Dermatophytosis caused by Nannizzia gypsea are considered rare. The clinical picture is indistinguishable from that produced by other dermatophytes, but, being this a geophilic fungus, it can cause more inflammatory disease.
MethodsRetrospective study. Patients with positive culture for N. gypsea observed at the Dermatological Institute of Jalisco "Dr. José Barba Rubio", from 2001 to 2023, were included. Frequency, sex, age, evolution, and clinical variant were investigated. We compared the findings between the pediatric versus adult population. Descriptive and inferential statistics were used.
ResultsOver 23 years, 155 patients were diagnosed (6.7 cases per year). Female sex predominated (53.5%). The median age was 9 years (minimum 1year and maximum 85 years), the more affected age group was 1–10 years (54.2%). The median time of evolution was 30 days (minimum one day and maximum three years), and 74.8% had an evolution ≤30 days. Tinea capitis predominated in pediatric patients (41.0%, p<0.01) whereas tinea corporis predominated in adults (72.7%, p<0.01). Inflammatory tinea was more prevalent in the pediatric population (21.0% vs. 3.6%, p<0.01).
ConclusionThe ability of Nannizzia gypsea to cause inflammatory tinea was observed primarily in pediatric patients. Since there is no clinical data to suspect this fungus, it will always be necessary to carry out a mycological study to identify the species and to implement the appropriate treatment.
Las dermatofitosis causadas por Nannizzia gypsea son poco frecuentes. El cuadro clínico es indistinguible del producido por otros dermatofitos, pero, por ser un hongo geofílico, puede ocasionar infecciones más inflamatorias.
MétodosEstudio retrospectivo. Se incluyeron pacientes con cultivo positivo de N. gypsea observados en el Instituto Dermatológico de Jalisco “Dr. José Barba Rubio”, del 2001al 2023. Se investigaron la frecuencia, el sexo, la edad, el tiempo de evolución y la variante clínica. Se compararon los hallazgos en población pediátrica versus adulta. Utilizamos estadística descriptiva e inferencial.
ResultadosEn 23 años se diagnosticaron 155 pacientes (6,7 casos por año). Predominó el sexo femenino (53,5 %), la mediana de edad fue 9 años (mínima 1 año y máxima 85 años), el grupo etario más afectado fue el de 1 a 10 años (54,2 %), la mediana del tiempo de evolución fue 30 días (mínima un día y máxima tres años) y el 74,8% tenían una evolución ≤30 días. En los pacientes pediátricos predominó la tiña de la cabeza (41,0%, p<0,01) y en los adultos la tiña del cuerpo (72,7%, p<0,01). La tiña inflamatoria fue más prevalente en la población pediátrica (21,0% vs. 3,6%, p<0,01).
ConclusiónLa capacidad de Nannizzia gypsea para causar tiñas inflamatorias se observó principalmente en los pacientes pediátricos. Dado que clínicamente no hay datos para sospechar de este hongo, siempre será necesario realizar un estudio micológico para identificar la especie e implementar el tratamiento adecuado.
Dermatophytoses, also known as tinea and ringworm, are infections caused by dermatophyte fungi, which affect 20%–25% of the world's population.1 Dermatophytes include 59 species distributed in nine genera, of which the main ones responsible for causing disease in humans are Trichophyton, Epidermophyton, Microsporum and Nannizzia.2,3 According to the latest classification of dermatophytes, proposed in 2017, the genus Nannizzia includes thirteen species, with N. gypsea being the most important in the medical field.4–6
Human infections caused by Nannizzia spp. are opportunistic, result from contact with contaminated soil, and are rare.7,8 Its prevalence among dermatophytoses varies from less than 1% in Korea9 to 6.8% in Italy.10 As such, most of the available evidence is based on case reports or series where all superficial mycoses are studied in general terms.
The importance of this study lies not only in the rarity of infections caused by N. gypsea, but also in the fact that, being a geophilic fungus, clinically it tends to produce more inflammatory infections. This causes greater morbidity and can lead the primary care physician to suspect eczema or impetigo and so erroneously prescribe corticosteroid or antibiotic therapy.11–16
Our aim was to describe the clinical-epidemiological characteristics of 155 cases of dermatophytosis caused by N. gypsea in western Mexico and to compare the condition in paediatric subjects and adults.
MethodsThis was a retrospective study conducted at the Instituto Dermatológico de Jalisco «Dr. José Barba Rubio» ["Dr José Barba Rubio" Jalisco Dermatological Institute], a tertiary care institution, located in western Mexico. Information was sourced from the electronic medical records and the Mycology Laboratory files. Patients with positive N. gypsea culture identified from 1 January 2001 to 31 December 2023 were included.
The same mycology method was used throughout the study. Samples were obtained from lesions on hairless skin or the nails and, when the condition affected the scalp, from broken hairs, which were cultured on simple and modified Sabouraud dextrose agar (addition of chloramphenicol and/or cicloheximide) at temperatures of 25°C to 28°C. Cultures were considered positive if they developed in an average time of eight to 10 days, were characterised macroscopically by powdery-looking colonies, initially white in colour, later turning beige, without pigment on the reverse, and microscopically by sparse thin, septate mycelia with a large quantity of macroaleurioconidia approximately 50 to 120 μm long by 10 to 20 μm wide, spindle-shaped or like tree leaves with a thin membrane, which sometimes had small spicules and formed four to six septa.17
The frequency and time since onset of the disease and the age and gender of the patients was determined. Infections were classified as superficial (scalp, facial, body, groin, hand, foot and nail ringworm) and inflammatory (kerion celsi, favus and trichophytic granuloma).
The statistical program IBM SPSS Statistics version 20.0 (IBM® Company, United States) was used to analyse the results. The population distribution was determined using the Kolmogorov-Smirnov test. Descriptive statistics were used through measures of central tendency (median) and dispersion (ranges). To compare qualitative variables, inferential statistics in the form of the chi-square test or Fisher's exact test were used, as appropriate. The Mann–Whitney U test was used to analyse quantitative variables. The difference was considered statistically significant if p<0.05.
This research was approved by the institution's Independent Ethics Committee (registration 2022-12-CEIIDJ-21).
ResultsOver the 23 years of the study, 24,449 cases of dermatophytosis were diagnosed, 155 (0.63%) of which were dermatophytoses caused by N. gypsea, with a rate of 6.7 cases per year (minimum 1 and maximum 15). Fig. 1 shows the macroscopic and microscopic characteristics of the culture.
Females predominated, with 83 cases (53.5%). The median age was nine years old (minimum one year and maximum 85). The most affected age group was the 1-to-10-year-olds, with 84 cases (54.2%), followed by the 11-to-20-year-olds, with 19 cases (12.3%), and 21-to-30-year-olds, with 16 cases (10.3%); the remaining 36 cases (23.2%) were patients aged 31 or over.
In terms of occupation, the three most common were: being a student, 88 cases (56.8%); homemakers, 25 cases (16.1%); and infants, 16 cases (10.3%). In total, 26 (16.8%) of the patients had variable occupations and two (1.3%) worked in agriculture.
The median time since onset was 30 days (minimum one day and maximum three years). The condition was acute (<15 days) in 47 patients (30.3%), subacute (15–30 days) in 69 (44.5%) and chronic (>30 days) in 39 (25.2%).
Dermatophytosis was classified as superficial in 132 cases (85.2%) and inflammatory in 23 (14.8%). In the first group, tinea corporis predominated, with 64 cases (48.5%), and in the second, kerion celsi, with 19 (82.6%) (Table 1).
Clinical classification of dermatophytosis caused by Nannizzia gypsea (n=155).
| Type of skin infection | n | % |
|---|---|---|
| Superficial (tinea infections)n=132 | ||
| Of the head | 23 | 17.4 |
| Of the face | 34 | 25.7 |
| Of the body | 64 | 48.5 |
| Of the groin | 1 | 0.8 |
| Of the hand | 2 | 1.5 |
| Of the foot | 5 | 3.8 |
| Of the nails | 3 | 2.3 |
| Inflammatoryn=23 | ||
| Kerion celsi | 19 | 82.6 |
| Trichophytic granulomaa | 4 | 17.4 |
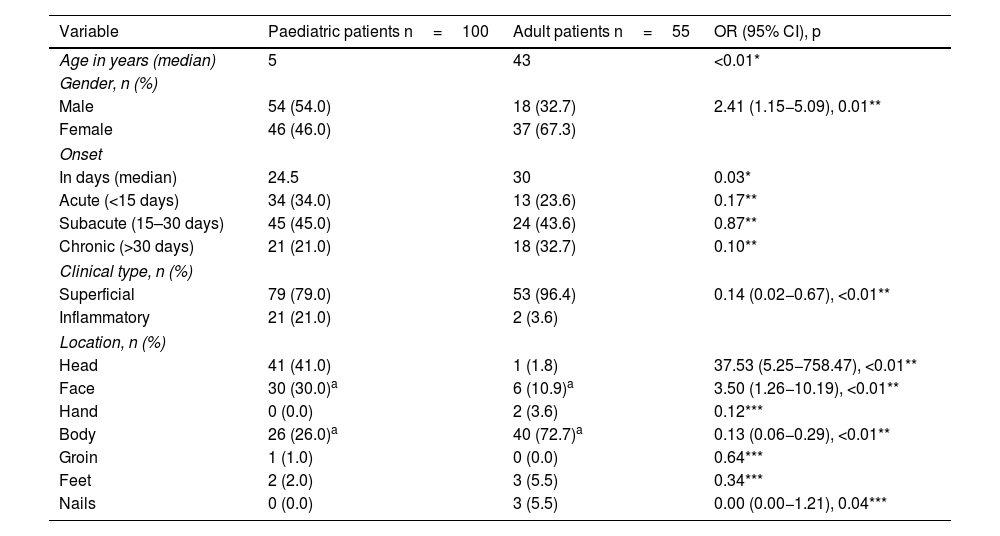
We compared the 100 patients (64.5%) of paediatric age and the 55 (35.5%) in the adult age group. Inflammatory ringworm was more common in the paediatric age group, with 21 subjects (21.0%), while there were just two cases among the adults (3.6%) (p<0.01). In the paediatric group, tinea capitis predominated, with 41 cases (41.0%), compared to one case in adults (1.8%) (p<0.01). Tinea corporis was more common in the adult group, with 40 cases (72.7%), compared to 26 among the paediatric patients (26.0%) (p<0.01) (Table 2 and Fig. 2).
Comparison of clinical-epidemiological findings of paediatric patients versus adult patients with dermatophytosis caused by Nannizzia gypsea (n=155).
| Variable | Paediatric patients n=100 | Adult patients n=55 | OR (95% CI), p |
|---|---|---|---|
| Age in years (median) | 5 | 43 | <0.01* |
| Gender, n (%) | |||
| Male | 54 (54.0) | 18 (32.7) | 2.41 (1.15−5.09), 0.01** |
| Female | 46 (46.0) | 37 (67.3) | |
| Onset | |||
| In days (median) | 24.5 | 30 | 0.03* |
| Acute (<15 days) | 34 (34.0) | 13 (23.6) | 0.17** |
| Subacute (15–30 days) | 45 (45.0) | 24 (43.6) | 0.87** |
| Chronic (>30 days) | 21 (21.0) | 18 (32.7) | 0.10** |
| Clinical type, n (%) | |||
| Superficial | 79 (79.0) | 53 (96.4) | 0.14 (0.02−0.67), <0.01** |
| Inflammatory | 21 (21.0) | 2 (3.6) | |
| Location, n (%) | |||
| Head | 41 (41.0) | 1 (1.8) | 37.53 (5.25−758.47), <0.01** |
| Face | 30 (30.0)a | 6 (10.9)a | 3.50 (1.26−10.19), <0.01** |
| Hand | 0 (0.0) | 2 (3.6) | 0.12*** |
| Body | 26 (26.0)a | 40 (72.7)a | 0.13 (0.06−0.29), <0.01** |
| Groin | 1 (1.0) | 0 (0.0) | 0.64*** |
| Feet | 2 (2.0) | 3 (5.5) | 0.34*** |
| Nails | 0 (0.0) | 3 (5.5) | 0.00 (0.00−1.21), 0.04*** |
CI: confidence interval; OR: odds ratio.
In this study, carried out in subjects from western Mexico, we found 155 cases of skin infections caused by N. gypsea, with an average of 6.7 cases per year, a lower rate than the 14 patients per year reported in Slovenia,13 but higher than that recorded in South Korea, with 5.21 cases per year,11 and south-eastern Mexico, with 4.57 cases per year.12 In any event, the number of cases confirms that, of the genera of fungi capable of causing disease in humans, N. gypsea is the least common, especially compared to Trichophyton rubrum, the agent responsible for 80%–90% of all dermatophytoses worldwide, with a rate in Mexico of 227 cases per year.18–21
In the overall sample, 53.5% of cases were female. Females were also more likely to be affected in the studies by Lee et al.11 on South Korean patients and Torres-Guerrero et al.12 on Mexican patients, accounting for 52.5% and 76.5% of cases, respectively. In reality, there is no clear explanation for the predominance of this infection in females, but some authors suggest that, in general, women are more likely to seek medical attention, as they have a worse perception of their health, with greater restrictions on their activities and more symptoms than men.22 However, it is important to mention that, in our study, gender was influenced by age group, as more boys were affected than girls in the paediatric group, while in adults we found that N. gypsea infections were twice as likely to occur in females. This had already been observed in the study by Lee et al.,11 where males predominated in the 0-to-19-year age group and females in the over-20s.
Dermatophytosis caused by N. gypsea occurs mainly in children and adolescents,11 as we found in our study, where the most affected age group was the 1-to-10-year-olds, with 54.2% of cases, followed by the 11-to-20-year-olds, with 12.3%; South Korea also reported a higher number of cases in these two age groups, with prevalence rates of 31.3% and 15.2%, respectively.11 This may be due to the fact that at these ages, children and young people are involved in more outdoor activities and have a greater tendency to play on the ground, which may be contaminated by N. gypsea7,11; this is what occurred in an epidemiological outbreak of tinea corporis in 13 Colombian children between one and 15 years of age from six neighbouring families who had in common that they used a piece of waste land as a playground, where the fungus was also isolated in the soil.23 Another factor that may explain this predominance in children and adolescents is the greater cohabitation with pets. This is important, as the fungus has been found in dogs and cats, which can be asymptomatic carriers and cause soil contamination, thereby increasing the risk of infection.8,10,24,25 Nonetheless, due to the retrospective nature of our study, this is not something we were able to corroborate.
Given that the majority of our population was under the age of 20 years, it is not surprising that in terms of occupation, a majority (56.8%) were students. We would nevertheless have expected that the proportion working in agriculture would be higher, since they have more contact with the land, but it was only 1.3%. Our results are in line with those reported by Torres-Guerrero et al.12 in the other Mexican study, where students also predominated (39.1%) followed by homemakers (23.4%).
The median time since onset was 30 days, with the median in the paediatric population being statistically lower, and although there were patients with up to three years since onset, in the majority (74.8%) it was no more than 30 days. This is probably because, as dermatophytosis caused by N. gypsea is more inflammatory and so causes more symptoms,8,26 the patient is likely to need to visit the doctor sooner, especially if they are children.
Inflammatory tinea occurred in 14.8% of cases and was predominant in paediatric patients, with a protective factor for this form of infection being found in adults. Of the 23 patients with inflammatory clinical forms, kerion celsi was the most common, accounting for 82.6% of cases. In the other Mexican study, of seven reported cases of tinea capitis, 100% were kerion celsi,12 making it the most common clinical form of inflammatory dermatophytosis caused by N. gypsea. Interestingly, the remaining 17.4% of our cases with inflammatory tinea were diagnosed with trichophytic granuloma, which is usually caused by the genus Trichophyton, especially T. rubrum, which is responsible for 50% of cases, while N. gypsea is a rare aetiological agent27; in fact, in a recently-published multicentre retrospective cohort study that included 147 cases of trichophytic granuloma, only one case caused by N. gypsea was reported.28
The higher rate of inflammatory tinea is characteristic of N. gypsea.26,29 This is in contrast to infections caused by the genus Trichophyton, which are generally non-inflammatory, as in cases of tinea capitis caused by this agent.30 This is believed to be due to the enzymatic profile of N. gypsea, consisting of alkaline phosphatase, esterase, lipase, leucine arylamidase, valine arylamidase, acid phosphatase, phosphoamidase, ®-glucosidase, N-acetyl-®-glucosaminidase and 〈-mannosidase, with more intense enzymatic activity seen in some cases than that caused by Microsporum canis, another agent associated with inflammatory clinical conditions.31
Of the 155 patients included, the most common anatomical location of ringworm was on the body. Other studies also report this finding, with highly variable frequencies: 38.4% in South Korea11; 69.03% in Slovenia13; and 77.8% in Mexico.12 However, we found that location was also influenced by age group. Paediatric patients were 37.53 times more likely to suffer from tinea capitis compared to adult patients, and 3.50 times more likely to have tinea faciei. However, they had a protective factor against suffering from tinea corporis, which was significantly more prevalent in adults. We only found three cases of nail tinea, all adult patients, confirming that N. gypsea is a fungus which, unlike T. rubrum, typically affects hairless skin and scalp, and rarely presents as onychomycosis.8,10
We can conclude that N. gypsea is a fungus that tends to mainly cause disease in children, and that children also have a higher risk of developing inflammatory clinical conditions. Therefore, physicians, especially primary care physicians, paediatricians and dermatologists, should include infections caused by this agent in their differential diagnoses of inflammatory lesions, in order to avoid incorrect diagnoses and inadequate treatments. The main limitation of this study is its retrospective nature, meaning we were unable to investigate points of interest, such as the treatment prescribed and the response to it. However, it is the second largest sample reported and provides information on clinical differences between the paediatric and adult populations, which have also not previously been reported.
FundingThis study received no specific funding from public, private or non-profit organisations.