A 10-year-old male with no prior disease history of interest was referred to a dermatology outpatient clinic to assess a lesion on his right knee which had developed 4 months earlier and which was not associated with any non-cutaneous signs or symptoms. The problem began after the boy fell on the school playground and suffered a skin abrasion followed by the onset of confluent papules forming the current lesion. A physical examination revealed an oval-shaped erythematous plaque spanning 6cm, purplish-red in colour, with multiple papules with keratotic crusting exhibiting a granulomatous appearance and no exudate or purulent discharge (Fig. 1). Initially, it was diagnosed as a foreign body reaction and the boy was prescribed very high-strength topical corticosteroids; however, no clinical improvement was seen. The patient's mother was questioned again. She reported that the boy had a tortoise at home and had been bathing with it in the months before his fall. She also reported that he was often in pools since he was taking swimming classes. With a skin infection being suspected, a punch biopsy was done for histology and culture of bacteria, mycobacteria and fungi.
Clinical courseHistology showed foci of abscessification with epithelioid and suppurative granulomas occupying the entire dermis. Giemsa, PAS and Ziehl–Neelsen stains were negative on tissue sampling.
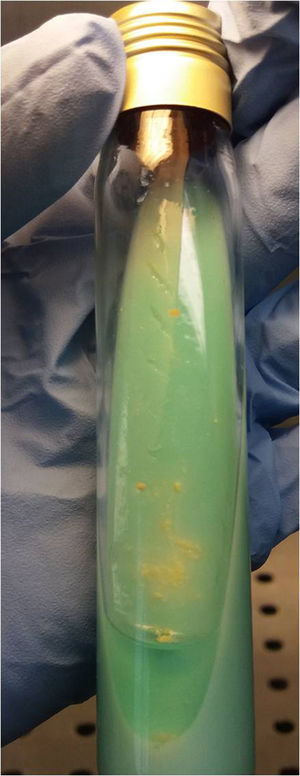
After 10 days of incubation in a liquid culture medium (BACTEC MGIT 960) and after 18 days of incubation in a Löwenstein solid medium, both at 37°C and at room temperature, a mycobacterium grew that was identified as Mycobacterium marinum. This identification was made due to its capacity for acquiring colour on being exposed to light (i.e. its photochromogenicity) (Fig. 2) and by exclusion upon performing the molecular hybridisation technique (Hain Lifescience). It was specifically identified as M. marinum/M. ulcerans (GenoType CM version) and as Mycobacterium spp. (GenoType AS version). Thus the diagnosis of non-tuberculous mycobacteriosis due to overinfection of the primary wound was confirmed.
Treatment was started with clarithromycin (500mg/12h), and resolution was achieved after 3 months of treatment. Treatment was maintained for 2 months following clinical resolution.
CommentsM. marinum belongs to the group of photochromogenic, slow-growing non-tuberculous mycobacteria. Generally, in culture media it requires 14–21 days to proliferate at temperatures of 30–32°C.1 Its primary reservoir is seawater or stagnant water, and its primary risk factors are activities related to fish as well as contact with contaminated water, both fresh water and salt water from aquariums, water tanks and pools.2 For this reason, infection caused by this microorganism is called “swimming pool granuloma” or “aquarium granuloma”. In order for infection to develop following exposure, a point of entry is needed. Typical points of entry are small sites of erosion or trauma that sometimes go unnoticed.
Clinically, this infection develops following a period of 2–3 weeks of incubation, with generally solitary lesions predominantly on the limbs in the form of papules and pustules, granulomatous plaques and subcutaneous nodules with a tendency to fistulise or ulcerate. Approximately 20–40% have a sporotrichoid distribution pattern, especially when contagion is associated with handling aquariums.3 Disseminated and extracutaneous signs and symptoms are rare.4 Although it may cause local synovitis and osteomyelitis, these are uncommon complications that require a deep point of entry.5
Diagnosis requires a strong clinical suspicion as it necessitates special culture media (Löwenstein, Middlebrook or MGIT), or detection through the polymerase chain reaction technique and sequencing from the affected tissue. Stains used to detect acid/alcohol-fast bacilli (Ziehl–Neelsen, auramine–rhodamine) are useful for confirming the diagnosis of mycobacteriosis, but do not distinguish between species of mycobacteria. Differential diagnosis is done primarily to distinguish this infection from any other infection due to non-tuberculous mycobacteria, leishmaniasis, sporotrichosis, deep mycosis, cutaneous tuberculosis or granuloma associated with a foreign body.
The treatment of choice is empirical systemic antibiotic therapy. An antibiogram is only recommended in cases of therapeutic failure. In cases with single lesions, surgical removal may be a good therapeutic option. The most commonly used drugs are minocycline, doxycycline, clarithromycin, ethambutol, rifampin and co-trimoxazole.6 In general, clarithromycin is the first-line drug of choice.7 The recommended length of treatment is 6 months or at least 2 months after clinical resolution.8 In cases with osteotendinous impairment it is recommended that at least 2 drugs be combined, generally clarithromycin plus rifampin or ethambutol. In many cases, surgical debridement and a longer antibiotic treatment time are required.
Please cite this article as: Sahuquillo-Torralba A, Calle-Andrino A, Gil-Brusola A, Évole-Buselli M. Placa granulomatosa en la rodilla derecha de un niño de 10 años de edad. Enferm Infecc Microbiol Clin. 2019;37:58–59.