The genus Prototheca are algae without chlorophyll, and are found ubiquitously in environmental sources such as plants, waters and animals.1 The species most commonly isolated is Prototheca wickerhamii.
P. wickerhamii rarely causes infections in humans. Infections have been reported mainly in nails,2 skin and subcutaneous tissues,3 although cases of peritonitis4 and meningitis5 have also been described. They particularly affect patients with diabetes,6 patients with HIV7 and transplant patients.8 Treatment usually involves a medical and surgical approach,2 but debate surrounds the drug treatment. There are no published prospective clinical studies comparing specific treatments for protothecosis and, although various regimens have been tried, there has been no consistency in clinical responses. The most commonly used antifungals are azoles, itraconazole and amphotericin B in particular, with amphotericin B displaying the best activity.9 The Prototheca spp. cell wall is rich in ergosterol, and it is thought that the efficacy of these antifungals lies in their ability to inhibit ergosterol.9,10 However, no cut-off points have been established for the interpretation of in vitro sensitivity. As the minimum inhibitory concentration (MIC) determination tests are not always reproducible, and the results are not always correlated with clinical success, performing sensitivity tests is only recommended in cases of treatment failure, not routinely.1
We present the case of a 57-year-old male patient with a history of hypertension, dyslipidaemia, obesity, venous insufficiency, lymphoedema and allergy to mites, under follow-up since 2014 due to repeated outbreaks of stasis eczema in the lower limbs, where he has also had venous ulcers for years which have been become infected on multiple occasions. The patient had suffered severe flare-ups of atopic dermatitis in its atopic context which at the time of presentation were well controlled with azathioprine 100mg/day, after previously requiring repeated courses of oral and topical corticosteroids. He attended the clinic with a 2–3 week history of a slightly pruritic lesion on the back of his right hand. Examination revealed an annular-shaped, scaly plaque with a maximum diameter of about 3cm, with centrifugal growth, central clearance with erythematous edges, and peripheral pustules. It did not give the impression of a staphylococcal infection as it lacked suppuration or characteristic impetiginised scabs. We did not consider it to be tuberculosis of the skin, as it does not present in this way and is usually accompanied by lymphadenopathy (moreover QuantiFERON® and Mantoux were negative). We also ruled out atypical mycobacteriosis, as it develops with nodular lesions or erythematous-desquamative plaques that grow progressively without central clearance. Coccidioidomycosis was excluded as it consists of an ulcerated, indurated nodule, often accompanied by secondary nodules. Sporotrichosis and leishmaniasis were ruled out due to no history of trauma or being stung respectively. The clinical diagnosis of non-inflammatory dermatomycosis was based on the shape of the lesion and its recent onset. This circinate shape is a result of the depletion of keratin from the centre of the lesion and its peripheral spread. Once the differential diagnosis was made, flakes were taken for mycological culture and we prescribed terbinafine 250mg/24h and ciclopirox cream every 12h for one month.
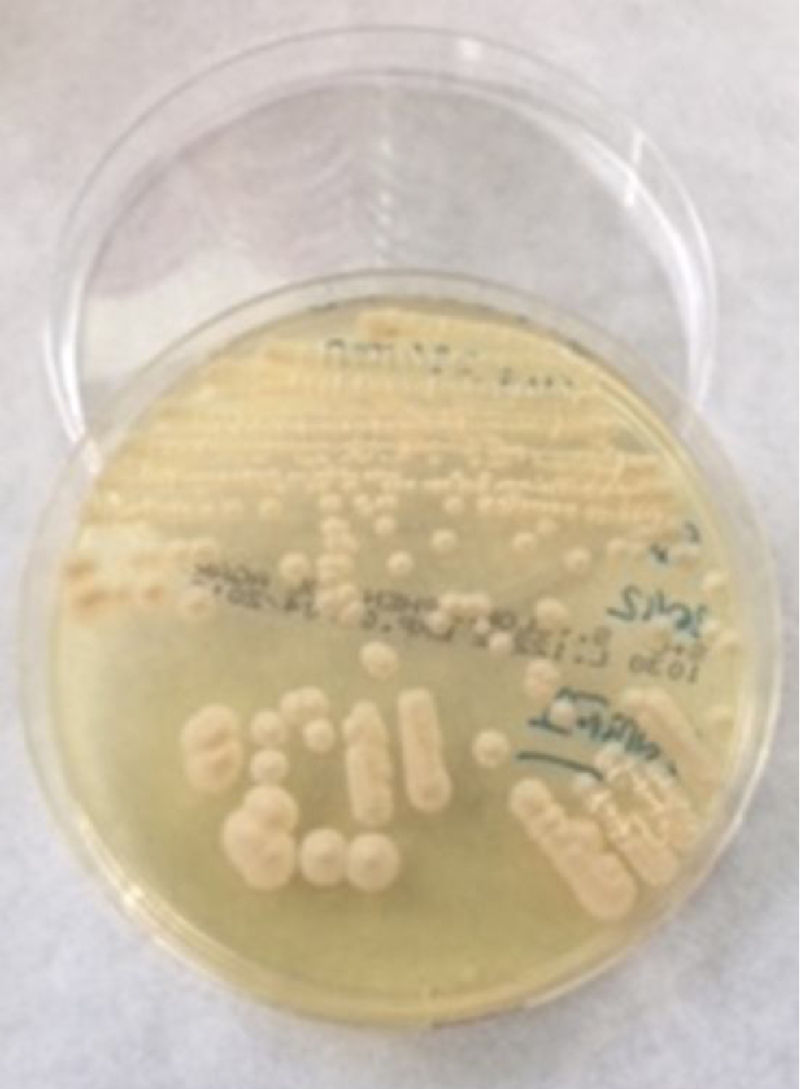
The flakes were seeded on Sabouraud-chloramphenicol agar (bioMérieux) and on a home-made medium of malt extract agar and incubated at 30°C for 30 days. Three weeks later rough, beige colonies with a yeast-like appearance were observed (Fig. 1). They were identified by VITEK® 2 System (bioMérieux) and MALDI-TOF VITEK® MS (bioMérieux) with both obtaining the result of P. wickerhamii. One month later there were no signs of lesion when the patient attended for follow-up. Although the treatment prescribed for this case was not that of choice (due to the treatment with lipid-lowering agents and azathioprine, azoles were avoided to reduce the risk of interactions), the tinea was eradicated. Like azoles or amphotericin B, terbinafine causes a decrease in ergosterol; in this case, by inhibiting squalene epoxidase in the cell membrane.10
The lack of literature and of cut-off points for the sensitivity of antifungals underline the need for further studies to investigate treatments for this type of infection.
The Prototheca species cause a wide range of infections in humans. These infections can occur in both immunocompetent and immunosuppressed patients, although the most severe and widespread infections usually occur in immunocompromised individuals. In view of their similar appearance to yeasts in routine media, but with very different implications for prognosis and treatment, both clinicians and microbiologists have to be aware of these organisms and work together to ensure that they are correctly diagnosed and the proper treatment provided.
Please cite this article as: Sante L, Cuervo M, de Andrés del Rosario A, Lecuona M. Onicomicosis por alga sin clorofila. Enferm Infecc Microbiol Clin. 2019;37:278–279.