Wilkie syndrome, also referred as superior mesenteric artery syndrome, is an unusual cause of a proximal small bowel obstruction. It is characterised by the compression of the duodenum in its third portion due to a narrowing of the space between the superior mesenteric artery and the aorta. Its presentation symptoms are consistent and include the obstruction of the proximal small bowel. However, the physical and laboratory findings are non-specific. Nevertheless, many imaging methods are useful for its diagnosis. The management of this condition varies between observation and surgery, depending on each particular case.
Clinical caseThe case is presented of a 19-year-old male who began with acute, intense abdominal pain, nausea, vomiting, and diarrhoea. On examination, he had abdominal wall rigidity and hyperesthesia. Imaging studies were requested, revealing a decreased superior mesenteric artery angle, a shortening of the aortic mesenteric distance, and a decrease in the calibre of the third duodenal portion, all findings concomitant with Wilkie syndrome. Conservative treatment was applied and the patient was discharged without complications.
ConclusionsWilkie syndrome continues to be an unknown condition to the general practitioner, and the underdiagnosis of this condition may put a patient at risk of serious complications. A high index of suspicion is required to reach a diagnosis. Early treatment should give a good outcome most of the time.
El síndrome de Wilkie o síndrome de la arteria mesentérica superior es una causa inusual de oclusión intestinal alta, se caracteriza por la compresión del duodeno en su tercera porción, es secundaria a un estrechamiento del espacio entre la arteria mesentérica superior y la aorta. El cuadro clínico suele estar caracterizado por síntomas de oclusión intestinal alta, la exploración física y los hallazgos de laboratorio suelen ser poco específicos. Diversos estudios de imagen son útiles para el diagnóstico. El tratamiento puede ir desde conservador, hasta la cirugía, que depende de cada caso.
Caso clínicoVarón de 19 años, que cursó con dolor abdominal súbito, intenso, náuseas, vómitos y diarrea; motivo por el cual acudió al servicio de urgencias, donde a la exploración destacaron: rigidez abdominal con hiperestesia e hiperbaralgesia, y los estudios de imagen evidenciaron una disminución del ángulo de la arteria mesentérica superior y de la distancia aortomesentérica; además de disminución del calibre de la tercera porción del duodeno, hallazgos característicos del síndrome de Wilkie. Se dio tratamiento conservador, siendo dado de alta hospitalaria sin complicaciones.
ConclusionesEl síndrome de Wilkie continúa siendo una entidad poco conocida por el médico general, el que poco se diagnostique o se piense en este síndrome, puede ocasionar complicaciones serias por lo que se requiere que el médico guarde un alto índice de sospecha diagnóstica ante esta patología. El tratamiento oportuno confiere un buen pronóstico la mayoría de las veces.
Wilkie syndrome, which is also known as upper mesenteric artery syndrome, plaster corset syndrome or aortomesenteric compass syndrome, is characterised by compression of the third portion of the duodenum. It is secondary to narrowing of the space between the upper mesenteric artery and the aorta. Although this entity was first described by Rokitansky in 1861,1 it was in 1921 when Wilkie2 published a series of 75 cases resolved by surgery that it became known eponymously.
Several risk factors have been found in association with this pathology. One of the most widely accepted causal theories is the loss or reduction in the mesenteric fat which functions as a cushion between the aorta and upper mesenteric artery.3 However, other case reports associate Wilkie syndrome with: HIV, neoplasias, diabetes mellitus,4 orthopaedic surgery for scoliosis,5 bariatric surgery,6,7 vascular surgery, major catabolic states, sudden weight loss and eating disorders such as anorexia nerviosa.8
Patients may present with symptoms that commenced suddenly or ones with a tendency to become chronic.9 The most common symptoms are those of upper intestinal blockage. The reasons why these patients visit include: postprandial epigastric pain, early satiety, nauseas, vomiting bile, pyrosis, ingurgitation and weight loss peso; some postures may relieve the symptoms, as they free the duodenum from compression.2 Although findings in physical examination are not characteristic, some conditions which are usually found are: abdominal distension, poorly localised pain and alterations in peristaltic noises. Laboratory findings may show hydroelectrolytic alterations after major vomiting or diarrhoea, given that late diagnosis may lead to fatal complications such as perforation and pylephlebitis.10
Several imaging studies are useful in the diagnostic approach when there is a suspicion that a patient has Wilkie syndrome, which in all cases requires that the doctor retain a high degree of suspicion to achieve a true and accurate diagnosis. At the present time computerised axial tomography is considered to be the gold standard diagnostic method. Nevertheless, findings using other imaging techniques may lead to the suspicion of a diagnosis when the clinical symptoms and risk factors are present. It is due to this that the approach usually commences with simpler and more economical methods. Simple abdominal X-ray may show major gastric dilation; a gastroduodenal series with oral contrast usually shows duodenal compression in the third part of the duodenum with active peristalsis, slow contrast transit and duodenal dilation close to the obstruction.9 Abdominal ultrasound scan by an expert is a good diagnostic alternative, given that it is possible to measure the aortomesenteric angle with the advantages of not exposing the patient to ionising radiation, its accessibility and low. However, this technique has the major disadvantage of being operator-dependent.11 Arteriographs are currently not used for the diagnosis of this pathology, and this technique is only used in cases with a high level of diagnostic suspicion and inconclusive results using other imaging methods.
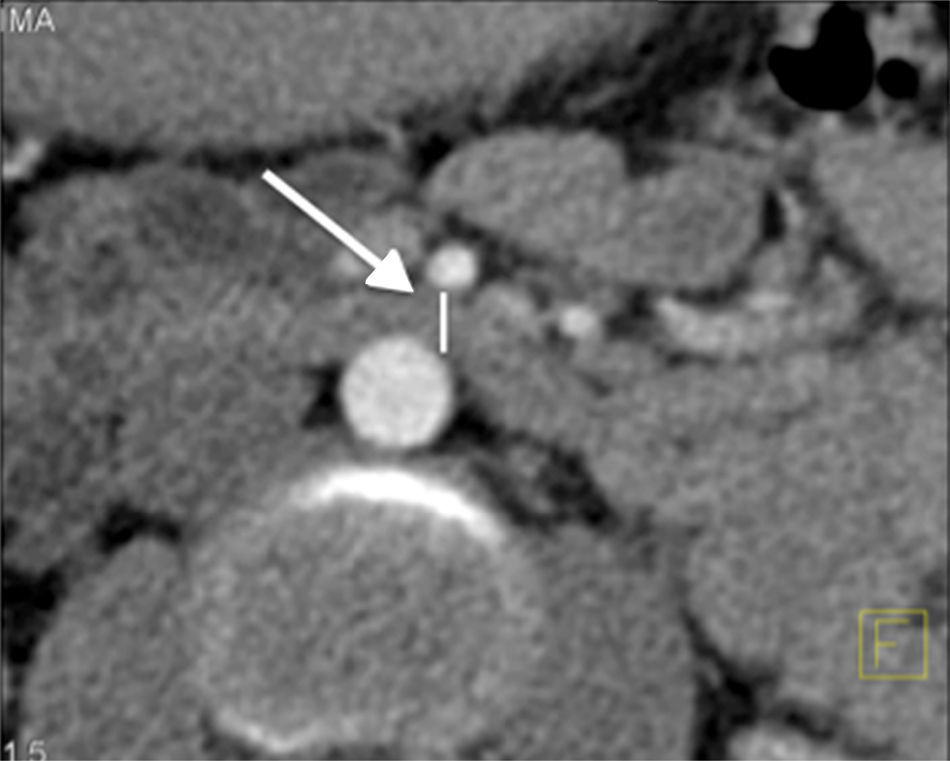
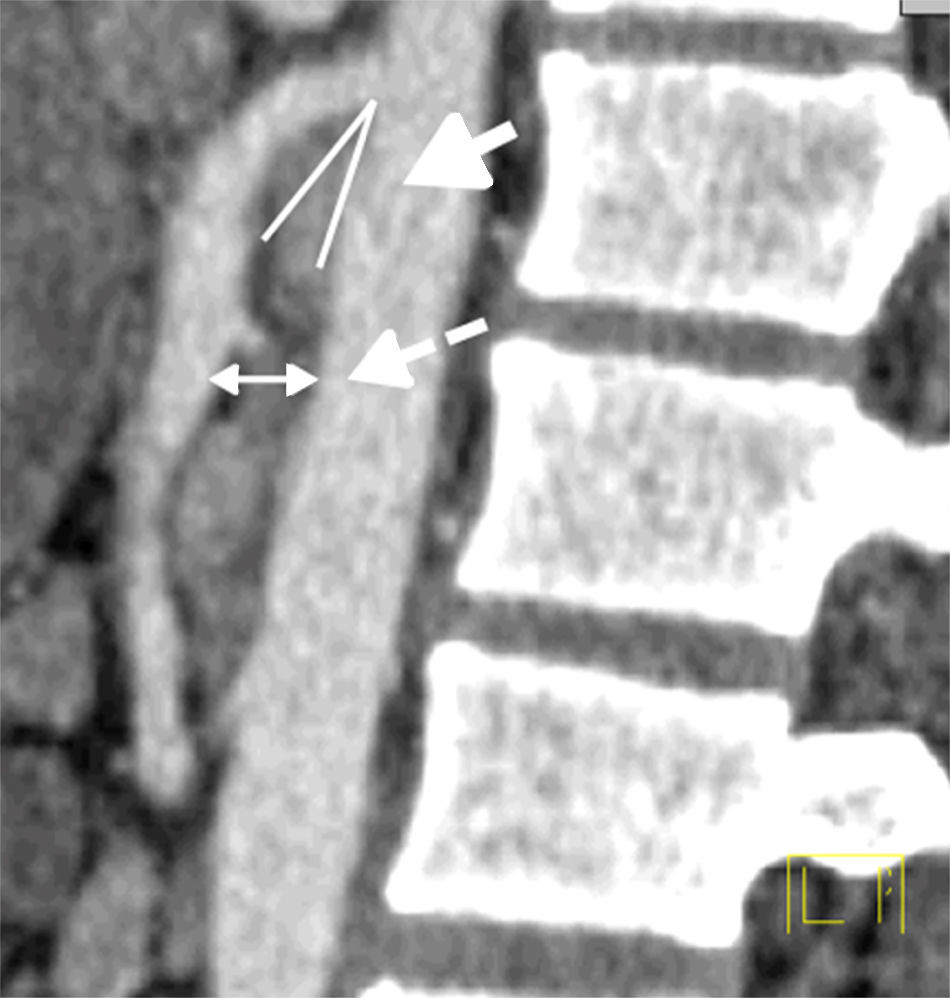
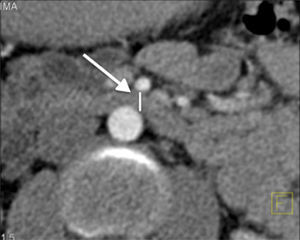
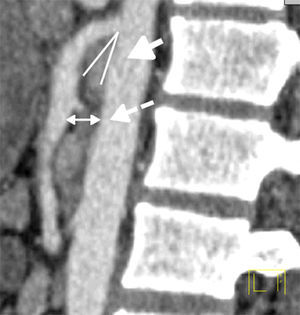
Computerised tomography has almost 100% specificity and sensitivity in diagnosis when the following criteria are fulfilled: (1) abrupt obstruction in the third portion of the duodenum, with active peristalsis, (2) an aortomesenteric angle of less than 25° (normal values run from 38° to 65°),12 particularly when the distance from the aorta to the mesenteric artery is equal to or less than 8mm (normal values are from 13 to 34mm),13–15 and (3) the upper duodenum is affixed by Treitz's ligament or anatomical variants of the upper mesenteric artery.
The initial treatment is usually conservative. It aims to relieve the symptoms caused by the obstruction while correcting the factors that triggered it. This treatment consists of hydrating the patient, inserting a nasogastric tube, replacing and balancing serum electrolytes16 and possibly feed the patient in special positions that free the obstruction and bring about the opening of the aortomesenteric angle through mechanical effects (prone, left lateral decubitus) or by inserting a nasojejunal tube, which gives good results.17 In those cases in which the syndrome is a result of eating disorders, the involvement of the psychiatric department is indispensible.
Surgical treatment (gastrojejunostomy, duodenojejunostomy, Strong's operation) is necessary in some cases when conservative treatment is unable to relieve the symptoms. It may use a laparoscopic approach18 or open surgery. Each of the surgical techniques currently used has its own difficulties, advantages, complications and drawbacks; nevertheless, laparoscopic duodenojejunostomy is the procedure of choice in comparison with the other techniques.19,20
Clinical caseWe present the case of a 19-year-old male patient who was initially diagnosed with symptoms of repetitive infectious gastroenteritis, treated with antibiotics and antispasmodics. He was admitted to the emergency department with symptoms characterised by colic-type abdominal pain, located in the mesogastrium and irradiating to all quadrants. This was accompanied by nausea, vomiting and weight loss. When questioned he denied any history of recent trauma, surgery, prolonged immobilisation or neurological disease; he mentioned gradual and unintentional weight loss. Abdominal examination revealed a distended abdomen, mild epigastric pain and hyperactive intestinal noises, without any palpable organomegalies. His haemoglobin was 17g/dl and the leucocyte count was 5.1×103/mm3. Albumin in serum was 2.5mg/dl. Arterial gasometry was performed, with the following findings: pH 7.48, PCO2 33.2, PO2 79.2, lactate 1.3mmol/l, HCO3 24.8, while the remaining laboratory data were within parameters.
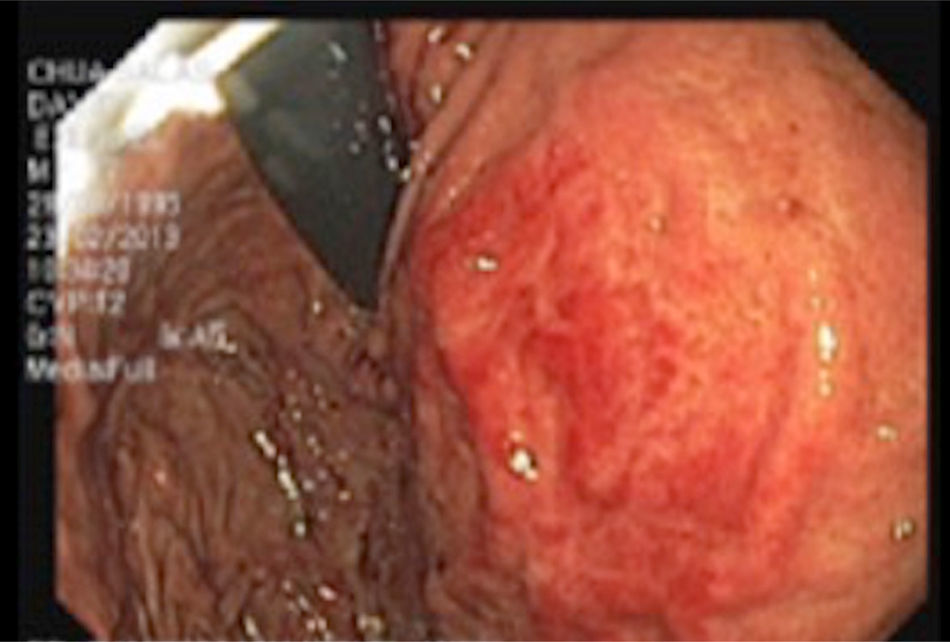
Endoscopic examination of the upper gastrointestinal tract revealed: mild esophagitis, stomach and proximal duodenum with major dilation, together with narrowing of the third portion of the duodenum due to pulsing extrinsic compression (Fig. 1).
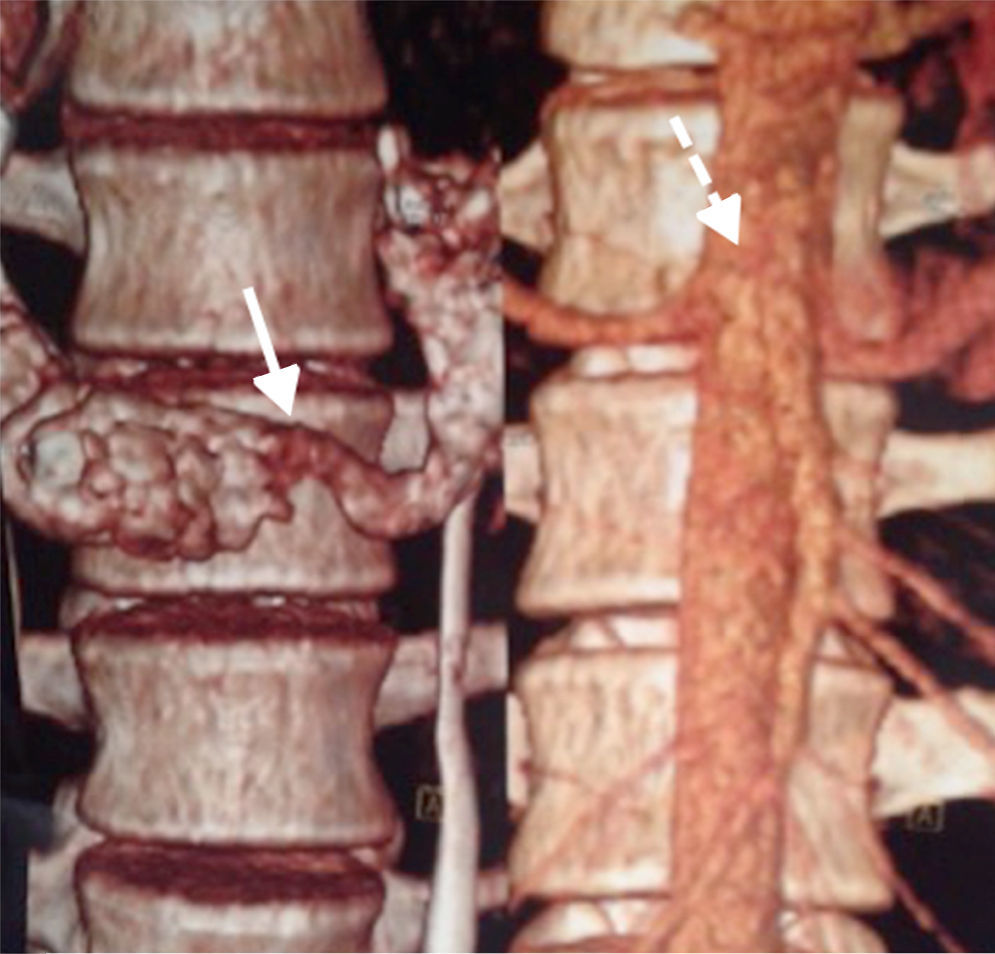
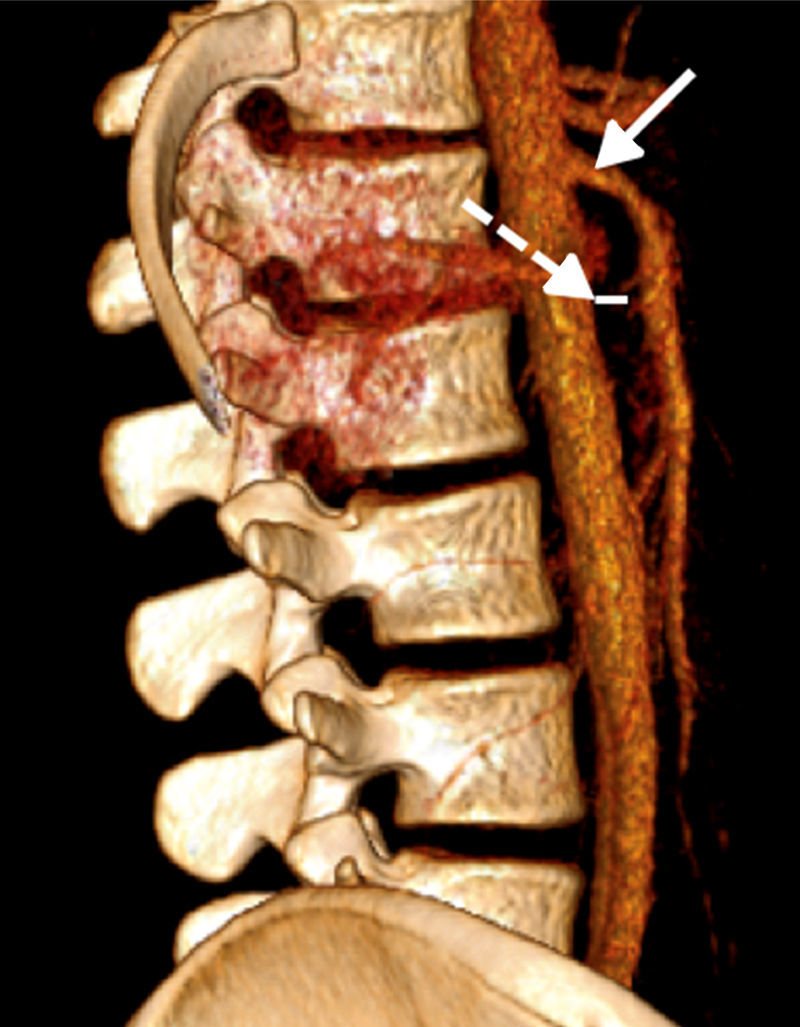
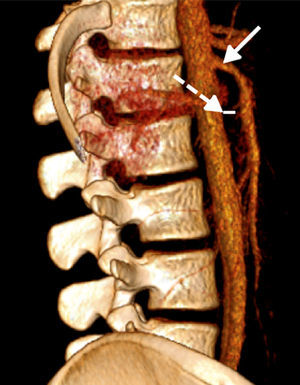
Abdominal computerised axial showed major gastric distension and dilation of the first and second portions of the duodenum, with extrinsic compression of the third duodenal portion, with a reduction of the angle of the upper mesenteric artery and the aortomesenteric distance (Figs. 2 and 3). Three-dimensional reconstruction showed the same findings, i.e., a reduction of the aortomesenteric angle and the aortomesenteric distance (Figs. 4 and 5). These characteristics strongly suggested Wilkie syndrome, so the patient was admitted to the general surgery department for treatment and medical monitoring. He was treated conservatively using intravenous hydration, analgesia, the insertion of a nasogastric tube to decompress the stomach and parenterally replace serum electrolytes. The patient progressed favourably, so he was discharged from hospital without requiring surgery.
This syndrome was described by Rokitansky more than 100 years ago in 1861.1 It is extremely rare, and an incidence of 0.2% was found in 6000 radiological studies. Three duodenal obstruction mechanisms have been described: (1) a very acute aortomesenteric angle; (2) a transversal duodenum in a high position due to a short Treitz ligament, and (3) an anomalous route of the mesenteric artery or one of its branches, displaced downwards and in front of the spinal column.21
This condition is more common in women and young adults, and in the majority of cases it presents after a major weight loss. Nevertheless, in 2006 Biank and Werlin17 published a series of 22 children, of whom only 50% had lost weight prior to their diagnosis. The causes of Wilkie syndrome may be classified in five groups: consumptive syndromes (AIDS, cancer, major burns, endocrinal pathologies, poor intestinal absorption); eating disorders (anorexia nervosa); postoperative (orthopaedic surgery, spinal surgery); severe trauma (craneoencephalic trauma, polytraumatism) and spinal deformities, diseases or lesions. Cases have been published recently in association with rapid weight loss after bariatric surgery.22
Wilkie syndrome symptoms are non-specific, and it may present as intolerance to food with nausea and vomiting, weight loss, early satiety, abdominal distension and epigastric pain. The pain may be relieved when the patient lies in prone decubitus, left lateral decubitus or a genupectoral position. These manoeuvres relax the pressure of the mesenteric artery on the duodenum,20 and this may guide diagnosis.
Patients may complain about reflux, which may be shown by the endoscopic study of stasis-linked esophagitis or gastritis. There is also a higher prevalence of duodenal ulcers than is the case for the general population (up to 45%). Fatality is secondary to severe hydroelectric alterations, gastric perforation, an obstructive bezoar and gastric or portal pneumatosis. Once the clinical symptoms are established they self-perpetuate, regardless of their aetiology.18
Historically a barium study that made it possible to observe the dilation of the first and second duodenal portions and the compression of the third portion was the diagnostic test used, together with arteriography. Nevertheless, computerised angiotomography has recently been shown to have greater diagnostic sensitivity.
The severity of the symptoms is correlated with aortomesenteric distance. Endoscopy helps to rule out intrinsic lesions of the digestive tract that may lead to obstruction, and it also permits taking biopsies.23
Patients with acute presentation almost always respond to conservative treatment, while those with chronic symptoms usually require surgery after a period of time during which they receive increased nutrition. Surgery is indicated in patients after: (1) the failure of conservative treatment, (2) long-term progression of the disease with gradual weight loss and duodenal dilation and stasis, and (3) complicated peptic ulcerous disease secondary to cholestasis and reflux.24
The surgical operations proposed for treatment include: Strong's procedure, gastrojejunostomy and duodenojejunostomy. Although Strong's procedure maintains the integrity of the gastrointestinal tract, it has a 25% failure rate. Although gastrojejunostomy permits gastric decompression, it does not relieve duodenal compression, so that digestive symptoms may persist and lead to the appearance of blind loop syndrome or recurring peptic ulcers. Duodenojejunostomy is the procedure of choice, with a success rate higher than 90%. Gastroparesis often occurs after surgical correction, in connection with gastric and duodenal flaccidity.
There is little information about management of this condition in modern medical literature, although treatment with prokinetic agents may be tried.25
In the case of our patient the clinical presentation coincided with descriptions in the literature and the main symptoms of blockage of the upper intestine. Although the results of physical examination were not very specific, radiological techniques confirmed the definitive diagnosis. Hypoalbuminemia was detected in laboratory studies. This is compatible with a state of acute malnutrition secondary to caloric deficit or an aggregated catabolic state that would support the theory of a reduction or loss of retroperitoneal fat. Arterial gasometry showed uncompensated respiratory alkalosis secondary to antalgic hyperventilation and anxiety. Conservative treatment and general measures brought about the remission of the acute symptoms.
ConclusionsWilkie syndrome is a rare entity that is still hardly known to general practitioners. Under-diagnosis may lead to the risk of patients suffering serious complications, so that doctors should maintain a high level of diagnostic suspicion regarding this pathology. Correct treatment leads to a good prognosis in the majority of cases.
Ethical disclosuresProtection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of dataThe authors declare that they have followed the protocols of their work center on the publication of patient data.
Right to privacy and informed consentThe authors declare that no patient data appear in this article.
Conflict of interestsThe authors have no conflict of interests to declare.
Please cite this article as: Hermosillo-Cornejo DG, Girón-Gidi AD, Vélez-Pérez FM, Lemus-Ramírez RI, Martínez-Garza PA. Síndrome de Wilkie. Reporte de un caso. Cir Cir. 2017;85:54–59.