Haemophilus influenzae is a Gram-negative coccobacillus first described by Pfeiffer in 1892.1 It may be encapsulated, with 6 antigenically different types (a–f), or non-encapsulated. H. influenzae type b (Hib) was responsible for 90–95% of cases of invasive disease in children under 5 years of age, until the introduction of the conjugate vaccine,2,3 being rare in adults.
We present the case of a 63-year-old woman, with no prior history of note or contact with children, who attended the emergency department due to odynophagia, arthromyalgia and a dysthermic sensation for the last 48–72h. Notable findings on physical examination were: fever (38°C), tachycardia (130bpm) and tachypnoea (20bpm); exanthema and petechiae on the palate; pharyngeal hyperaemia; lateral cervical lymphadenopathy; and hypophonesis at the base of the right lung. Complementary tests revealed: acute renal failure (Cr 2.4mg/dl), leukopenia (3270 leukocytes), coagulopathy (PT 1.41), high CRP (48.8mg/dl) and procalcitonin (19.6ng/ml), acute partial respiratory failure (pO2 49mmHg, pCO2 31mmHg), and right pleural effusion. A diagnosis of severe sepsis was made, blood cultures (BCs) were collected, empirical antibiotic therapy was started with imipenem and the patient was admitted. Once the patient was on the unit, an ear, nose and throat examination was performed; this examination was normal. After 15h, Hib (resistant to ampicillin and susceptible to cefotaxime, azithromycin and ciprofloxacin) was isolated in her BCs, and her antibiotic therapy was adjusted to ceftriaxone. A diagnostic thoracocentesis was performed which yielded purulent fluid. Subsequently, Hib was isolated in this fluid too, and a chest tube was placed. Thereafter, the patient had arthritis in her right ankle. Arthrocentesis was performed and real-time PCR was used to detect Hib in the fluid extracted. The patient received intravenous antibiotic therapy for 2 weeks and continued with oral ciprofloxacin until she had completed 4 weeks of treatment, with resolution of her signs and symptoms and normalisation of her renal function and inflammatory parameters. An immunity study was performed. A notable finding was an IgG level of 469mg/dl (751–1560mg/dl). In subsequent tests, IgG levels were within normal limits (878 and 848mg/dl, respectively). Hib-specific antibodies (1.23mg/dl) were found to be above the protective value (>1mg/l). Therefore, it was not necessary to vaccinate the patient, nor were there any indications for chemoprophylaxis. Hence, this was a case of bacteraemia, empyema and septic arthritis caused by Hib in an adult patient with no risk factors.4
We report this case due to the rarity of invasive disease caused by Hib in an adult without comorbidity. Hib is capable of colonising the respiratory tract for long periods of time and reaching the bloodstream. This would lead to bacteraemia and metastatic infection, thanks to its polysaccharide capsule composed of polyribitol phosphate.1 Asymptomatic carrier rates vary by study from 0% to 9%, and are much higher in children.2 The epidemiological characteristics of invasive disease due to H. influenzae have changed since the introduction in 1989 of the conjugate vaccine against Hib in children under 5 years of age. Many studies have reported a 99% decrease in incidence in this age group after the introduction of the vaccine. In adults, the epidemiological situation is different. A study conducted in Illinois from 1996 to 2004 on changes in the epidemiology of invasive disease due to H. influenzae showed an increase in the incidence in adults, especially those over 65 years of age.5 This increase in incidence was due to non-typeable strains in many studies.3,5–9 In addition, it has been observed that the majority of Hib infections occur in adults with comorbidities. This suggests the need to execute strategies to protect this most vulnerable group.8 The risk factors for acquiring the disease include: age, complement deficiency, hypogammaglobulinaemia, sickle cell anaemia, HIV, COPD, smoking, alcoholism, overcrowding and low immunisation.4
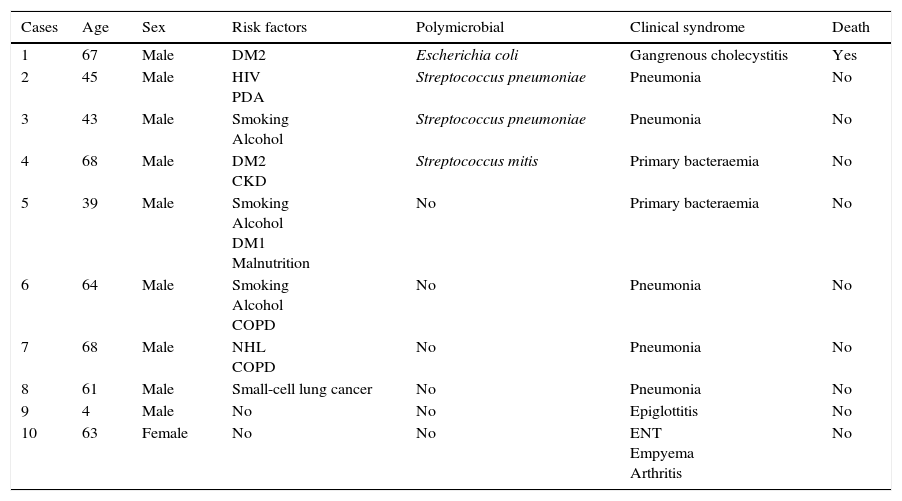
We identified 10 cases of invasive Hib disease at our centre between 2005 and 2015. Their characteristics are shown in Table 1. Save for one case of epiglottitis in a child and the case presented here, all were in adults (mean age 57 years, 100% males) with at least one of the above-mentioned comorbidities.
Cases of invasive Hib disease at Complexo Hospitalario Universitario de A Coruña from 2005 to 2015.
| Cases | Age | Sex | Risk factors | Polymicrobial | Clinical syndrome | Death |
|---|---|---|---|---|---|---|
| 1 | 67 | Male | DM2 | Escherichia coli | Gangrenous cholecystitis | Yes |
| 2 | 45 | Male | HIV PDA | Streptococcus pneumoniae | Pneumonia | No |
| 3 | 43 | Male | Smoking Alcohol | Streptococcus pneumoniae | Pneumonia | No |
| 4 | 68 | Male | DM2 CKD | Streptococcus mitis | Primary bacteraemia | No |
| 5 | 39 | Male | Smoking Alcohol DM1 Malnutrition | No | Primary bacteraemia | No |
| 6 | 64 | Male | Smoking Alcohol COPD | No | Pneumonia | No |
| 7 | 68 | Male | NHL COPD | No | Pneumonia | No |
| 8 | 61 | Male | Small-cell lung cancer | No | Pneumonia | No |
| 9 | 4 | Male | No | No | Epiglottitis | No |
| 10 | 63 | Female | No | No | ENT Empyema Arthritis | No |
CKD, chronic kidney disease; COPD, chronic obstructive pulmonary disease; DM, diabetes mellitus; ENT, signs and symptoms in the ear, nose and throat area; HIV, human immunodeficiency virus; NHL, non-Hodgkin lymphoma; PDA, parenteral drug addiction.
Therefore, it seems necessary to build upon studies on this disease in the adult population, and to take it into account in the differential diagnosis for early antibiotic treatment, since mortality rates in this group are far from negligible (up to 20%).5–7
Please cite this article as: Fuente Cosío S, Castelo Corral L, Rodríguez Mayo M, Llinares Mondejar P. Enfermedad invasiva por Haemophilus influenzae serotipo b en el adulto. Enferm Infecc Microbiol Clin. 2017;35:325–326.