Traumatic neck injuries account for 5%–10% of all traumatic injuries and carry a high rate of morbidity and mortality, because several vital structures can be damaged. Currently there are several treatment streams, based on initial management by zones, initial management not based on areas and conservative management of selected patients. The objective of this systematic review is to describe the management of traumatic neck injuries.
Las lesiones cervicales traumáticas suponen un 5-10% del total de las lesiones traumáticas y acarrean una alta tasa de morbimortalidad, debido a que varias estructuras vitales pueden resultar dañadas. En la actualidad existen varias corrientes de tratamiento, basadas en el manejo inicial por zonas, manejo inicial no basado en zonas y el manejo conservador de pacientes seleccionados. El objetivo de esta revisión sistemática es describir el tratamiento de las lesiones cervicales traumáticas.
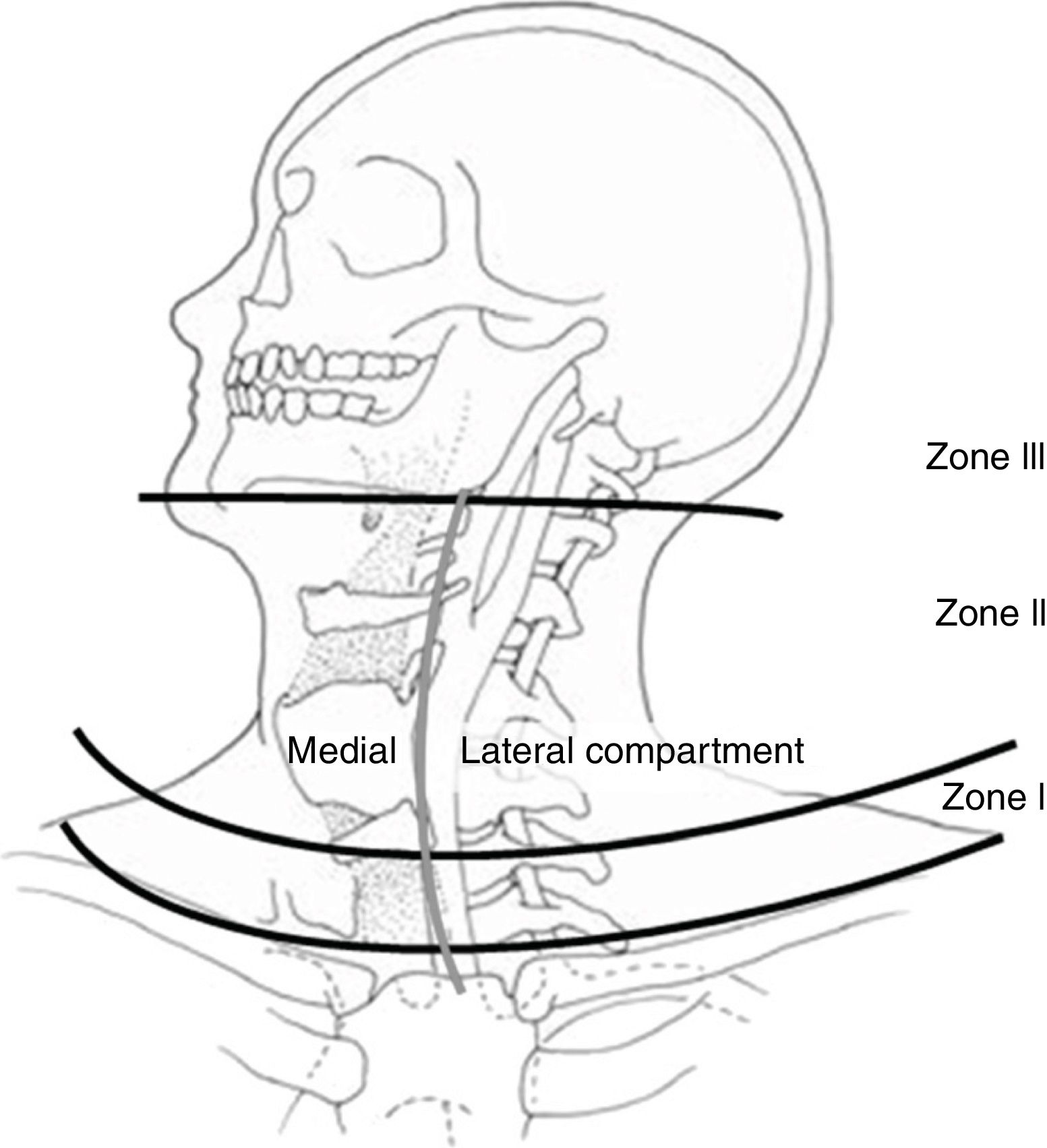
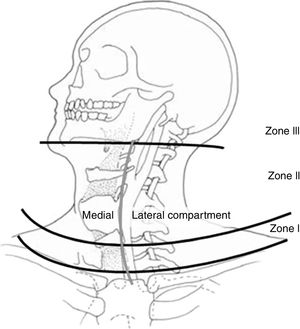
Neck injuries in patients who have suffered blunt or penetrating trauma are not frequent, although their morbidity and mortality rates are high.1,2 The management of these injuries has evolved throughout history, which has improved survival and morbidity. Since 1522, when Ambrose Paré described carotid artery ligation as a surgical procedure for the control of cervical hemorrhage caused by a sword wound, this was the technique of choice (despite its high morbidity and mortality), even during World War I.3,4 It was not until World War II that carotid artery repair was established as a treatment.5 In addition, the watch-and-wait approach was found to allow many vascular and neurological injuries to go unnoticed. Hence, surgical exploration became the treatment of choice until the 1990s, when this management began to be questioned because many explorations did not uncover injuries.6 Management of cervical injuries by zones was also established (Fig. 1 and Table 1),7,8 and currently both conservative management in selected patients9 and “no zone” management10,11 are being debated. The objective of this study was to review the literature on the management of neck trauma, with the exception of spinal and bone injuries.
Anatomical zones of the neck (Source: Monson et al.69).
Neck Zones.
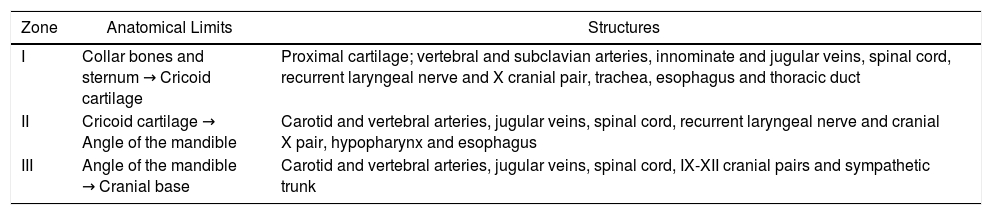
| Zone | Anatomical Limits | Structures |
|---|---|---|
| I | Collar bones and sternum → Cricoid cartilage | Proximal cartilage; vertebral and subclavian arteries, innominate and jugular veins, spinal cord, recurrent laryngeal nerve and X cranial pair, trachea, esophagus and thoracic duct |
| II | Cricoid cartilage → Angle of the mandible | Carotid and vertebral arteries, jugular veins, spinal cord, recurrent laryngeal nerve and cranial X pair, hypopharynx and esophagus |
| III | Angle of the mandible → Cranial base | Carotid and vertebral arteries, jugular veins, spinal cord, IX-XII cranial pairs and sympathetic trunk |
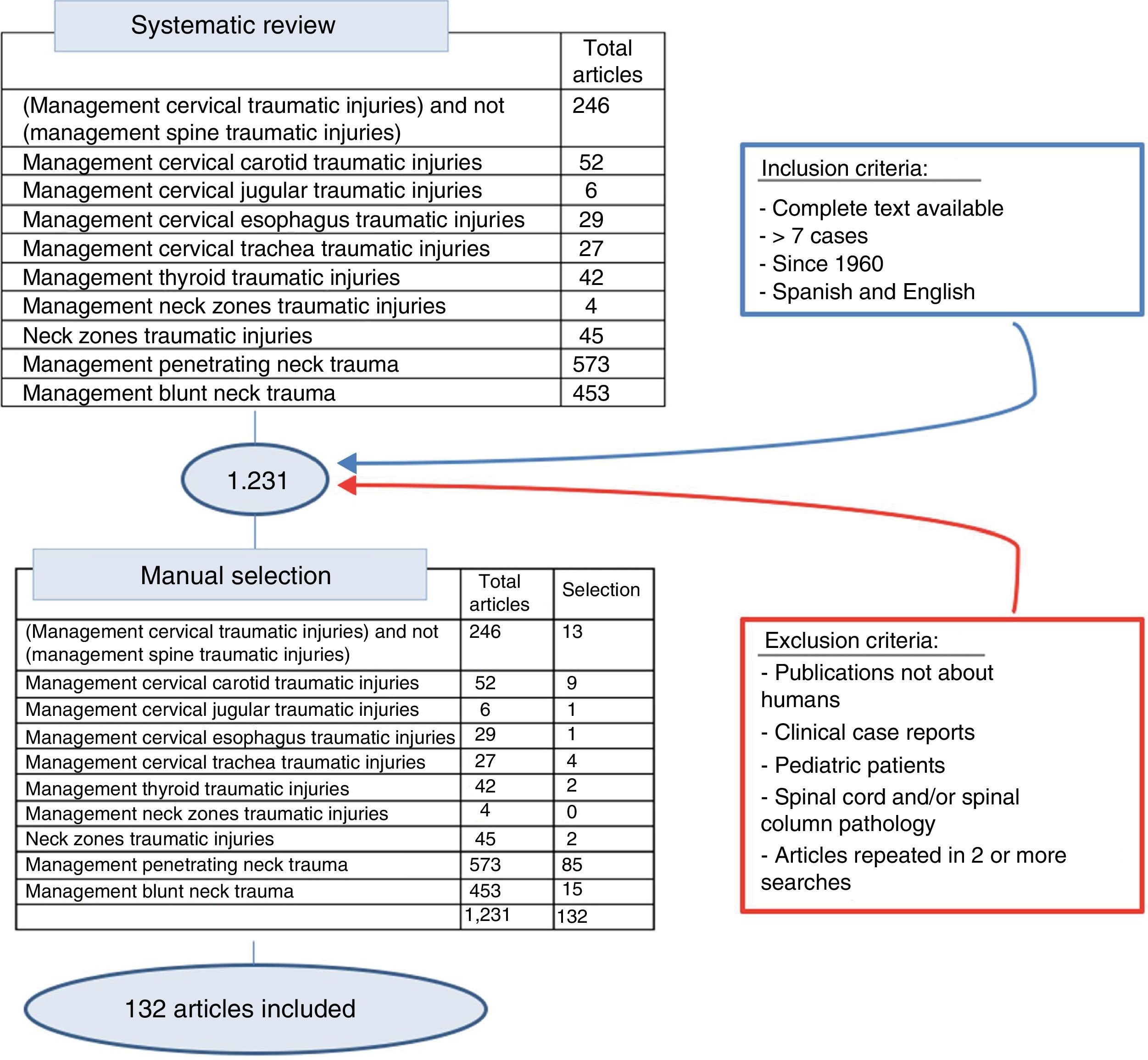
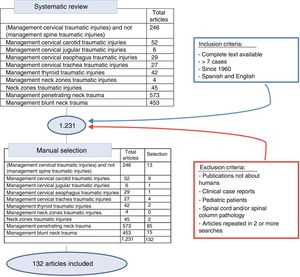
A systematic review of the literature was conducted using the SCOPUS database under the criteria established by its reviewers, conducting both generalized and organ-based searches. The following keywords were used: neck zones traumatic injuries, penetrating neck trauma, blunt neck trauma, thyroid, cervical trachea, cervical esophagus, cervical jugular, cervical carotid, combined with trauma injury management. Subsequently, the articles were reviewed manually to exclude publications not about humans, clinical case reports, literature reviews, pediatric patients, and publications in languages other than English or Spanish, making a thorough review from 1960 to 2018, inclusive (Fig. 2).
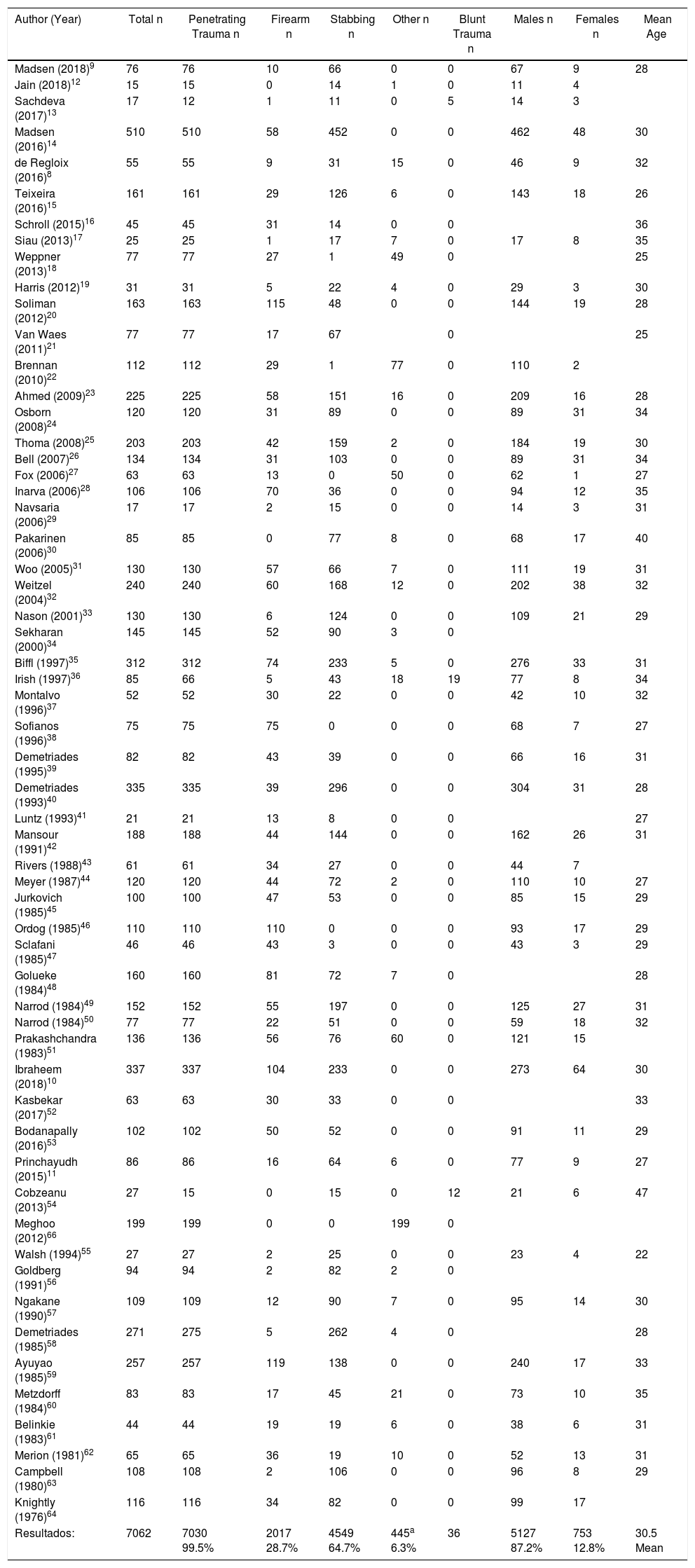
DemographicsThe incidence of neck trauma varies according to the population studied and according to the region in which the study is conducted. In our review, the incidence was higher in men with a mean age of 30.5 (Table 2).
Demographic and Trauma Mechanism.
| Author (Year) | Total n | Penetrating Trauma n | Firearm n | Stabbing n | Other n | Blunt Trauma n | Males n | Females n | Mean Age |
|---|---|---|---|---|---|---|---|---|---|
| Madsen (2018)9 | 76 | 76 | 10 | 66 | 0 | 0 | 67 | 9 | 28 |
| Jain (2018)12 | 15 | 15 | 0 | 14 | 1 | 0 | 11 | 4 | |
| Sachdeva (2017)13 | 17 | 12 | 1 | 11 | 0 | 5 | 14 | 3 | |
| Madsen (2016)14 | 510 | 510 | 58 | 452 | 0 | 0 | 462 | 48 | 30 |
| de Regloix (2016)8 | 55 | 55 | 9 | 31 | 15 | 0 | 46 | 9 | 32 |
| Teixeira (2016)15 | 161 | 161 | 29 | 126 | 6 | 0 | 143 | 18 | 26 |
| Schroll (2015)16 | 45 | 45 | 31 | 14 | 0 | 0 | 36 | ||
| Siau (2013)17 | 25 | 25 | 1 | 17 | 7 | 0 | 17 | 8 | 35 |
| Weppner (2013)18 | 77 | 77 | 27 | 1 | 49 | 0 | 25 | ||
| Harris (2012)19 | 31 | 31 | 5 | 22 | 4 | 0 | 29 | 3 | 30 |
| Soliman (2012)20 | 163 | 163 | 115 | 48 | 0 | 0 | 144 | 19 | 28 |
| Van Waes (2011)21 | 77 | 77 | 17 | 67 | 0 | 25 | |||
| Brennan (2010)22 | 112 | 112 | 29 | 1 | 77 | 0 | 110 | 2 | |
| Ahmed (2009)23 | 225 | 225 | 58 | 151 | 16 | 0 | 209 | 16 | 28 |
| Osborn (2008)24 | 120 | 120 | 31 | 89 | 0 | 0 | 89 | 31 | 34 |
| Thoma (2008)25 | 203 | 203 | 42 | 159 | 2 | 0 | 184 | 19 | 30 |
| Bell (2007)26 | 134 | 134 | 31 | 103 | 0 | 0 | 89 | 31 | 34 |
| Fox (2006)27 | 63 | 63 | 13 | 0 | 50 | 0 | 62 | 1 | 27 |
| Inarva (2006)28 | 106 | 106 | 70 | 36 | 0 | 0 | 94 | 12 | 35 |
| Navsaria (2006)29 | 17 | 17 | 2 | 15 | 0 | 0 | 14 | 3 | 31 |
| Pakarinen (2006)30 | 85 | 85 | 0 | 77 | 8 | 0 | 68 | 17 | 40 |
| Woo (2005)31 | 130 | 130 | 57 | 66 | 7 | 0 | 111 | 19 | 31 |
| Weitzel (2004)32 | 240 | 240 | 60 | 168 | 12 | 0 | 202 | 38 | 32 |
| Nason (2001)33 | 130 | 130 | 6 | 124 | 0 | 0 | 109 | 21 | 29 |
| Sekharan (2000)34 | 145 | 145 | 52 | 90 | 3 | 0 | |||
| Biffl (1997)35 | 312 | 312 | 74 | 233 | 5 | 0 | 276 | 33 | 31 |
| Irish (1997)36 | 85 | 66 | 5 | 43 | 18 | 19 | 77 | 8 | 34 |
| Montalvo (1996)37 | 52 | 52 | 30 | 22 | 0 | 0 | 42 | 10 | 32 |
| Sofianos (1996)38 | 75 | 75 | 75 | 0 | 0 | 0 | 68 | 7 | 27 |
| Demetriades (1995)39 | 82 | 82 | 43 | 39 | 0 | 0 | 66 | 16 | 31 |
| Demetriades (1993)40 | 335 | 335 | 39 | 296 | 0 | 0 | 304 | 31 | 28 |
| Luntz (1993)41 | 21 | 21 | 13 | 8 | 0 | 0 | 27 | ||
| Mansour (1991)42 | 188 | 188 | 44 | 144 | 0 | 0 | 162 | 26 | 31 |
| Rivers (1988)43 | 61 | 61 | 34 | 27 | 0 | 0 | 44 | 7 | |
| Meyer (1987)44 | 120 | 120 | 44 | 72 | 2 | 0 | 110 | 10 | 27 |
| Jurkovich (1985)45 | 100 | 100 | 47 | 53 | 0 | 0 | 85 | 15 | 29 |
| Ordog (1985)46 | 110 | 110 | 110 | 0 | 0 | 0 | 93 | 17 | 29 |
| Sclafani (1985)47 | 46 | 46 | 43 | 3 | 0 | 0 | 43 | 3 | 29 |
| Golueke (1984)48 | 160 | 160 | 81 | 72 | 7 | 0 | 28 | ||
| Narrod (1984)49 | 152 | 152 | 55 | 197 | 0 | 0 | 125 | 27 | 31 |
| Narrod (1984)50 | 77 | 77 | 22 | 51 | 0 | 0 | 59 | 18 | 32 |
| Prakashchandra (1983)51 | 136 | 136 | 56 | 76 | 60 | 0 | 121 | 15 | |
| Ibraheem (2018)10 | 337 | 337 | 104 | 233 | 0 | 0 | 273 | 64 | 30 |
| Kasbekar (2017)52 | 63 | 63 | 30 | 33 | 0 | 0 | 33 | ||
| Bodanapally (2016)53 | 102 | 102 | 50 | 52 | 0 | 0 | 91 | 11 | 29 |
| Princhayudh (2015)11 | 86 | 86 | 16 | 64 | 6 | 0 | 77 | 9 | 27 |
| Cobzeanu (2013)54 | 27 | 15 | 0 | 15 | 0 | 12 | 21 | 6 | 47 |
| Meghoo (2012)66 | 199 | 199 | 0 | 0 | 199 | 0 | |||
| Walsh (1994)55 | 27 | 27 | 2 | 25 | 0 | 0 | 23 | 4 | 22 |
| Goldberg (1991)56 | 94 | 94 | 2 | 82 | 2 | 0 | |||
| Ngakane (1990)57 | 109 | 109 | 12 | 90 | 7 | 0 | 95 | 14 | 30 |
| Demetriades (1985)58 | 271 | 275 | 5 | 262 | 4 | 0 | 28 | ||
| Ayuyao (1985)59 | 257 | 257 | 119 | 138 | 0 | 0 | 240 | 17 | 33 |
| Metzdorff (1984)60 | 83 | 83 | 17 | 45 | 21 | 0 | 73 | 10 | 35 |
| Belinkie (1983)61 | 44 | 44 | 19 | 19 | 6 | 0 | 38 | 6 | 31 |
| Merion (1981)62 | 65 | 65 | 36 | 19 | 10 | 0 | 52 | 13 | 31 |
| Campbell (1980)63 | 108 | 108 | 2 | 106 | 0 | 0 | 96 | 8 | 29 |
| Knightly (1976)64 | 116 | 116 | 34 | 82 | 0 | 0 | 99 | 17 | |
| Resultados: | 7062 | 7030 99.5% | 2017 28.7% | 4549 64.7% | 445a 6.3% | 36 | 5127 87.2% | 753 12.8% | 30.5 Mean |
On the other hand, the incidence in the military population during an armed conflict ranges between 5% and 30%, although this figure may vary, probably due to the improvement of the protection of the rest of the body and the use of new explosives.8,65,66 The incidence described in civil populations in Europe and the United States ranges between 1% and 10%.1,20,32,52 In studies conducted in South Africa, the percentage of neck injuries compared to other areas is not specified. However, their studies have a high number of patients, so their incidence is probably higher.14,67
Mechanism of InjuryMost of the articles analyzed refer to the penetrating mechanism, which is divided into gunshot wounds and stab wounds. The latter are more frequent, while gunshot wounds tend to be more serious and have associated injuries. Explosions are another mechanism of penetrating injury described in study populations involved in armed conflict.
Few studies refer to blunt trauma,36 most frequently caused by strangulation68 and traffic accidents.36 These mechanisms produce fewer injuries and have fewer complications than penetrating trauma36 (Table 2).
ManagementThe anatomical zones of the neck for the management of trauma injuries were described by Monson in 196969 (Fig. 1) and are currently being used to classify neck injuries8 (Table 1).
After the results obtained in World War II with the watch-and-wait approach, certain studies advocated surgical exploration in all patients who presented cervical trauma injuries.51,55,64 However, the percentage of negative examinations was high (40%–89%),25,30,33,42,44,45,48,52,59–62 and it was later demonstrated that conservative management in selected patients does not increase morbidity or mortality.43,45,48,49
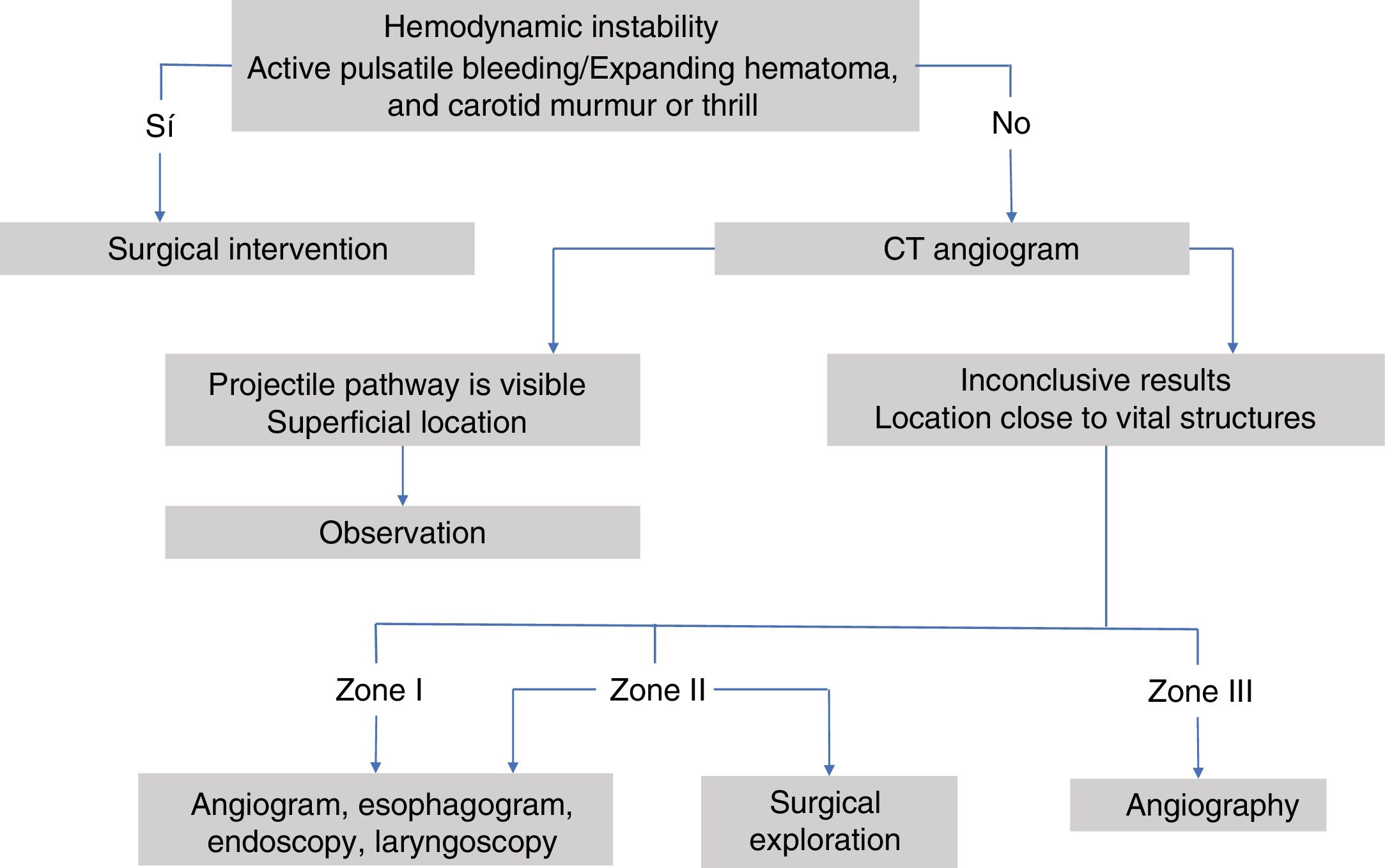
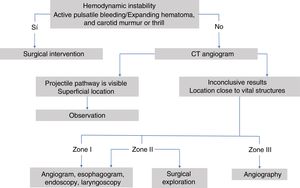
The management of cervical trauma is different depending on the area of the neck in question, hemodynamic stability and clinical signs, either the so-called ‘hard signs’ (active pulsatile bleeding, expanding hematoma, absence of carotid pulse, vascular murmur or thrill, cerebral ischemia), or ‘soft signs’ (history of bleeding at the scene, trauma in vascular territory, small non-pulsatile hematoma).
Initial management is performed following the Advanced Trauma Life Support (ATLS®) protocol of the American College of Surgeons,14,19,25,26,54,55 securing the airway and plugging wounds with active hemorrhage.12,23,35,41,42 Likewise, the Definitive Surgical Trauma Care (DSTC®) protocol is also used, whose Manual establishes current guidelines for assessing and treating these patients. Several of the studies reviewed refer to management depending on the anatomical zone in which the injury is located. Fig. 3 shows a management algorithm for this type of trauma.
Zone IThe injuries in this area have a high mortality rate (12%)36,51 because they can affect the mediastinum, large intrathoracic vessels and the tracheobronchial tree. These can go unnoticed when examining the patient, so it is important to use complementary tests for diagnosis,40,44,45 such as angiography,23,36,39,48–50 if the patient is hemodynamically stable. Since it is an invasive complementary test, the use of Doppler ultrasound is proposed to rule out vascular lesions, then using angiography only in case of positive findings on Doppler.37 It is an area of difficult surgical access, so in case of vascular lesions the use of Interventional Radiology is recommended when available.17,19,38 If surgical treatment is required, thoracic and cervical approaches are usually combined:26 middle sternotomy, anterior thoracotomy, clavicle resection or resection of the first rib.35,42,44,46,51 The presence of a cardiothoracic surgeon is recommended.17
In asymptomatic patients with no evidence of injury, conservative management is indicated,38 which consists of observation for 24–48 h, wound sutures if necessary, and possible antibiotic coverage and tetanus vaccine.
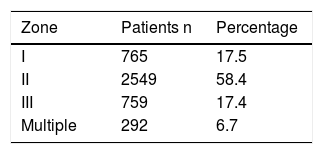
Zone IIThis is the most frequently affected anatomical area both in civil areas and regions of armed conflict (Table 3). Because this area has easy access, surgical exploration is recommended in all symptomatic patients, without the need for complementary tests, except if they are accompanied by injuries in other zones or multiple injuries.35,49 Doppler ultrasound is also proposed as the first diagnostic test in stable patients, prior to the use of angiography.37
Subsequently, given that this area is exposed, it has been proposed that complementary tests are not necessary in asymptomatic patients, as hidden injuries in this area are infrequent (0.9%), indicating selective conservative management.34,35,38,45,49,50
In unstable or symptomatic patients with exploration and/or positive diagnostic tests, surgical exploration is indicated, approaching this area by cervicotomy parallel to the anterior edge of the sternocleidomastoid muscle.26,30,38,42,44,46,49
Zone IIISurgical exposure of this zone is complicated and can lead to iatrogenic injuries that go unnoticed. Injuries in this area can cause central neurological sequelae such as coma, hemiparesis, aphasia and cranial nerve injuries.47
In stable patients, angiography is recommended23,35,39,45,47–49 to determine whether there is vascular injury and, if confirmed, to identify its location and plan the surgical intervention.36,47 When the angiography is negative, it is not advisable to perform surgical exploration.47 Injuries that are diagnosed are sometimes not surgically approachable but are treatable through Interventional Radiology techniques.17,19,35,47,48
Unstable or symptomatic patients with evidence of injuries that require surgical treatment sometimes need aggressive approaches for good exposure: horizontal incision to expose the cranial base, mandibular resection, mandibular dislocation and even craniotomy.26,44 In asymptomatic patients, observation is recommended for 24–48 h, wound suture when necessary, and antibiotic coverage and tetanus vaccine should be considered.17
Conservative ManagementAlthough selective conservative management has been shown to be safe, cervical injuries continue to be classified by zones. Therefore, action protocols have been developed depending on the severity criteria of clinical signs and findings from complementary testing.
Management continues to be surgical in unstable patients and in those with severe signs, such as active bleeding, pulsatile or expanding hematoma, neurological symptoms, hematemesis, or air leakage through the wound, regardless of the area affected by the injury.5,9,11,19,20,23–26,28
Initial conservative management is proposed in stable patients, which can vary from mere observation to the need for invasive complementary tests, such as endoscopy and angiography.17,19,33,41,45,46
In asymptomatic patients, observation alone is proposed, since a very low percentage will subsequently need surgery (0%–1%)19,21,23,35,40,42,44 and the reported mortality is 0%–1.6%.19,21,23,25,28,30,35,38,39,44,58 Patients operated with negative examinations have a significantly longer postoperative stay than those who have been under observation.19,30,35,39,87 Even with selective conservative management, 19%–38% of cervical examinations were negative.10,19,20,28
Diagnostic TestsAngiography was the gold standard for the diagnosis of vascular injuries until 2008.24 However, it has been dismissed as a screening method since the results are usually negative, the test has a high economic cost, and associated complications include hematomas, vasospasm, atherosclerotic plaque emboli, thrombosis and arterial dissection.26 Subsequently, computerized tomography angiogram (CT angiogram) has been established as an initial diagnostic test. It has the advantage of being available at most hospitals, it can be done in 2–3 minutes, and it can explore vessels, soft tissue and bone. Its sensitivity and specificity for vascular injuries are 90%–100%,21,22,24,26 while the sensitivity and specificity to determine which symptomatic patients need a surgical exploration are 83%–100% and 98.6%–100%, respectively.11,16 CT angiogram has replaced angiography as the first diagnostic test at many hospitals.11,15,16,18,19,21,22,24,26
With the increasing use of CT angiography, the need to perform invasive complementary tests decreases significantly, as do the number of cervical examinations and the number of negative cervical results.8,19,21,24–26,28,31
There are some studies of patients who had undergone CT angiogram after deciding to perform surgical exploration. In this group, no exploration was negative. However, in the remaining group, 36%–40% of cervical examinations were negative.16,22
Surgical TreatmentAs management protocols improve for selective conservative management, the percentage of patients who do not require surgical exploration increases (74%–78%).19,25
Physical examination and complementary tests seem sufficient to indicate surgical intervention or observation.23 As predictors of a serious injury, severe clinical symptoms have a sensitivity of 96%–97.2% and a specificity of 87.4%–97.2%.22,23,66 Severe symptoms together with the findings from complementary tests have a sensitivity of 100%, and their absence has a negative predictive value of 100%.19 CT angiography has a sensitivity and specificity to diagnose aerodigestive injuries of 76% and 97%, respectively.53
In patients with active bleeding, a Foley catheter is useful for the initial stabilization of the patient, after which complementary tests can be done to determine the possible indication for urgent surgical intervention.21,25,29 In patients whose bleeding is under control and no arterial injury has been found on arteriography or CT angiogram, the injury is assumed to be venous; urgent surgery is avoided, and the catheter is removed 48–72 h later in the operating room.9,21,25,29 Comparing the results of the use of a Foley catheter with external pressure together with procoagulant drugs, no statistically significant differences were found between the number of initially controlled hemorrhages. However, the percentage of re-bleeding is significantly higher in those patients in whom external pressure was used (7% Foley vs. 26% external pressure).18
Treatment by OrgansAirway InjuriesTo secure the airway, orotracheal intubation is recommended when necessary; if this is not possible, an urgent cricothyroidotomy should be done,25 and the surgical technique is safer than the percutaneous one.70 Rapid-sequence intubation is most often used in both the prehospital (69%–77%)24,26,71 and hospital (81%)72–74 settings, and it is considered a safe technique (88%–100%).73–75 However, no statistically significant differences were found between the different techniques to secure the airway.76 Prehospital blind nasotracheal intubation is also a safe option.32
Laryngotracheal injuries are uncommon and are mainly caused by blunt trauma.77–84 Injuries to the pharynx and larynx are usually easily diagnosed during examination. The absence of clinical signs (blood in the mouth, odynophagia, dysphagia, transcervical wound) has a negative predictive value of 91%–95%.25 Patients with this type of trauma progress satisfactorily with conservative management (nasogastric tube, enteral nutrition and antibiotic therapy).21,25,53,83,85–89
Thyroid cartilage fracture is one of the most frequent injuries found in surgical examinations after blunt trauma.90 Surgical treatment is advised in cases of displacement.77 The thyroid gland is frequently damaged; however, injury does not endanger the patient’s life.91,92
Most tracheal injuries have an indication for surgical management.79,80,82,93–95 Conservative management is only justified in iatrogenic injuries and those that meet strict criteria.96,97
Esophageal InjuriesThe absence of dysphagia and saliva in the wound, together with negative complementary test results (esophagogram and endoscopy) have a predictive value of 98%.25 Flexible endoscopy has a sensitivity of 100% and a specificity of 94% for the diagnosis of esophageal trauma injuries,98 although it cannot always be performed in these patients.99 As for CT angiography, very wide ranges of sensitivity have been reported for the diagnosis of cervical esophageal lesions (50%–100%).28,53
Most authors advocate the surgical treatment of these injuries22,25,99–104in less than 24, h, as, a longer delay entails a significant increase in morbidity, mortality.105–108
Vascular InjuriesThe majority of patients who require surgery have vascular involvement.20,22,24–26,58,61 To rule out major vascular injuries, physical examination is sufficient.25,34,40
Repair of penetrating internal carotid injuries should be attempted in non-comatose patients, unless the patient is unstable109–111 since their ligation causes neurological deficits and death.111,112 However, injuries of the external carotid or its branches can be treated by ligation.26
Vertebral artery injuries require surgical exploration in unstable patients. These arteries can be well visualized by CT angiogram.113–115 If an injury is observed, angiography is recommended as it avoids unnecessary surgical examinations and allows for endovascular treatment (morbidity 0.5%, mortality 0%).116
Venous injuries of large isolated vessels (subclavian and internal jugular veins) can be managed with observation in stable patients,9,28,66 and bleeding can be controlled with a Foley catheter in unstable patients, to be later removed in 48–72 hours.9 If the hemorrhage cannot be controlled with the Foley, or if there are accompanying arterial or aerodigestive tract injuries, urgent surgery is necessary.53 Although ligation of the veins may initially cause edema, this condition resolves itself in a few days.110,117
Arterial thrombosis of the cervical vessels after blunt trauma is a known entity, but its incidence is low (0.1%–3% carotid).115,118–121 The incidence in vertebral arteries is lower, and there are less frequently clinical repercussions.118,119,122 Arterial thrombosis should be suspected in lucid patients with hemiparesis, hemiplegia, Horner syndrome, or carotid murmur and normal cerebral CT that does not explain their neurological deficit, accompanied by skull and facial fractures that affect the territory of the internal carotid artery.123 Cervical pain is not usually a symptom related to this pathology.118–119 CT angiogram and Doppler ultrasound may not show alterations in the damaged arteries during the first 12 h.118,119,123 Magnetic resonance imaging (MRI) is able to diagnose this trauma faster.118 However, angiography remains the gold standard study118,119 due to its sensitivity.121 Anticoagulation and/or antiplatelet therapy seem to be the most beneficial therapies.119,120,124
In 1999, Biffl125 proposed the following classification of vascular lesions after closed trauma for prognosis and treatment:
- -
Grade I: 2/3 involvement of the intima
- -
Grade II: dissection or hematoma with luminal stenosis
- -
Grade III: pseudoaneurysm
- -
Grade IV: complete occlusion
- -
Grade V: transection
In the case of carotid injuries, conservative management is proposed for grade I and surgery is recommended for the remainder. In inaccessible grade II, III and IV injuries, treatment with anticoagulation is recommended. In lesions grade II and III injuries with reduction of the lumen, endovascular treatment using stents is safe.126,127 Endovascular techniques can be a resource in case of grade V injuries.115,125
Grade I and II vertebral injuries evolve satisfactorily without treatment.128 Grade III and IV injuries, however, require treatment with antiplatelet agents and/or anticoagulants due to a higher rate of cerebrovascular accidents (CVA).129
After blunt trauma with suspected thoracic aorta injury, it is important to extend the carotid angiography study, as this injury is frequently associated but may go unnoticed.130
Morbidity and MortalityThe overall mortality rates reported in these patients range from 3 to 13%.8,9,20,22,32,35,131 Laryngotracheal injuries can lead to the death of patients and serious complications, such as tracheoesophageal fistulae with aspiration,84,93 immobilization of the vocal cords, tracheal stenosis, dysphonia and prolonged dysphagia.78,79,83,93,131–134
Delayed diagnosis of esophageal trauma increases morbidity and mortality, causing infectious complications such as mediastinitis, pharyngoesophageal abscess, empyema, fistula and sepsis.73,99,102,105,135
Blood loss due to vascular injuries can be fatal.117 If a venous injury requires ligation, edemas in the upper extremities may develop, which becomes more evident when the subclavian vein is ligated.117 If there is trauma to the superior vena cava, edema in the arms, neck and head is reported, even after its repair.117 Damage to the internal carotid artery can lead to permanent neurological damage112 since they cause cerebrovascular accidents (embolic, ischemic and hemorrhagic),136 and morbidity and mortality are higher in penetrating injuries than in blunt trauma.112 Distal internal carotid trauma has more morbidity and mortality than trauma to the common carotid.112 Complete occlusion of the 2 vertebral arteries results in cerebellar infarction; however, if a vertebral artery maintains its flow, this event is rare.115,116
Special ConsiderationsAlthough most authors advocate urgent surgical exploration in both unstable patients and those with severe signs, Madsen9 and Schroll16 go one step further, demonstrating that performing CT angiograms in patients with severe signs also decreases the need for surgical exploration and, if required, facilitates planning.
That said, it is important to take into account both the resources of the hospital where these patients are treated, as well as its patient volume and experience. Hospitals with low volumes have an understandably higher percentage of cervical examinations (60%), as well as negative examinations (65%). It would be desirable for each hospital, depending on its resources and incidence, to have an action protocol for this type of trauma, thereby minimizing unnecessary surgical interventions.30
Another scenario to contemplate are the areas of armed conflict, with its peculiarities, such as the time of evacuation of patients to a tertiary hospital.28 The authors advocate the conservative selective management of these patients, presenting a percentage of cervical examinations around 30%. However, many of these patients require urgent surgical intervention due to instability caused by other injuries, and previous CT angiogram cannot be performed.22 They propose the same use of CT angiogram as in civil hospitals;28 however, we should be reminded that these patients can present artifacts due to metal fragments.22,27 In this case, the use of Doppler ultrasound is recommended in zone II and angiography is recommended in patients with involvement of zones I and III or abnormal ultrasound.27
We should specifically mention injuries caused by bulls and other horned animals. There are different classifications for this type of trauma, depending on the mechanism of injury or their severity.137 The cervicofacial region is one of the least affected by this mechanism. Chambres et al.138 ranked it as the third location (16% versus 64% in the lower extremities). The wounds are incisive and contusive, presenting special characteristics. For instance, the entrance opening is usually small and surrounded by an area of erosion, and one or more deep tracts may be present, usually with significant destruction of muscle tissue. These wounds are contaminated, and multiple foreign bodies can be found at the bottom of the wound path, including fragments of cloth, dirt and horn splinters. The depth will depend on the penetration force of the antler in the body as a result of the weight and speed of the animal. Additional force is applied due to the effect of the strong muscles of the animal’s neck when lifting its horns, causing tears in the arteries, veins and nerves at right angles to the ground.139 Bull horn injuries are their own entity, and there is no equivalent found among other trauma etiologies. Therefore, in all cases, these patients should be considered polytrauma patients.
Conclusions- -
Initial management of these patients is established according to ATLS criteria.
- -
Urgent surgical examination is indicated in unstable patients and patients with severe signs; the latter may benefit from previous CT angiography.
- -
If hemodynamic instability is caused by hemorrhage, tamponade with a Foley catheter can assist in the initial stabilization of the patient, providing the necessary time to perform a CT angiogram and diagnose the injury type.
- -
It is advisable to perform a CT angiogram in all symptomatic patients (reducing the need for surgical examinations, as well as their complications), and also in asymptomatic patients with a high-speed mechanism of injury.
- -
Observation is safe in asymptomatic patients; those with negative CT angiogram do not require treatment.
- -
Angiography and Interventional Radiology can be a diagnostic and therapeutic tool in patients with vascular trauma, thereby avoiding unnecessary surgical interventions.
The authors have no conflict of interests to declare.
Please cite this article as: Petrone P, Velaz-Pardo L, Gendy A, Velcu L, Brathwaite CEM, Joseph DK. Diagnóstico, manejo y tratamiento de las lesiones cervicales traumáticas. Cir Esp. 2019;97:249–500.