A case of premature closure of foramen ovale (PCFO) is presented. The patient was sent to the Fetal Maternal Unit after 30 weeks of gestation due to hydrops fetalis. A Doppler ultrasound performed after 34 weeks of gestation showed no interatrial flow and led to the confirmation of PCFO, associated to pleural effusion and ascitis. No evidence of hydrops, pleural effusion, ascitis, cardiac failure, cardiac defects nor chromosomal abnormalities were present in the newborn baby. Since prenatal diagnosis of PCFO is a life threatening condition, detection improves fetal and neonatal life expectancy.
Se reporta el cierre prematuro de foramen oval (CPFO) en un embarazo de 30 semanas de gestación, enviado con hidrops fetal a Unidad de Medicina Materno Fetal. A las 34 semanas se evaluó con Ultrasonido Doppler y se observó falta de flujo entre aurículas, confirmando el CPFO, presencia de derrame pleural y ascitis. Después del nacimiento, al neonato se le descartó la presencia de hidrops, derrame o ascitis, insuficiencia cardiaca, defectos cardiacos o cromosomopatía, y egresó sano. El CPFO pone en riesgo la vida. Cuando es detectado prenatalmente mejora la expectativa de vida fetal y neonatal.
The premature obstruction of the foramen ovale (PCFO) is a rare and serious clinical entity that can be associated to fetal hydrops and heart defects, and in most cases the diagnosis is postmortem and etiology is unknown. When signs of cardiac failure are present, delivery should be induced if possible.1
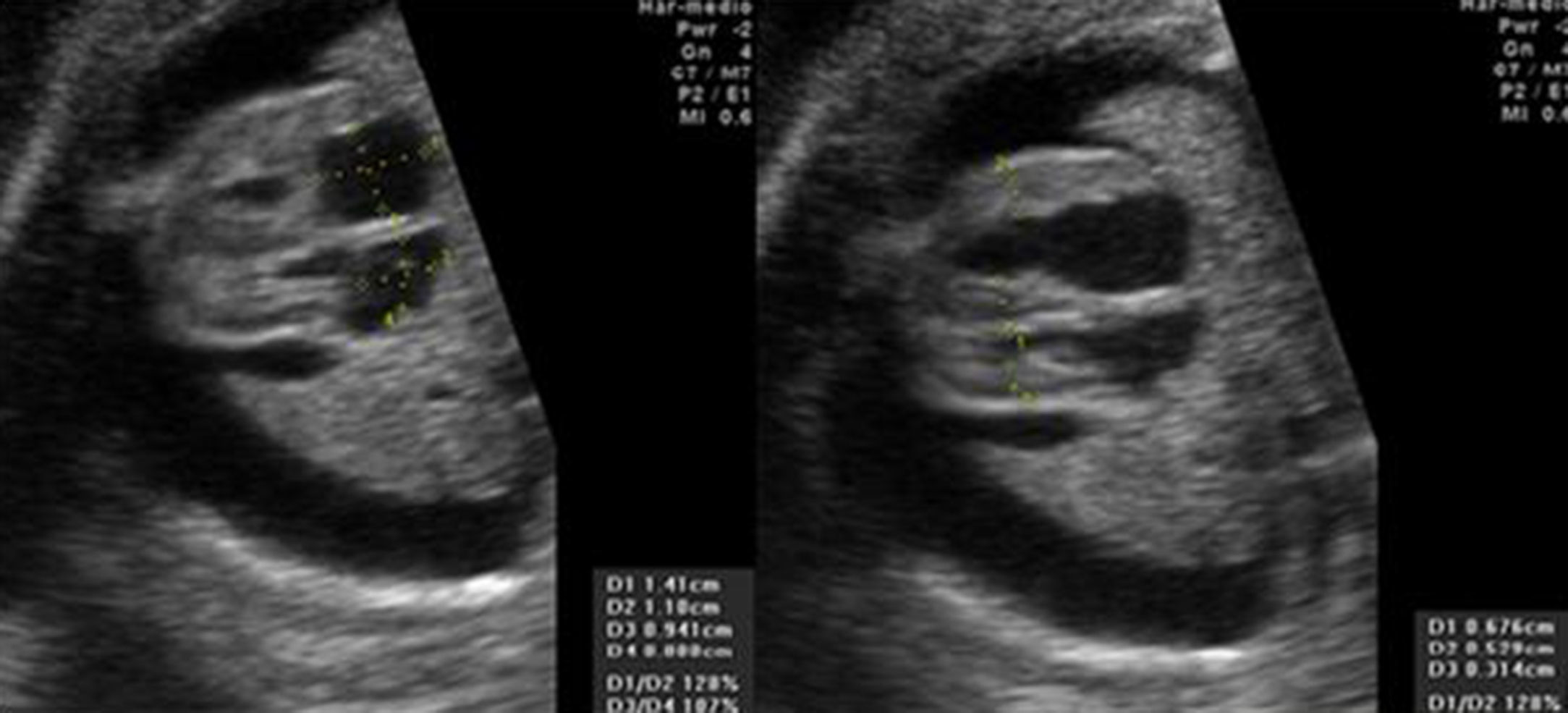
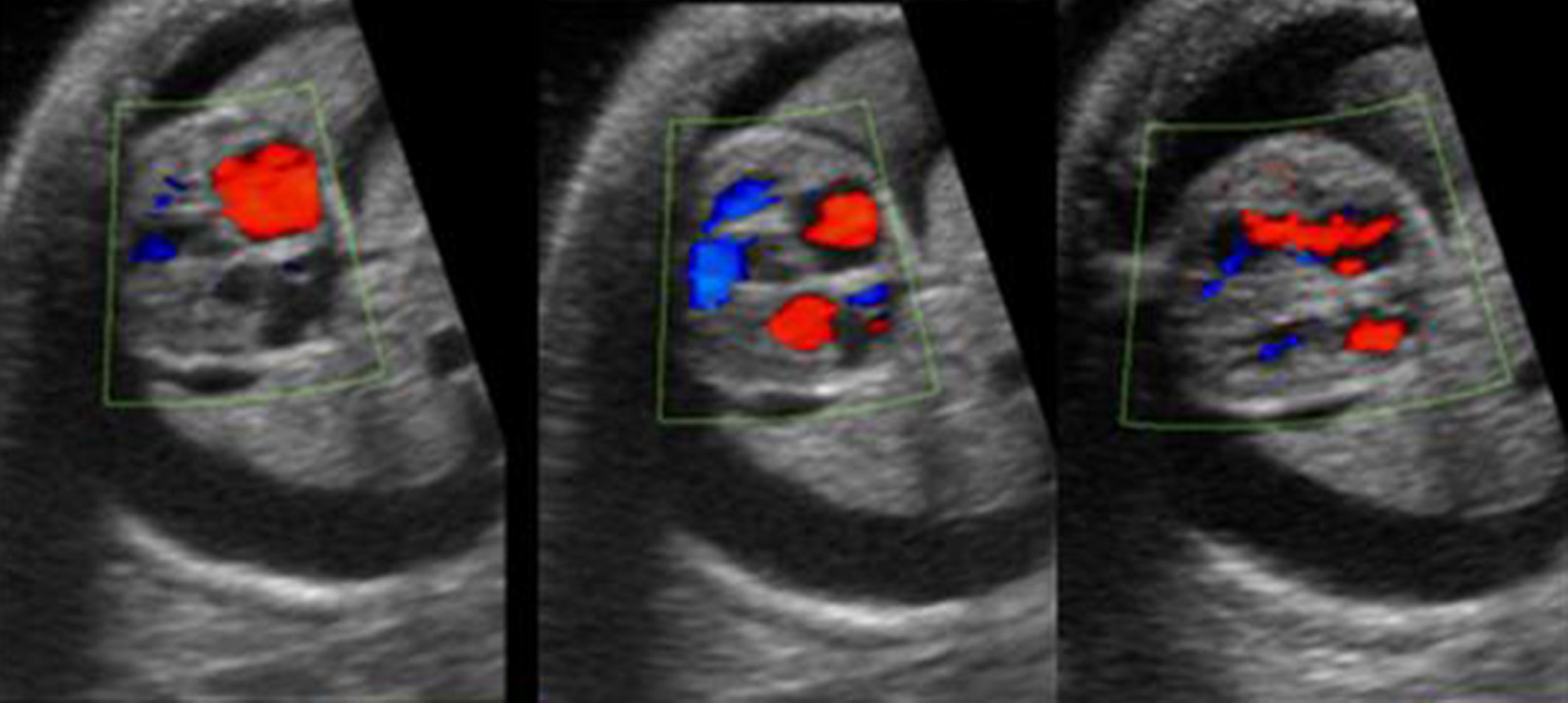
ResultsA 23-year-old mother, with second gestation with no family history nor pregnancy medication is presented. After 30 weeks of gestation, pleural effusion and ascitis were found, and the patient was sent to a Fetal Maternal Unit evaluation. In four chamber view atrium and ventricular normal size were observed, and bilateral pleural effusion and ascitis were detected (Fig. 1). The color Doppler image in the systolic and diastolic ventricular contraction, demonstrated no flow through foramen ovale with intact atrial septum and confirmed PCFO (Fig. 2). The fetal growth of cranial and femur were compatible with a 34 weeks gestation. No evidence of any other cardiac defect was present. A cesarea was done after 34 weeks and obtained a not asphyxiated newborn female of 3.4kg with no hydrops, ascitis, pleural effusion, cardiac failure, cardiac defects or any signs of chromosomal abnormality. Image was obtained with a Toshiba Power Vision 6000 ultrasound with 2D and color Doppler mode.
The PCFO has been reported to be associated a great variety of cardiac defects: transposition of great arteries, giant atrium septum aneurysm, aortic stenosis, left ventricular dilatation, mitral atresia, double-outlet right ventricle, prenatal treatment with indomethacin, non-immune hydrops fetalis or gene defects.2–9 The Doppler application is useful to detect flow changes and permeability of foramen ovale, tricuspid regurgitation, abnormalities of tricuspid and pulmonary valves or ductus arteriosus, associated with hydrops fetalis.10,11 The ultrasound of fetal heart has become increasingly sophisticated, being an accurate assessment of cardiovascular structures,12 and this is a reliable tool for prenatal diagnosis in experienced hands.13 Prenatal diagnosis of cardiac defects anticipates to family preparation for better counseling and postnatal management plans and prognosis.14 Prenatal diagnosis of cardiac defects has recently been achieved in many countries, and in cases like the PCFO that are rarely detected in <1% of cardiac defects,15 it is especially important to stop pregnancy in presence of cardiac failure or hydrops, when fetal viability is at risk.
Ethical disclosuresProtection of human and animal subjects. The authors declare that no experiments were performed on humans or animals for this investigation.
Confidentiality of Data. The authors declare that no patient data appears in this article.
Right to privacy and informed consent. The authors declare that no patient data appears in this article.
Conflict of interestThe authors declare no conflict of interest.