A three-month old infant, with no relevant history, born by vaginal delivery with no complications, was seen in the emergency department as she had a lesion on her scalp which was detected by her parents 4–5 weeks ago, and which had grown progressively since then. The patient did not have a fever or general symptoms and no lesions were observed at other sites. The parents denied previous wounds or lesions in the area. In the emergency department, a fungal and bacterial culture was performed with a negative result, and treatment was started with corticosteroids and topical antifungals with no improvement. It was therefore decided to refer the patient to the Dermatology department. In the consultation, during the physical examination, we observed a verrucous plaque formed by multiple grouped papules of follicular distribution, some of which had a cystic appearance, measuring around 2cm in diameter in the right parieto-occipital region (Fig. 1). As viral plaque warts vs congenital molluscum contagiosum infection was suspected, a small area was shaved. A physical examination of the mother's genitalia was performed. She did not have any lesions at the time.
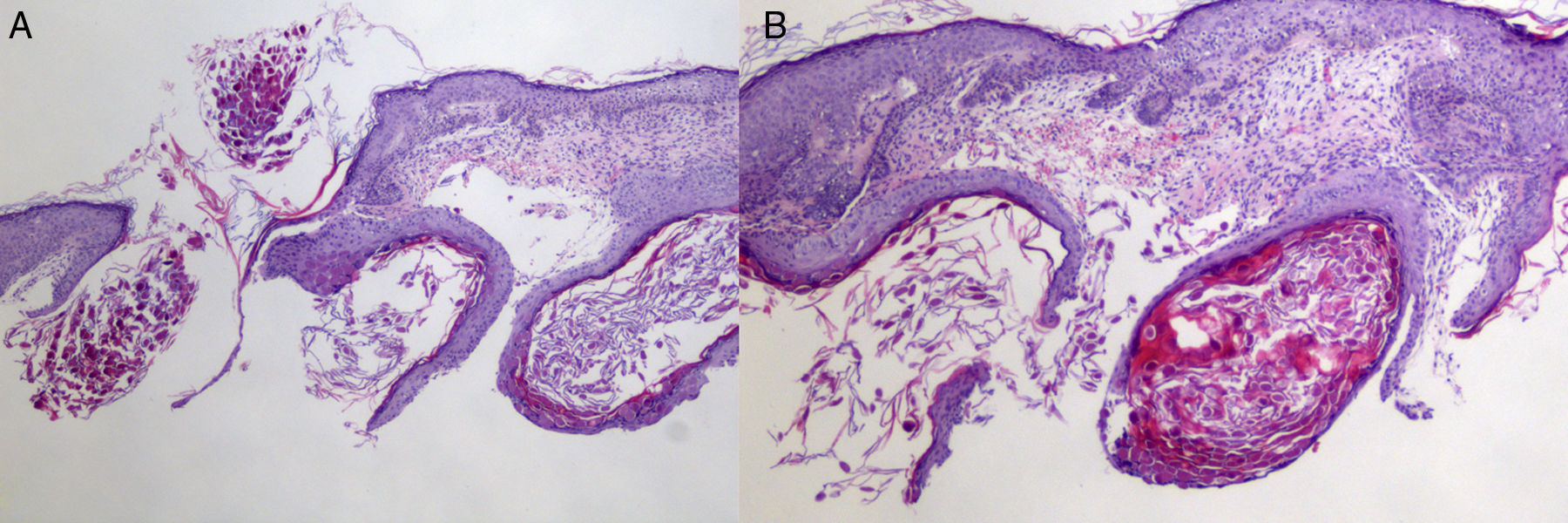
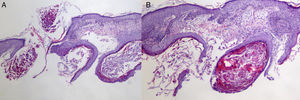
Clinical courseThe histological study revealed the presence of follicular epithelium lobes open at the skin surface which penetrated the dermis (Fig. 2A). We were able to observe the typical inclusion bodies in the cytoplasm of the keratinocytes, which increased in size from the basal layers to the more superficial layers of the epidermis, in turn increasing their basophilia. This resulted in a diagnosis of molluscum contagiosum viral infection (Fig. 2B). The follicular distribution of the infection was striking, with lesions observed only in the follicular epidermis. Once the diagnosis had been made, treatment was started with a dilute KOH solution, presenting significant improvement within two weeks, with only 3–4 residual papules observed.
(A) Panoramic view of molluscum contagiosum infection's follicular involvement, observing follicular epithelium lobes which penetrate the dermis where the characteristic inclusion bodies of the virus are seen. (B) At a higher magnification, we can see in detail how these inclusion bodies increase in size from the more basal layers to the more superficial layers, becoming more basophilic.
Molluscum contagiosum is a double-stranded DNA virus belonging to the family of Poxviruses.1 This infection, which is very common in children and relatively common in the genitalia of young adults, has rarely been published in neonates and infants, with only 15 cases reported in the literature.2–8 The location of this infection is the scalp in all but three of the 15 cases, and it is worth noting that all patients were born by vaginal delivery, indicating vertical transmission as the most plausible mechanism, as occurs with other viruses such as herpes or the human papilloma virus. Berbegal-DeGracia et al., in their review of published cases, indicate that the use of instruments which may damage the skin during delivery could have an impact on the infection, as well as the greater skull diameter of the child or longer deliveries, such as those of first-time mothers.2
Histology is used for diagnosis of this infection, with basophilic inclusion bodies in epidermal keratinocytes being very characteristic, although, generally, when typical lesions in the form of pinkish umbilical papules with a keratotic centre in older children or young adults are present, it is not necessary to perform a biopsy. There are various treatments. Most of them are mechanical by means of scraping or squeezing the lesions. In recent years, products such as the one used in our case which irritate the lesions and stimulate the inflammatory response to eliminate the virus have been developed.
In conclusion, we presented a case in which both the symptoms and the histology are unique. The plaque presentation that we saw in this girl is very rare. An image like this was not found in the cases published on neonates and, although it has been reported beforehand,9 there are few cases of molluscum infection with only follicular involvement such as that which was observed in our patient, as massive or more extensive cases are typical of immunosuppressed patients. Knowledge of this atypical presentation is very helpful in order to carry out an early and visual diagnosis in these patients. In addition, knowing that molluscum contagiosum infection may have vertical transmission, as occurs with the papilloma virus or the herpes virus, may urge professionals to treat the mother during pregnancy to prevent contagion.
Conflicts of interestThe authors declare that they have no conflicts of interest.
Please cite this article as: Prieto-Torres L, Sanchez-Bernal J, Felipo F, Ara-Martín M. Placa verrugosa de crecimiento progresivo en cuero cabelludo de lactante de 3 meses. Enferm Infecc Microbiol Clin. 2018;36:384–385.