A 68-year-old male attended the ophthalmology office for redness and pain in the right eye of years of evolution, which had been getting worse in the last few months despite treatment prescribed by various ophthalmologists consisting of topical application of autologous serum, cyclosporine, prednisolone, moxifloxacin and tobramycin.
In the patient's medical history, there was no reference to toxic habits, arterial hypertension, diabetes mellitus or other systemic diseases. Regarding his ophthalmological background, the patient underwent a cornea transplant in that eye 18 years ago and required a new transplant 3 years ago due to the failure of the first one. Likewise, he required surgery on the upper eyelid of the right eye due to distichiasis. Various eye drops were used chronically (moxifloxacin, fluorometholone, dorzolamide and timolol).
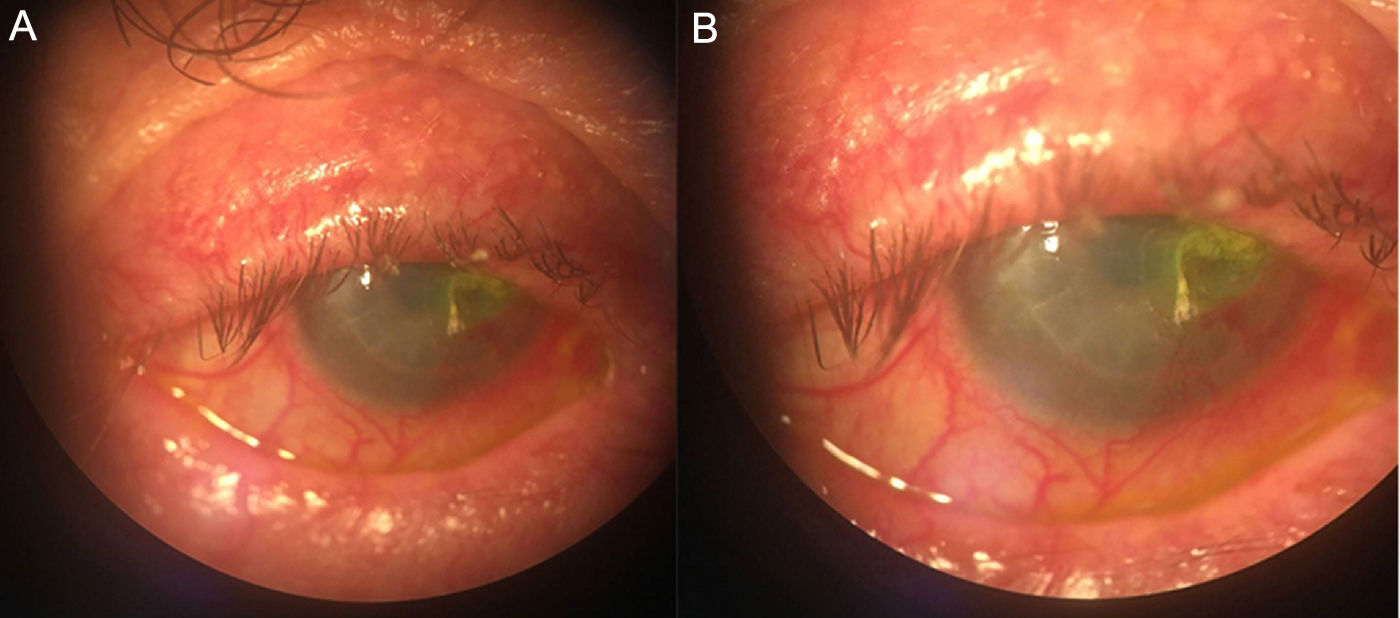
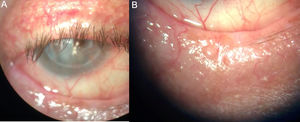
In the first examination (Fig. 1) he presented with palpebral telangiectasia, oily secretions in orifices of Meibomian glands, patchy distichiasic or absent lashes, together with secretions at the base of the same. At the level of the eyeball, there was symblepharon of the inferior conjunctiva, mixed hyperaemia and cornea with opaque, vascularised transplantation and with a corneal ulcer without signs of associated infectious infiltration. The left eye, unlike the right, presented with mild blepharitis, without signs of ocular inflammation.
Given these findings, the patient was diagnosed with ocular rosacea, which causes severe blepharitis and corneal thinning, beginning treatment with oral doxycycline, 0.5% erythromycin ointment, intense ocular lubrication and daily eyelid hygiene measures. Likewise, ocular lubrication and daily eyelid hygiene were recommended in his left eye.
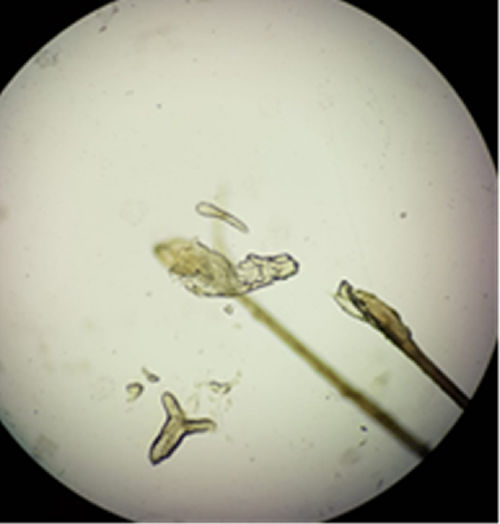
After 4 weeks of treatment, there was no improvement. Swabs were taken from the skin of the eyelids and 6 eyelashes were taken for microbiological study. Using PCR,1 6150copies/ml of Demodex folliculorum suspension were detected, as well as visualised on the eyelashes(Fig. 2).
EvolutionAfter confirming demodicosis, specific antiparasitic treatment was prescribed, which consisted of oral ivermectin 6mg, one tablet morning and night on the same day, repeating the same dose one week later. Eyelid hygiene with neutral pH shampoo followed by the application of 50% tea tree oil twice daily for 4 weeks was recommended and 0.5% erythromycin ointment was also prescribed at night for 4 weeks.
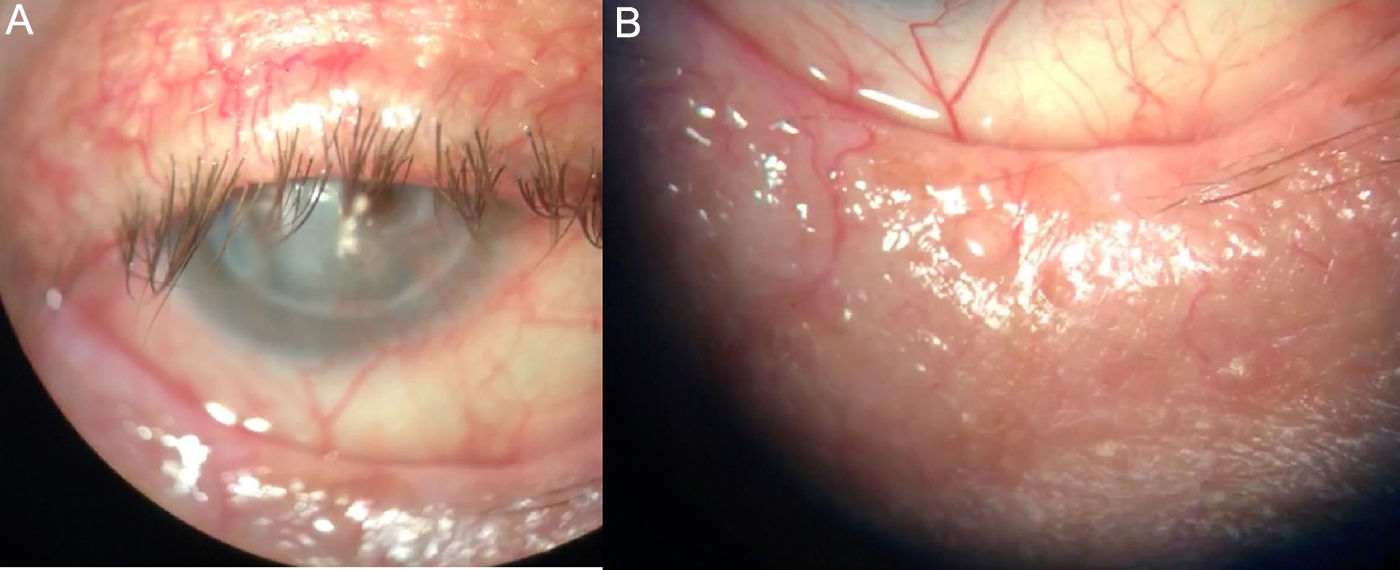
In the follow-up after 2 weeks of treatment the patient showed a clear improvement, with less seborrhoeic secretion in the orifices of the Meibomian glands and absence of crust on the eyelashes (Fig. 3). Likewise, there was an absence of ocular redness and corneal oedema, although there was a residual descemetocele that later required a conjunctival flap. The same treatment was continued as a result of the clinical improvement and there was microbiological confirmation of its effectiveness after repeating the same sample taking with swabs and direct visualisation with microscopy, both cases showing negative.
After completing the 4 weeks of treatment, the patient was asymptomatic and showed no ocular redness. Palpebral hygiene was maintained twice a day with neutral pH shampoo, applying tea tree oil once a week for 4 more weeks.
CommentsD. folliculorum is a parasite of the mite family that normally lives in the follicles of the eyelashes.2 It is believed that most of the time it coexists with the host in a saprophytic way, being more prevalent in older age groups.3 However, it has occasionally been linked to skin and eye conditions such as rosacea and chronic blepharitis.4,5 Although the relationship of anterior and mixed chronic blepharitis with the parasite D. folliculorum is sufficiently documented in the literature,4–6 it is not usually considered a priori in a first clinical diagnosis, due to the high frequency of bacterial superinfections. This parasitic infestation should be suspected in the event that a patient does not respond to conventional treatments (eyelid hygiene measures, anti-inflammatories and antibiotics).7–9 For this reason, treatment sometimes fails and blepharitis becomes chronic, considerably reducing the quality of life of the patient due to constant discomfort.10 Therefore, in cases of chronic blepharitis, the possibility of D. folliculorum as an aetiological agent, which would be easily detectable with a simple eyelash sample or PCR swab, should always be considered. Being able to establish specific treatment with ivermectin considerably increases the chances of therapeutic success. Although some studies have shown that the association of ivermectin with metronidazole has been superior to ivermectin alone,11 in the present case it was not used because there was previous treated with doxycycline and a favourable evolution along with microbiological findings were observed, so the use of metronidazole was not considered necessary.
Please cite this article as: Iglesias-Martín J, Tenorio-Abreu A, Rodríguez-Molins E, Jiménez Alcántara M. Blefaritis crónica grave. Evolución tórpida de varios años. Enferm Infecc Microbiol Clin. 2019;37:410–412.