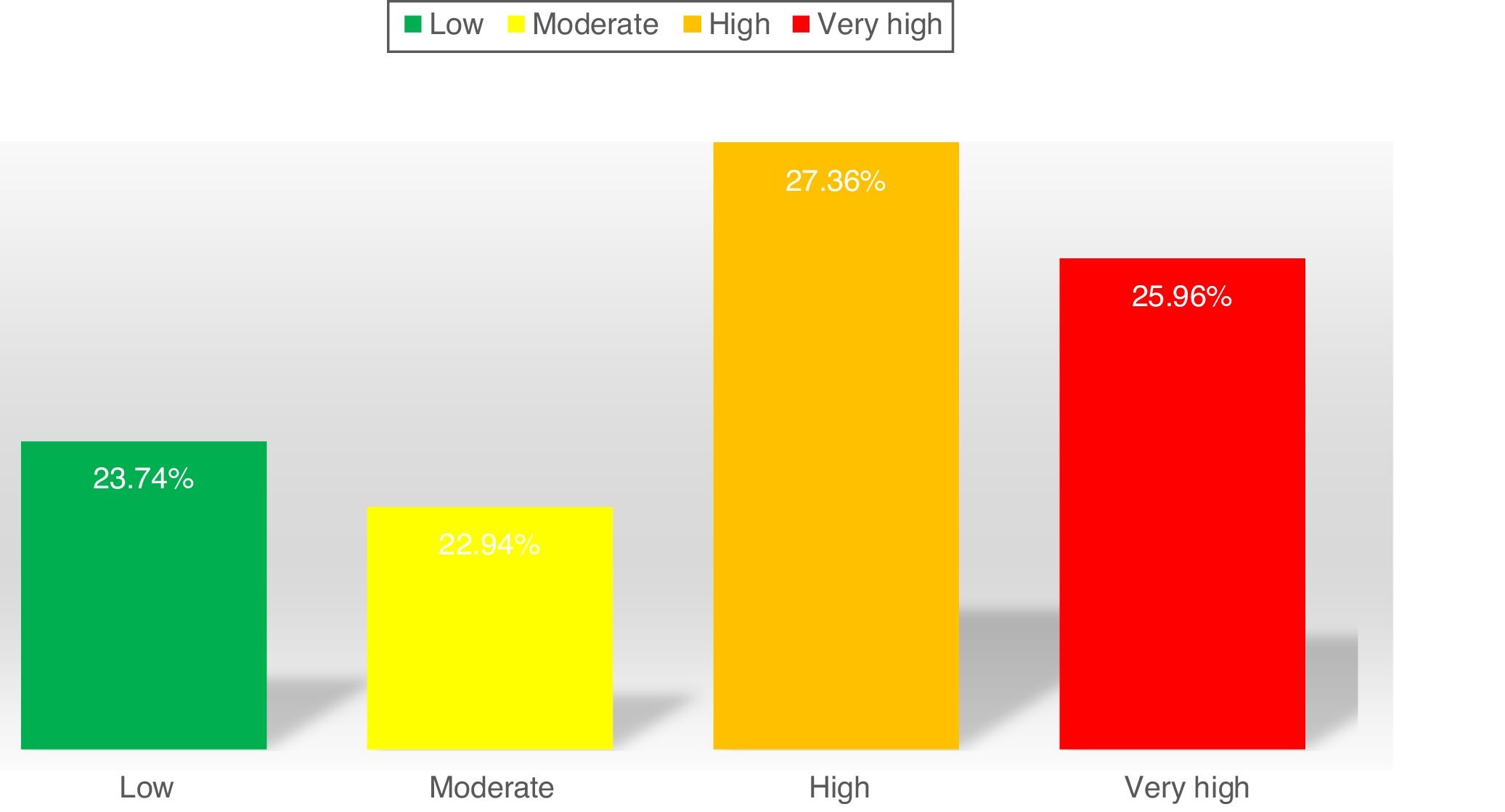
ResultWe found the distribution of COVID-19 exposure risk level in daily activities almost the same was 26.0% of participants had very high risk, 27.4% were high risk, 22.9% were moderate risk, and 23.7% were low risk. Male had activity risk level significantly lower than female (p-value 0.001). There are 14% of participants with a very high level of activity risk living in areas with uncontrolled virus transmission.
ConclusionThe risk of COVID-19 transmission occurs through a variety of activities carried out daily. All public meeting places have to consider compliance with health protocol to prevent it.
COVID-19 on 30 January 2020 as a Public Health Emergency of International Concern (PHEIC).1 Case in Indonesia reached 34,316 confirmed cases on 10th June and the largest number of confirmed cases in Southeast Asia.2,3 Performed strict physical distance measures instructing people to stay at home, gave evidence of a decrease in the transmission of COVID-19.4 The “fear” of the new virus, consistently predicted involvement in public health behaviors recommended by the government.5
Restrictions on community activities make sparked fears of an impending economic crisis.6 WHO support the government to adjust public health and social measures (PHSM) for relaxing.7 Indonesia starting a new normal policy so that economic activity can work, but still pay attention to health protocols. Government response with public health campaign advising people to protect themselves and others, including often handwashing with soap and water or alcohol-based hand sanitizer, physical distancing, and using a mask.
Reducing the rate of infection is a priority in the face of new infectious diseases, with no effective pharmacological interventions or vaccines available in the near future.8 Non-pharmaceutical interventions are effective decisions for governments because the timing and quality of implementation are closely related.9 A meta-analysis showed the effects of physical distance, face masks, and eye protection on virus transmission concluded none of these interventions afforded complete protection from infection.8 Lowering local transmission in the reduction of COVID-19 transmission is becoming important.10
In adapting new habits, the risk of COVID-19 transmission can occur through a variety of activities carried out daily. These activities do not have the same risk, some activities are riskier than others depending on the level of physical proximity to other individuals, how the activity has a high relationship with the spread of the disease, and the frequency of exposure to diseases or infections.11 Besides that, it really depends on the level of compliance.12
The impact of adapting new habits policy had not been studied in depth. Surely, it will cause changes in contact patterns and decreasing compliance with the easing of restrictions. Change in contact patterns on daily activities may increase the risk of exposure to COVID-19. This paper explores how the COVID-19 exposure risk level in daily activity.
MethodsA cross-sectional online survey of the Indonesian adult (aged 19 years over) population. The online survey was administered by an online questionnaire in which the survey link was shared with the WhatsApp group, Facebook with a public setting, a volunteer group. We requested approval before filling out the questionnaire. A total of 564 participants filled out the online questionnaire and 497 participants eligible (age 19 years over and complete data on all variables) for sample, used the probabilistic sampling method. The responding sample was weighted to be representative of the Indonesian adult population. The sample settled in 108 districts across all 32 provinces in Indonesia.
The questionnaire had five components: (1) socio-demographic characteristics, (2) domestic activities and general activities daily, (3) transportation activities, (4) consumption activities, (5) sport, health, and entertainment activities. Socio-demographic characteristics consisted of gender, age, marital status, Indonesia area of residence, and education level, and employment status. Domestic activities consisted of all daily activities carried out by the community at large, included activities at home, studying, working, and using public facilities and religious activities. Transportation activities consisted of using transportation facilities, such as private, public transportation, and online transportation. Consumption activities consisted of all activities related to the activities of shopping for goods, food, and vehicles. Sport, health, and entertainment activities consisted of activities such as sports, entertainment venues, and health and beauty consultations.
There are three choices of answers to the questionnaire statement: (1) did not do the activity, (2) comply means doing by complying to health protocol, including wearing a mask, washing hands use soap/hand sanitizer, and physical distancing (3) did not comply means doing it with not complying of health protocol. Analyses conducted descriptive statistics and bivariate analyses with Chi-squared tests in SPSS version 25.
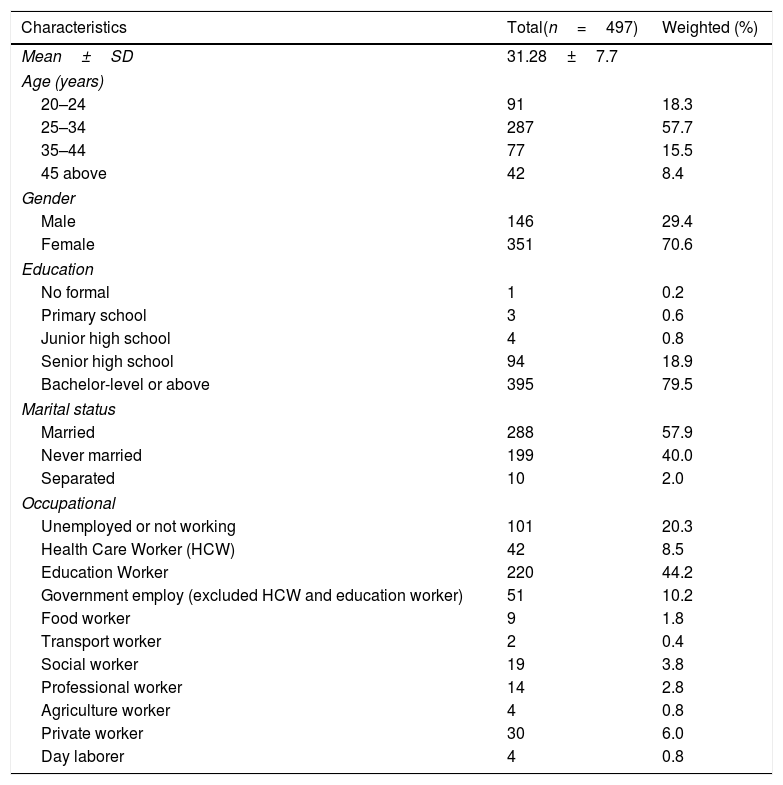
ResultWe surveyed 497 Indonesian participants. Data were collected between 20th and 24 June 2020, about 1 month after WHO supported the Ministry of Health in developing guidance and protocols in various sectors for the “new normal” scenarios.13 The average age of participants was 31.2 years±7.7 SD, and 70.4% (350/497) were female. The majority of respondents were bachelor-level or above (79.5%), and 57.9% (288/497) of respondents reported being married.
Overall, participants reported their specific occupation, we category more simple for detail are reported in Table 1. Twenty percent were unemployed, the majority of participants were education workers where education institutions still work from home at the time of this study, and 8.5% (42/497) working as health care workers (HCW) i.e. nurses, a midwife.
The socio-demographic characteristic of participants (n: 497).
| Characteristics | Total(n=497) | Weighted (%) |
|---|---|---|
| Mean±SD | 31.28±7.7 | |
| Age (years) | ||
| 20–24 | 91 | 18.3 |
| 25–34 | 287 | 57.7 |
| 35–44 | 77 | 15.5 |
| 45 above | 42 | 8.4 |
| Gender | ||
| Male | 146 | 29.4 |
| Female | 351 | 70.6 |
| Education | ||
| No formal | 1 | 0.2 |
| Primary school | 3 | 0.6 |
| Junior high school | 4 | 0.8 |
| Senior high school | 94 | 18.9 |
| Bachelor-level or above | 395 | 79.5 |
| Marital status | ||
| Married | 288 | 57.9 |
| Never married | 199 | 40.0 |
| Separated | 10 | 2.0 |
| Occupational | ||
| Unemployed or not working | 101 | 20.3 |
| Health Care Worker (HCW) | 42 | 8.5 |
| Education Worker | 220 | 44.2 |
| Government employ (excluded HCW and education worker) | 51 | 10.2 |
| Food worker | 9 | 1.8 |
| Transport worker | 2 | 0.4 |
| Social worker | 19 | 3.8 |
| Professional worker | 14 | 2.8 |
| Agriculture worker | 4 | 0.8 |
| Private worker | 30 | 6.0 |
| Day laborer | 4 | 0.8 |
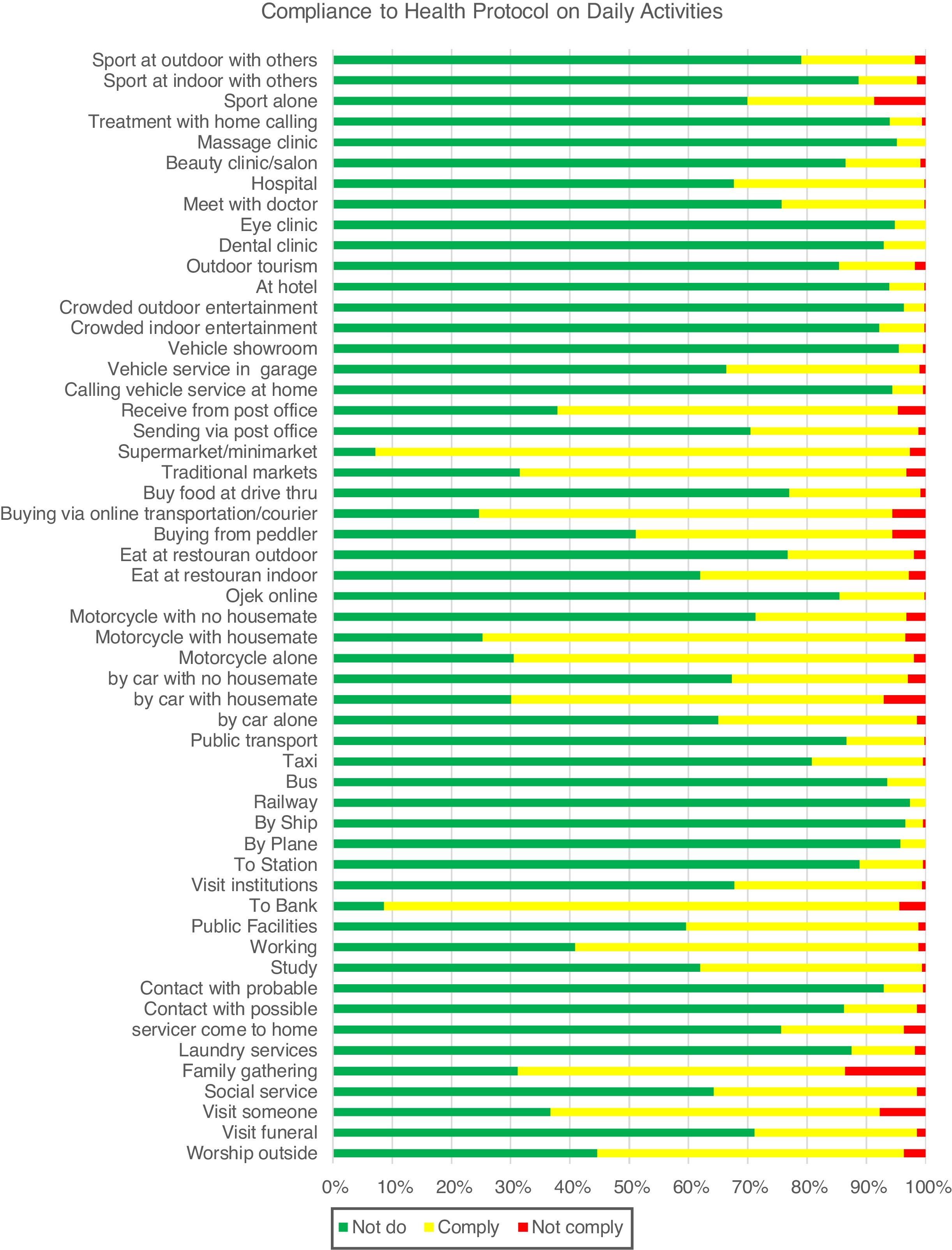
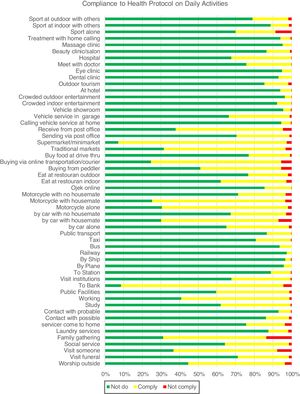
Our findings in compliance with health protocol on all of the daily activities are detailed in Fig. 1. Most reported in all activities were respondents did not do an activity (69.43%), then did with complying (28.50%), and lowest did with not comply (2.06%).
We defined the risks score of daily activities based on 3 indicators: compliance with health protocol, how the activity has the level of physical proximity (closed contact), and how the activity has a high relationship with the spread of the disease (closed spaces, crowded space). The activity risk weighting score was 0–4 i.e.: Score 0 if the activity is not done. Score 1 if the activity is carried out by comply, had closed contact, or closed/crowded space. Score 2 if the activity is carried out by comply, had closed contact, and closed/crowded space. Score 3 if the activity is carried out by not comply, had closed contact, or closed/crowded space. Score 4 if the activity is carried out by not comply, had closed contact, and closed/crowded space.
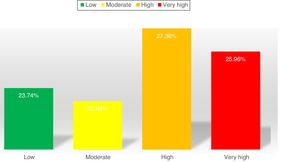
After that, we categorize COVID-19 risk levels based on quartile data from accumulated risk scores. Score 0–23 for low risk, >23–31 for moderate risk, >31–41 for high risk, >41 for very high risk. The overall distribution of COVID-19 risk level in daily activities, almost the same were 26.0% (129/497) very high risk, 27.4% (136/497) high risk, 22.9% (114/497) moderate risk, and 23.7% (118/497) low risk (Fig. 2).
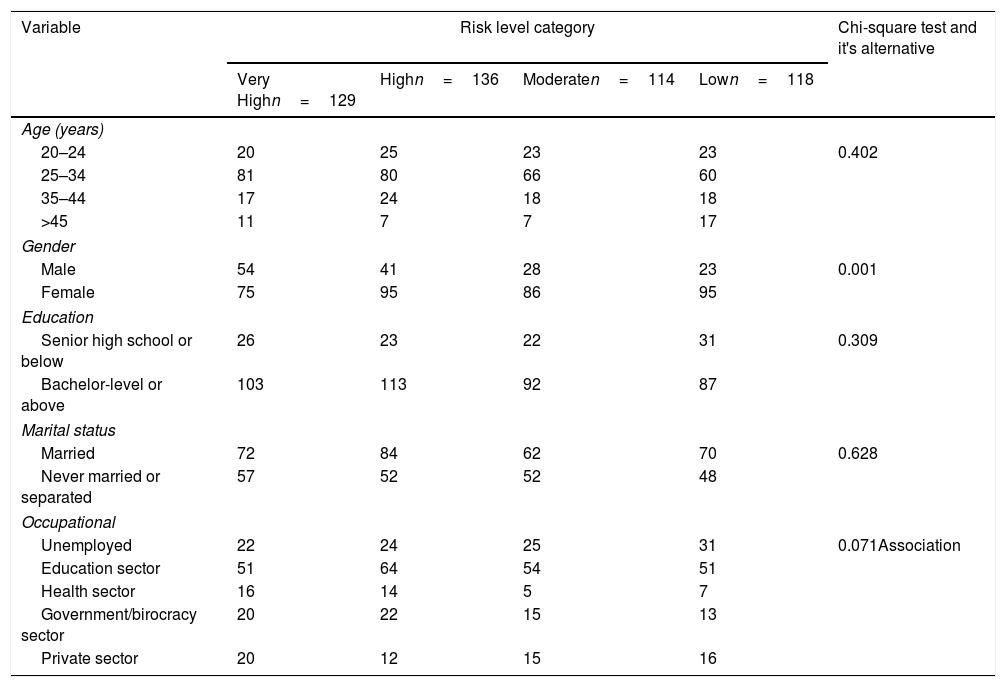
Based on Table 2, the result of the proportion difference test found there is no significant difference in the activity risk level between age groups, education level, marital status, occupational sector proportion. There is a statistically significant difference in the risk level between gender. Male proportion on very high activity risk (15.8%) lower than female (27.1%), also on high activity risk (19.2%) versus (24.5%).
Proportion difference of activity risk level between socio-demography variable (n=497).
| Variable | Risk level category | Chi-square test and it's alternative | |||
|---|---|---|---|---|---|
| Very Highn=129 | Highn=136 | Moderaten=114 | Lown=118 | ||
| Age (years) | |||||
| 20–24 | 20 | 25 | 23 | 23 | 0.402 |
| 25–34 | 81 | 80 | 66 | 60 | |
| 35–44 | 17 | 24 | 18 | 18 | |
| >45 | 11 | 7 | 7 | 17 | |
| Gender | |||||
| Male | 54 | 41 | 28 | 23 | 0.001 |
| Female | 75 | 95 | 86 | 95 | |
| Education | |||||
| Senior high school or below | 26 | 23 | 22 | 31 | 0.309 |
| Bachelor-level or above | 103 | 113 | 92 | 87 | |
| Marital status | |||||
| Married | 72 | 84 | 62 | 70 | 0.628 |
| Never married or separated | 57 | 52 | 52 | 48 | |
| Occupational | |||||
| Unemployed | 22 | 24 | 25 | 31 | 0.071Association |
| Education sector | 51 | 64 | 54 | 51 | |
| Health sector | 16 | 14 | 5 | 7 | |
| Government/birocracy sector | 20 | 22 | 15 | 13 | |
| Private sector | 20 | 12 | 15 | 16 | |
Indonesia began relaxing large-scale social restrictions (PSBB) and implementing a new normal of activity by opening up all economic, social, and public activities. The community can back work, study, and socialize to be productive in the pandemic era. This makes the people who have to stay at home back to carry out activities with the adaptation of new habits while maintaining a health protocol to COVID-19. It to protect oneself and others with the discipline of healthy living by frequently washing hands, wearing masks, and keeping a distance.14
Distribution of exposure risk level category is very high, high, moderate, and low almost the same indicates the level of prevention efforts that still varies. The risk of COVID-19 transmission occurs through a variety of activities. It depending on the level of compliance, the level of physical proximity, and how the activity has a high relationship with the spread of the disease.11,12 Very high levels are them that back to carry out the activity in enclosed, crowded areas where it is difficult to maintain a social distance and people are in close contact, the risk of infection is greater. Such as use public facilities, traveling by public transportation, dining in an indoor restaurant, visit the traditional market, visit crowded entertainment, and sport indoor. So, highly recommended to reduce risky activities and increase compliance with activities that are very urgent to do.
In this research, the high level of compliance is estimated by the “fear” and anxiety in the community of this new virus. Adaptive public health-compliant behavior change is predicted by negative emotions (fear and anxiety) in response to the current pandemic (e.g. washing hands, social distancing).15 The main factors influencing compliance during the outbreak were people's understanding of the disease and quarantine procedure, social norms, perceived quarantine benefits and perceived disease risk, as well as practical problems such as running out of supplies or the financial consequences of out of work.16 The appeal to altruistic motives to comply with distancing instructions appears to maintain motivation over an extended period of time to maintain social distance from others.17
Compliance with prevention can change the level of risk significantly. The study reported moderate-frequency washing hands predicted a lower personal risk of coronavirus infection 35%.18 At least 1 m physical distance is likely associated with a large 85% reduction in infection.8 Use of face mask could result in a large 70% reduction in risk of infection for surgical mask and 45% cotton mask. At all times in public, people should wear their masks properly.19 Following all recommendations could result in 84% of COVID-19 infection burden being controlled.20 None of these interventions provided complete protection against infection, and a risk assessment and several contextual considerations might be required for their optimal role.8
There is no difference in the activity risk level between socio-demographic variables, this explained that the impact of this pandemic was evenly distributed to all communities. But on gender, the high-risk proportion of females higher than males. Females and males have different life and health experiences because of biological, psychological, economic, social, political, and cultural attributes and possibilities. Also different travel and activity patterns.21 These differences can impact health status.22 A evidence found a female higher risk to exposure COVID-19 related stress disorders and occupation, like family caregivers and higher occupational risks of exposure to COVID-19, such as health care workers, further exacerbate stress exposure.11,23–26
Recommendation for the implementation and adoption of new habits in many countries around the world as measures against COVID-19, it is important that continue to promote personal protective measures and campaign to all public meeting places consider all steps for potential prevention against COVID-19. Limitation of this study because the collection of data online: (1) limited access, so that those living in areas with limited internet access did not have a chance to participated, (2) there is no interviewer, the respondent will misinterpret or read the instructions for filling out the form superficially. In this context, the data collected would most likely be of poorer quality than data collected via an interview, (3) auto-selection bias: if only those groups of people who are either more inspired or have better internet skills participate in the survey, the results would be biased.
ConclusionThis paper has presented cross-sectional data demonstrating, in real-time, COVID-19 risk level in daily activities in response to a global viral pandemic. We have shown that risk from community activities after back again work, study, and socialize activity in new habits adapting era. The risk of COVID-19 transmission can occur through a variety of activities carried out daily. Compliance with health protocol to prevent COVID-19 must be recommended massive. All public meeting places consider all steps for potential prevention against COVID-19 and the public must comply with wearing masks, washing hands, and social distances in daily activities all the time.
Ethical approvalThe study team strictly followed ethical standards in research, although ethics approval documents are not available; that is, we ask for approval before becoming a participant, all individual information was strictly kept confidential and not reported in the paper.
Conflict of interestAll authors declare no conflict of interest.
Peer-review process of the 3rd International Nursing & Health Sciences Students & Health Care Professionals Conference (INHSP) 2019 is under the responsibility of the scientific committee of the 3rd International Nursing & Health Sciences Students & Health Care Professionals Conference (INHSP).