The increased prevalence of complex chronic diseases in all stages of life, the progressive aging of the population, the prevalence of multimorbidity, polypharmacy, and loss of autonomy, have given rise to new needs in society. The current model of care is failing to meet these needs in an effective or sustainable way.
People with complex chronic diseases are vulnerable, they deteriorate as diseases progress, and they require individualised and coordinated professional care that takes into account the progression of the disease, transitions and people's preferences.
It is essential to determine a new care paradigm as a framework for the projects and actions that should be promoted to reach transversal, sustainable and quality care directed at people with complex and advanced chronic diseases in all stages of life.
Different studies show that case management is an added value in terms of quality, safety and cost-effectiveness. However, its implementation in Spain is uneven and heterogeneous, and no regulations have yet been developed to give stability to this new nurse figure. The Ministry and the Autonomous Communities now have the responsibility to create regulations and institutionalise the figure of case management nurses/advanced practice nurses, with a clear definition of their professional competences and functions, as has been done in other countries.
El aumento de la prevalencia de enfermedades crónicas complejas en todas las etapas de la vida; el progresivo envejecimiento de la población; la prevalencia de multimorbilidad, la polimedicación, y la pérdida de autonomía, han hecho emerger nuevas necesidades en la sociedad, a las que el actual modelo de atención no está dando respuestas eficaces ni sostenibles.
Las personas con enfermedades crónicas complejas son vulnerables, se van deteriorando a medida que las enfermedades progresan, y requieren cuidados profesionales individualizados y coordinados, que tengan en cuenta la progresión de la enfermedad, las transiciones y las preferencias de las personas.
Es imprescindible determinar un nuevo paradigma de atención en el que enmarquemos los proyectos y las acciones que se deben impulsar para avanzar hacia una atención transversal, de calidad y sostenible dirigida a las personas con enfermedades crónicas complejas y avanzadas en todas las etapas de la vida.
Diferentes estudios demuestran que la gestión de casos es un valor añadido en términos de calidad, seguridad y coste-efectividad. Sin embargo, su implementación en España es desigual y heterogénea, no habiéndose desarrollado aún normativa alguna que dé estabilidad a esta nueva figura enfermera. El Ministerio y las Comunidades Autónomas, tienen ahora la responsabilidad de crear normativa e institucionalizar la figura de enfermera gestora de casos como modelo de práctica avanzada, con una definición clara de sus competencias y funciones, tal y como se ha hecho en otros países.
Since the prevalence of chronic diseases (CD) in all life stages is rising and its distribution is unequal an in-depth demographic approach to this reality with the greatest fairness possible is crucial. A major part of the human and social impact caused each year by deaths relating to CD could be avoided by viable and economical interventions.1
The prevalence of multimorbidity and pluripathology increases with age, reaching a mean of 2.8 CD in people aged between 65 and 74, and 3.23 in people over 75.2 The multimorbidity associated with ageing and polymedication lead to disability, dependence,3 and finally complexity.
Health and social systems in Spain are facing one of the highest rates of ageing and chronicity in the whole of Europe with a clearly rising trend. 91.3% of mortality and 86% of life years lost are attributable to CD.4
Furthermore, technological and scientific advances have contributed to the increase in survival of many diseases, leading to an increase in chronicity and complexity in children and teenagers. This requires a new comprehensive and coordinated healthcare model to include primary care (PC), hospital care, social services and education In order to achieve an as normalised as possible life and schooling.5
It has been estimated that complex chronicity accounts for between 3% and 5% of the population.6 These people are a homogeneous population in complexity, vulnerability, fragility, mortality, functional impairment, polypharmacy and frequent situations of dependency, since they are heavy consumers of health and social resources. However, the clinical practice guidelines, mainly designed for a single health problem, have major limitations regarding comorbidity and pluripathology, particularly when there are comorbidities which do not share the same physiopathological mechanism.7
The complexity of people with CD from the person's own viewpoint concerns the loss of functionality and the spiral o, fragmented and uncoordinated contact with the health services, where patients and family members do not know what to do and feel overwhelmed by the maze of staff, environments and interventions, in addition to the presence of socioeconomic factors which increase this perception of complexity.8,9
Within this setting of multimorbidity, progressive ageing, hospitalisation and the indiscriminate use of technology our healthcare system has both responded badly to people and also become ineffective and unsustainable.10 The development of case management as advanced practice care has become a basic strategy in complex chronicity care in Spain. However, in order to guarantee the best multiprofessional, coordinated and evidence-based care it is essential to synergically impose contentious, coordinated actions in the different areas within the same territory and population.11
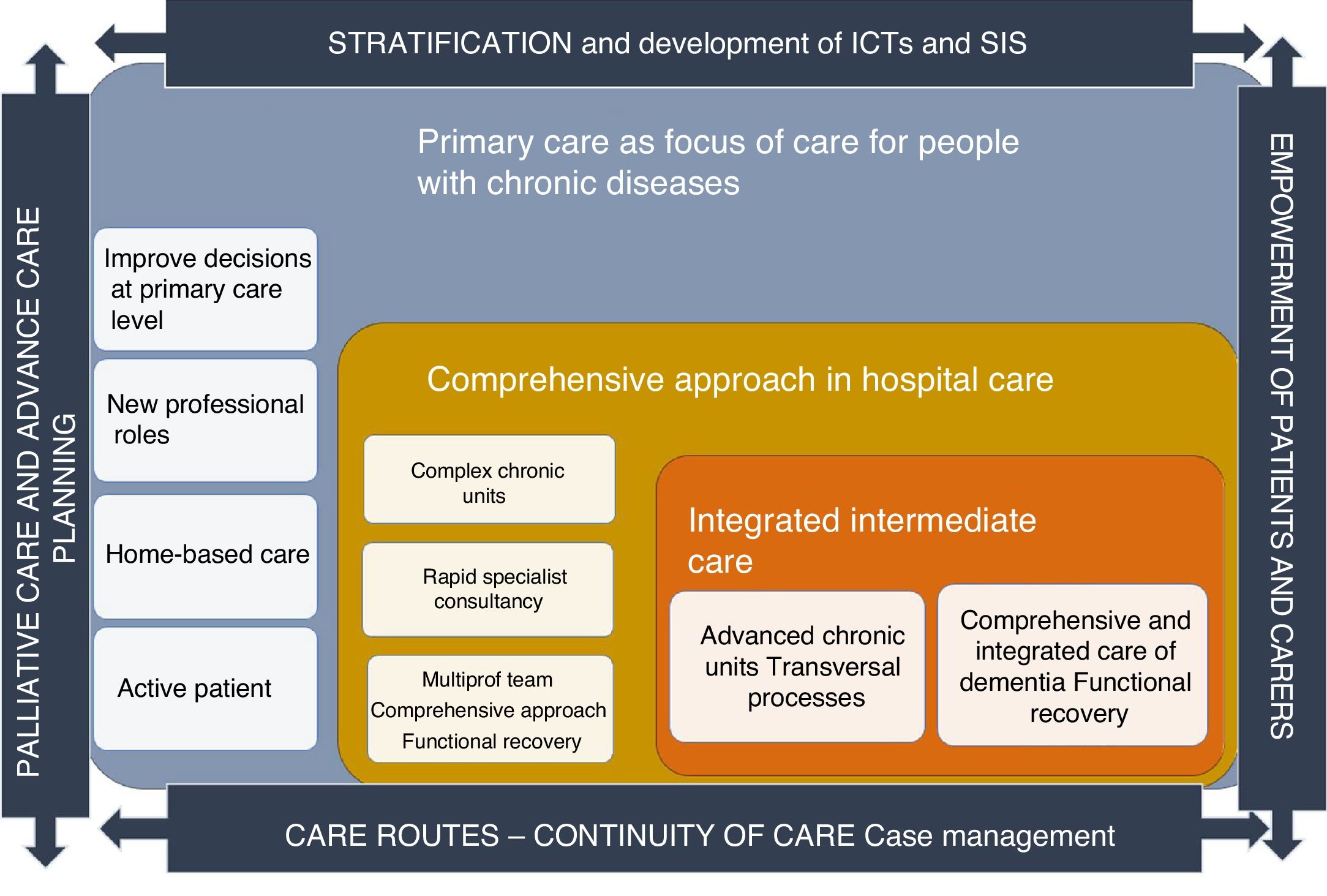
A new care paradigm: personalised, comprehensive, efficient and sustainableThe strategic chronicity care map (Fig. 1 contains an example of strategic projects which may be simultaneously implemented to create alliances between care areas are suggested. These projects may put together the foundations of a proactive, comprehensive and individualised model which will lead to a quality, efficient and sustainable care.5 We will now suggest some key elements to this procedure.
Strategic map of the chronicity care plan of the Balearic Islands.
Modified by Miguélez-Chamorro et al.5
Population stratification is key to identifying individuals according to their complexity and morbidity. Their incorporation into computerised clinical files serves as a “reminder” to the practitioners to take planned and appropriate decisions for the social and healthcare needs of people with CD.2 Furthermore, the development of ICT helps practitioners to take decisions whilst also being an essential element for the empowerment of the population, self-care, treatment adherence and connection between patients and practitioners.
Primary care as a focus of care in people with chronic illnessesHealth systems aimed at PC which focus attention on people and their needs, achieve better results in health at lower costs. To improve the clinical effectiveness of current chronicity and fragility and reduce the epidemic of over diagnosis and disproportionate interventionism, PC requires strengthening.12,13 Programmes with specific interventions in the community area which guarantee personalised and continuous care, are able to reduce the number of hospital admittances and mean hospital stays.14
The national strategy for approaching chronicity in the National Health System15 and the World Health Organisation resoundingly confirms that PC should be the focus of attention for people with CD.16 Guaranteeing planned and proactive homecare to people is more effective and efficient than institutionalised care.17 In PC the nurse case manager proactively gathers together people with chronic complex and advanced disease (CC and AD) to adapt care and ensure equity in home care, and guarantee continuity of care. He or she supports the team and is the care benchmark, activating and coordinating care opportunities in transitions, with the prevention of inappropriate hospitalisations as a result.18
New hospital models that prevent functional impairment on admittances and prioritise functional recoveryFunctional impairment of the elderly during hospital stays is a serious problem due to its high incidence and the serious consequences in terms of dependence, institutionalisation, and the high use of resources and mortality.19 Barisonzo et al. confirm that clinical attitudes and hospital organisation are the most common reasons for the existence of inappropriate stays.20 The reversal of these serious consequences is in the hands of the health services which may create specific units with a multiprofessional approach, focusing on comprehensive care to people with CCD and enhancing the person's Independence and autonomy.
Intermediate care (IC) hospitals aim to recover functional capacity and reduce the rate of long-term institutionalisation. IC has been scientifically proven without a doubt to significantly improve mortality rates, reduce institutionalisation, improve functional ability in basic activities instrumental to daily life, improve the cognitive situation, reduce hospital re-admittance and care costs.21 Its implementation will be a key determinant in care quality, safety and expenditure, and strategy will consist of defining care routes between IC and PC.5
The NCM plays a pivotal role in IC. In an analytical observational cohort study of people with CCD García-Fernández et al. showed that when the NCM was involved, the cohort achieved better results midterm regarding dependency and overburden of the carer; hospital re-admittance rates; consumption of resources and achieved better satisfaction in care and continuity of care.22
Design of clinical treatment routes and specific care routes for patients with complex chronic diseases where the nurse case manager (NCM) will be the flow managerTo ensure quality and safe transitions, it is essential to design clinical and specific care routes for people with CCD, where the undertaking of each activity and care intervention is perfectly defined with regard to what, who, how, when and where this should take place. According to the study by Gallud in Valencia the NCM boosts care, improves care integration and continuity of care and considerably reduces the need for emergency services and hospital admittance for people with CCD.18 When the person returns home with a poorer health status, the NCM's intervention is key to them adapting to the new situation, ensuring resources and support are available to the person and the family.23
Guarantee care coordination and continuity with the NCMCoordination within the health system and with social services is essential to guarantee resource availability, continuity of care, quality of care and for users to be central to the organisation.24
In 2002 the Canary Islands and subsequently Andalusia were pioneer in the introduction of the NCM, aiming at ensuring continuity of care, and guaranteeing safe and high quality home care for fragile and dependent people. In 2005 this figure was introduced in Catalonia although they evolved differently due to the wide variety of health service provision. Valencia, the Balearic Islands and the Basque Country initiated pilot studies from 2007 to 2011. Evaluation in Valencia18 and the Basque Country,25 together with political and organisational support led to this figure being introduced into both communities. Almost all autonomous communities have designed care strategies for chronicity using more or less disruptive change proposals and with the drive for coordination and care continuity projects led by nurse case managers being a constant.26 However, they lack a conceptual and legal framework with well-defined NCM functions and competences, and this has led to ambiguities and conflicts affecting satisfaction and work performance.8
The NCM and complex chronicity: results and new proposalsThe assessment of the different case management models is complex, because it takes place in specific models, population groups and contexts, and this makes generalisation difficult.8,27
One study centred on the analysis of case management in the Canary Islands, shows an improvement in the clinical results and greater efficiently of resources, promoting higher use of social workers.28 In Andalusia, the 2008 ENMAD study highlights that intervention of the NCM improves the autonomy of immobile people, reducing the overburden of carers, improving the therapeutic plan and activating the use of social work and physiotherapy services.29
Internationally there is also evidence that case management improves functionality and the appropriate use of drugs, increases the use of community services and reduces institutionalisation.27
Furthermore, studies on the clinical effectiveness of management programmes of care transitions aimed at patients over 65 with pluripathology or considered geriatrics or with fragility or polymerisation have been proven to considerably statistically reduce mortality rates at 3, 6, 12 and 18 months post hospital discharge and a reduction of hospital re-admittances at 3, 6, 12, and 18 months, without finding differences in quality of life. The NCM, who are responsible for coordination and care continuity play a pivotal role.23
In Spain, the impact of nursing interventions was assessed in chronicity care, concluding that interventions carried out by NCM are more effective in their approach to people with CCD, than those undertaken using standard methods.30
Morales-Asencio8 defines the keys to success in the introduction of the NCM, which include the following: define the NCM role and competences with a clear conceptual and legal framework for all professionals.
Despite the results and formal recognition of the NCM in the care of people with CCD, the degree of involvement of the NCM is heterogeneous in the autonomous communities and in none has permanent functioning with legal security been consolidated. The lack of a legal and retributive framework by the state is a huge barrier to the consolidation of this figure of proven efficiency and efficacy.31
The Autonomous Communities, together with the Ministry of Health, are responsible for courageously institutionalising the figure of the NCM and moving beyond health planning which promotes administrative factors, but does not ensure continuity or formal institutionalisation. A necessary and urgent previous step to this is to abolish the Medicines (Guarantees and Rational Use) law 29/2006, as well as Royal Decree 954/2015, because they limit prescription by nurses in Spain in their area of competence, thus blocking decisive and quality care to the general population and the development of effective and efficient advanced nursing practice. Andalusia is the only community with regulated nursing prescription and has demonstrated that this prescription by nurses supports quality and efficiency to care.32 A law is urgently required to enable nurses to prescribe in all areas of their competences because they have already been qualified to do this through their university degree.
Case management from advanced practice for long-term quality care to people with complex chronic illnessesAccording to the 2009 Case Management models of Ontario,33 by the Case Management Society of America of 2016,34 and the most consolidated case management programmes of Spain, we may say that it is the NMS function to provide excellent individualised care to people with complex care needs, dependency and fragility, enhancing preventative activities which promote self-care and improvement in quality of life. They must also collaborate with the professionals involved in this process to offer appropriate health management, taking into account personal preferences, encouraging accompaniment, minimising elements of fragmentation, discontinuity and/or duplicity in care, through shared decision making and with the use of the available resources, to promote safe and cost-effective quality care. Among the competences expected of this professional are the ability to work in multiprofessional teams, the capacity to provide advanced care, manage conflicts and the possession of communicative and motivating skills, together with the ability for critical thinking and inquisitiveness regarding innovation.31 The international council of nurses’35 definition of the advanced practice nurse provides a reference, proving that the nurse case manager in the Spanish health system context possesses advanced practice competences.
The creation of a technical commission in the Ministry may be a good beginning to define the competences and functions of the NCM in every area of care from consensus, to later create laws and institutionalise the figure of the NCM, with clear indications of the selection and assessment. The work of Andalusia and the Basque Country may be a good starting point.
Advanced practice competences developed by the NCMsThe clinical practice which involves direct and indirect care of patients and their families, groups, communities or populations is the main objective of the APN functions. Apart from clinical practice, other responsibilities of their role include training nurses and other health professionals, evidence-based practice and research, leadership in organisation and professional development.35,36
There is a lack of international consensus on the precise definition and the competences associated with APN roles,37 related to the academic training level of the profession, the legal framework regulating the nursing profession and the health system features of each country.
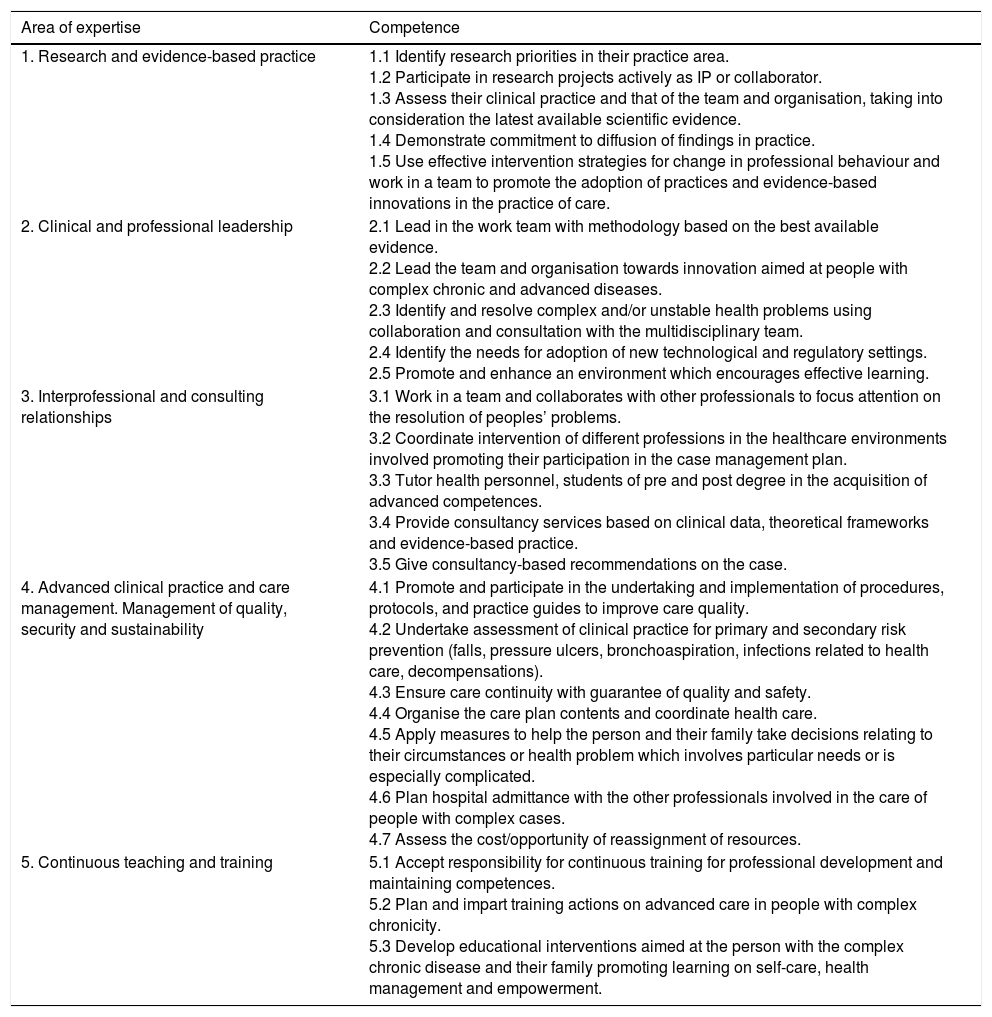
The National Health Service, in the case management framework document for care of people with CD,38 determines that the competences of the NCM will depend on the target population and the results expected to be obtained with their intervention. Bearing in mind the target population at which the case management is directed at (people with CC and AD and/or fragility, dependency and raised vulnerability) we have put forward a proposal for advanced practice nurse competences in Table 1 in case management, having first analysed the models of advanced practice of the Nurses Association of Canada,36 the NHS,35 the classification of work by Sastre-Fullana et al.,37 and the NCM competence model as defined by the Andalusian Health Service.39
Areas of expertise and competences of the advanced practice nurse in case management.
| Area of expertise | Competence |
|---|---|
| 1. Research and evidence-based practice | 1.1 Identify research priorities in their practice area. 1.2 Participate in research projects actively as IP or collaborator. 1.3 Assess their clinical practice and that of the team and organisation, taking into consideration the latest available scientific evidence. 1.4 Demonstrate commitment to diffusion of findings in practice. 1.5 Use effective intervention strategies for change in professional behaviour and work in a team to promote the adoption of practices and evidence-based innovations in the practice of care. |
| 2. Clinical and professional leadership | 2.1 Lead in the work team with methodology based on the best available evidence. 2.2 Lead the team and organisation towards innovation aimed at people with complex chronic and advanced diseases. 2.3 Identify and resolve complex and/or unstable health problems using collaboration and consultation with the multidisciplinary team. 2.4 Identify the needs for adoption of new technological and regulatory settings. 2.5 Promote and enhance an environment which encourages effective learning. |
| 3. Interprofessional and consulting relationships | 3.1 Work in a team and collaborates with other professionals to focus attention on the resolution of peoples’ problems. 3.2 Coordinate intervention of different professions in the healthcare environments involved promoting their participation in the case management plan. 3.3 Tutor health personnel, students of pre and post degree in the acquisition of advanced competences. 3.4 Provide consultancy services based on clinical data, theoretical frameworks and evidence-based practice. 3.5 Give consultancy-based recommendations on the case. |
| 4. Advanced clinical practice and care management. Management of quality, security and sustainability | 4.1 Promote and participate in the undertaking and implementation of procedures, protocols, and practice guides to improve care quality. 4.2 Undertake assessment of clinical practice for primary and secondary risk prevention (falls, pressure ulcers, bronchoaspiration, infections related to health care, decompensations). 4.3 Ensure care continuity with guarantee of quality and safety. 4.4 Organise the care plan contents and coordinate health care. 4.5 Apply measures to help the person and their family take decisions relating to their circumstances or health problem which involves particular needs or is especially complicated. 4.6 Plan hospital admittance with the other professionals involved in the care of people with complex cases. 4.7 Assess the cost/opportunity of reassignment of resources. |
| 5. Continuous teaching and training | 5.1 Accept responsibility for continuous training for professional development and maintaining competences. 5.2 Plan and impart training actions on advanced care in people with complex chronicity. 5.3 Develop educational interventions aimed at the person with the complex chronic disease and their family promoting learning on self-care, health management and empowerment. |
We prefer to talk of competence areas instead of domains, as we believe this is a clearer term and we decided to eliminate the competences nurses with degrees in Spain already have.
It is important to study in greater depth and debate the advanced practice in each specific area of knowledge and to be clear about the difference between an advanced practice nurse and a specialist who acquires competences and greater autonomy in the area of their specialty.
ConclusionsThe general population and therefore patients have changed. The way in which people fall ill is different and technologies have revolutionaries how we live, making it necessary to re-design the healthcare model where the citizen becomes the focus and participates in their health process.
To guarantee the sustainability, quality and safety of the most complex and fragile cases, there is an urgent need to introduce an integral care model which guarantees multiprofessional and coordinated care. To do so requires synergic and disruptive changes to the framework of a new paradigm, in which the advanced practice NCM plays an essential role in all care areas. This will ensure quality care in the best care environment and an efficient use of resources in the whole healthcare process for people with CCD.
The NCMs have proven to be an added value throughout the care process for people with CCD. They guarantee professionalised, integral and continuous care to society's most vulnerable people, whilst considering their preferences and priorities and their potential for recovery from a multiprofessional stance.
It is important to establish a legal and regulatory framework for consolidation of advanced practice case management, in which professional competences are defined. This will continue contributing quality and security to the processes of people with ECG, but without variability, with the best available evidence, pointing the way towards necessary research in CC and AD care.
Conflict of interestsThe authors have no conflict of interests to declare.
Please cite this article as: Miguélez-Chamorro A, Casado-Mora MI, Company-Sancho MC, Balboa-Blanco E, Font-Oliver MA, Román-Medina Isabel I. Enfermería de Práctica Avanzada y gestión de casos: elementos imprescindibles en el nuevo modelo de atención a la cronicidad compleja en España. Enferm Clin. 2019;29:99–106.