Non-traumatic spontaneous rupture of the biliary tract and retroperitoneal accumulation (retroperitoneal biloma) is an extremely rare condition.
Clinical caseA 57 year-old woman with no known biliary disease, started with intense pain in the right abdomen 30 days prior to consultation. She also had jaundice (4+). The initial hepatobiliary ultrasound reported choledocholithiasis and retroperitoneal fluid collection, which was confused with a peri-renal abscess. Guided puncture was performed and the presence of bile was evident. Dilation of the bile duct was observed in the computed tomography. The patient underwent laparotomy to correct both conditions.
ConclusionThe retroperitoneal biloma, also called choleretroperitoneum, is of multifactorial origin. Clinical presentation is non-specific, with diffuse abdominal distension and pain in all patients. The diagnosis is made based on ultrasonography and computed tomography, and can even be diagnosed intra-operatively. The treatment is based on liquid bile drainage and correction of the leak.
La rotura espontánea no traumática de las vías biliares y su acumulación en retroperitoneo (biloma retroperitoneal) es una condición infrecuente.
Caso clínicoMujer de 57 años de edad, no conocida como portadora de enfermedad biliar, que inició padecimiento 30 días previos a consulta, con dolor intenso en hemiabdomen derecho y posteriormente ictericia (4+). En el ultrasonido hepatobiliar inicial se reportó: coledocolitiasis y colección de líquido retroperitoneal, que se confundió con un absceso perirrenal roto. Se realizó punción guiada, con la cual se evidenció presencia de bilis. En la tomografía axial computada fue evidente la dilatación de la vía biliar. La paciente fue intervenida mediante una laparotomía para resolver ambas dolencias.
ConclusiónEl biloma retroperitoneal, también llamado coleretroperitoneo, es de etiología multifactorial. Su presentación clínica es inespecífica y cursa con distención y dolor abdominal difuso en todos los pacientes. Su diagnóstico se realiza a base de ultrasonografía y tomografía axial computada, e incluso puede ser diagnosticado en el transoperatorio. Su tratamiento se basa en el drenaje del líquido biliar y en la corrección de la fuga.
The term biloma refers to a collection of liquid bile outside the biliary tract, which may or may not be encapsulated.1–3 The condition is associated with rupture of the biliary tract due to trauma, abdominal surgery, duodenal diverticula, or biliary disease, and very occasionally presents spontaneously.3 Non-traumatic spontaneous rupture of the bile ducts can occur extrahepatically or intrahepatically. It can manifest as an intraperitoneal or retroperitoneal collection; the latter does not compromise the peritoneal cavity, as occurred with our patient.
According to Cólović and Persić, the word biloma was first used in 1979 by Gould and Patel.4 However, reports have been found dating back to the 19th century,3 although it is rare and there are few cases in the literature. We present a clinical case and review of the subject.
Clinical caseA 57-year-old woman, whose clinical symptoms started with intense pungent-type pain, irradiating towards the right iliac fossa and lumbar region, of 30 days’ onset. She was managed with proton pump inhibitors, and analgesics. However, the pain worsened, the patient had little tolerance to food, and her general condition deteriorated. Three days earlier the patient had started with jaundice, acholia and choluria, which is when we became involved in the case.
The patient was not known to be a carrier of biliary disease, and had a history of hysteroopherectomy for benign conditions; 2 pregnancies, 2 births; smoker, up to 10 cigarettes per day, no detectable pathological history or relevant family history.
On physical examination we found: normal vital signs, conjunctival jaundice (4+), normally hydrated oral mucosa. Uncompromised cardiopulmonary system, distended abdomen, resistance and induration in the right hemiabdomen, pain on superficial palpation, dullness to percussion and bowel sounds present and normal.
The laboratory tests on admission reported: leukocytes 11.42×103/μl, neutrophils 9.6×103/μl, haemoglobin 12.59g/dl, platelets 738.1×103/μl, glucose 103mg/dl, cholesterol 330mg/dl, LDL 336mg/dl, albumin 2.9g/dl, globulin 4.2g/dl, total bilirubin 13.5mg/dl, direct bilirubin 9.9mg/dl and indirect bilirubin 3.6mg/dl, alkaline phosphatase 1.029IU/l, gamma-glutamyl transpeptidase 1.090IU/l, aspartate aminotransferase 260IU/l and alanine aminotransferase 316IU/l. Prothrombin time 15.6s, partial thromboplastin time 31.4s (amylase and lipase were not performed). General urine test with 4mg/dl bilirubin. The remainder of the results were within normal limits.
Abdominal ultrasound reported choledocolithiasis and perirenal abscess ruptured into the right paracolic gutter.
On arrival at hospital the patient underwent an abdominal ultrasound-guided aspiration of the retroperitoneal fluid, a bile-like fluid was obtained that was sent to the laboratory for culture and gram staining, and was negative for bacteria.
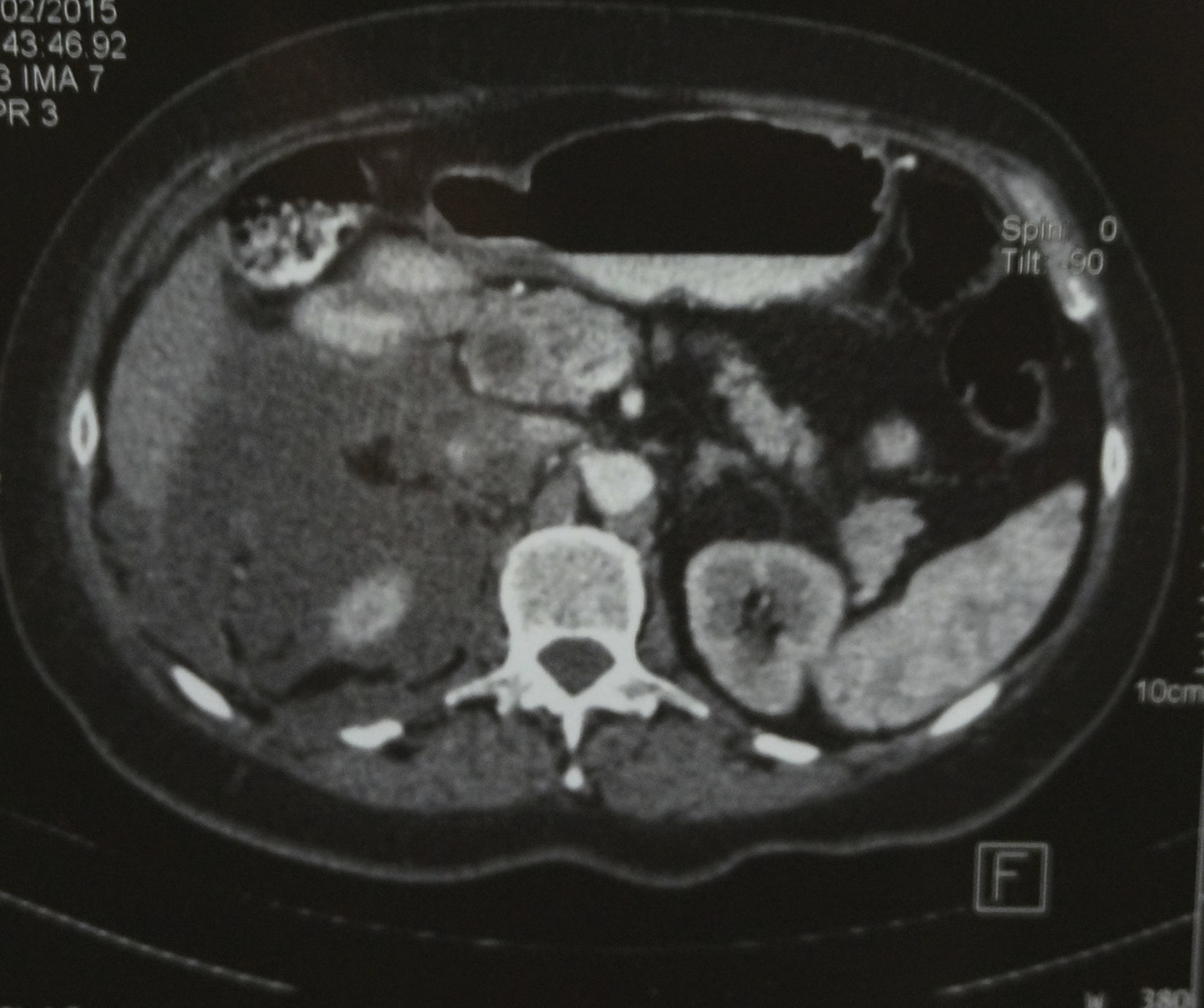
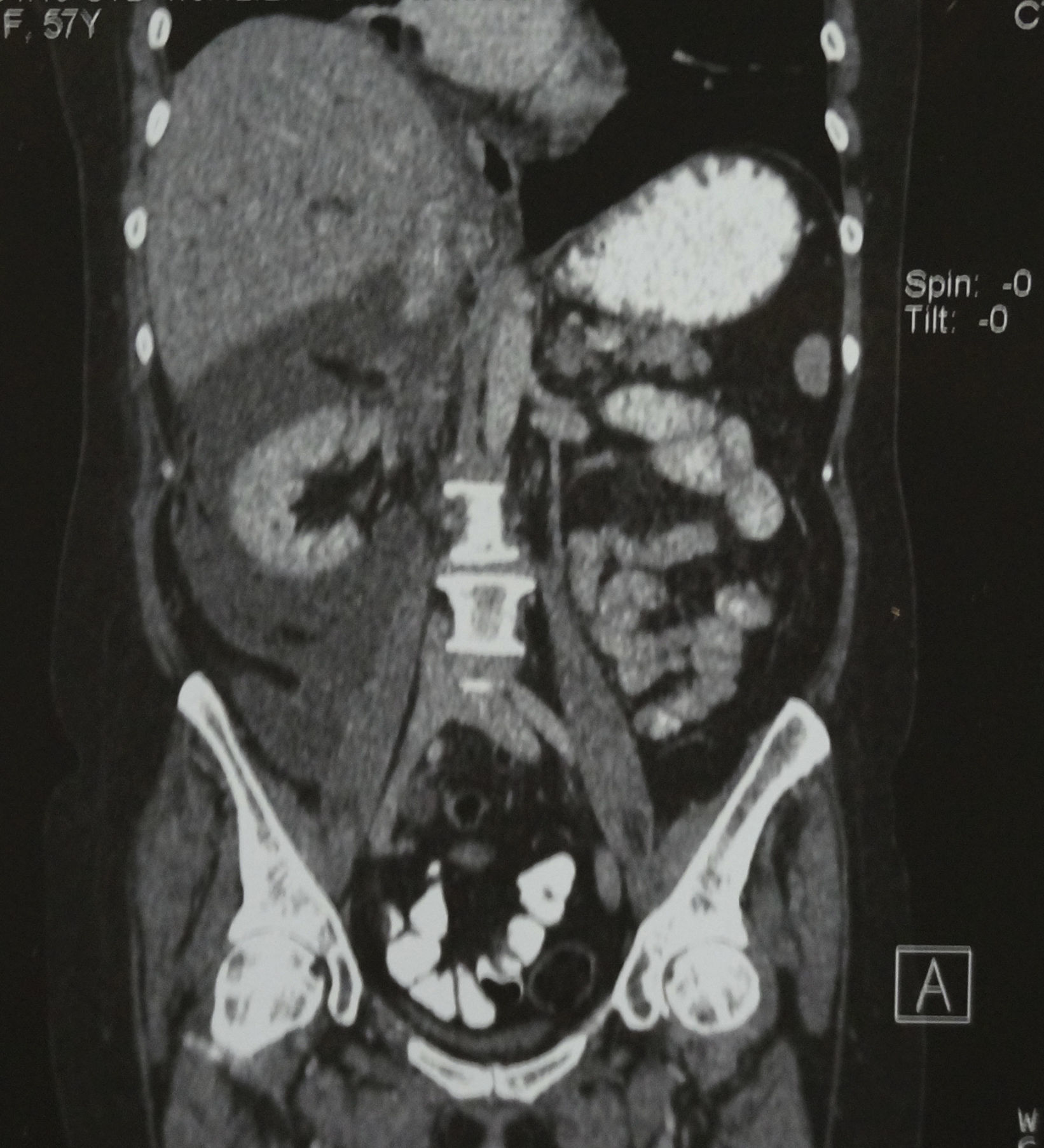
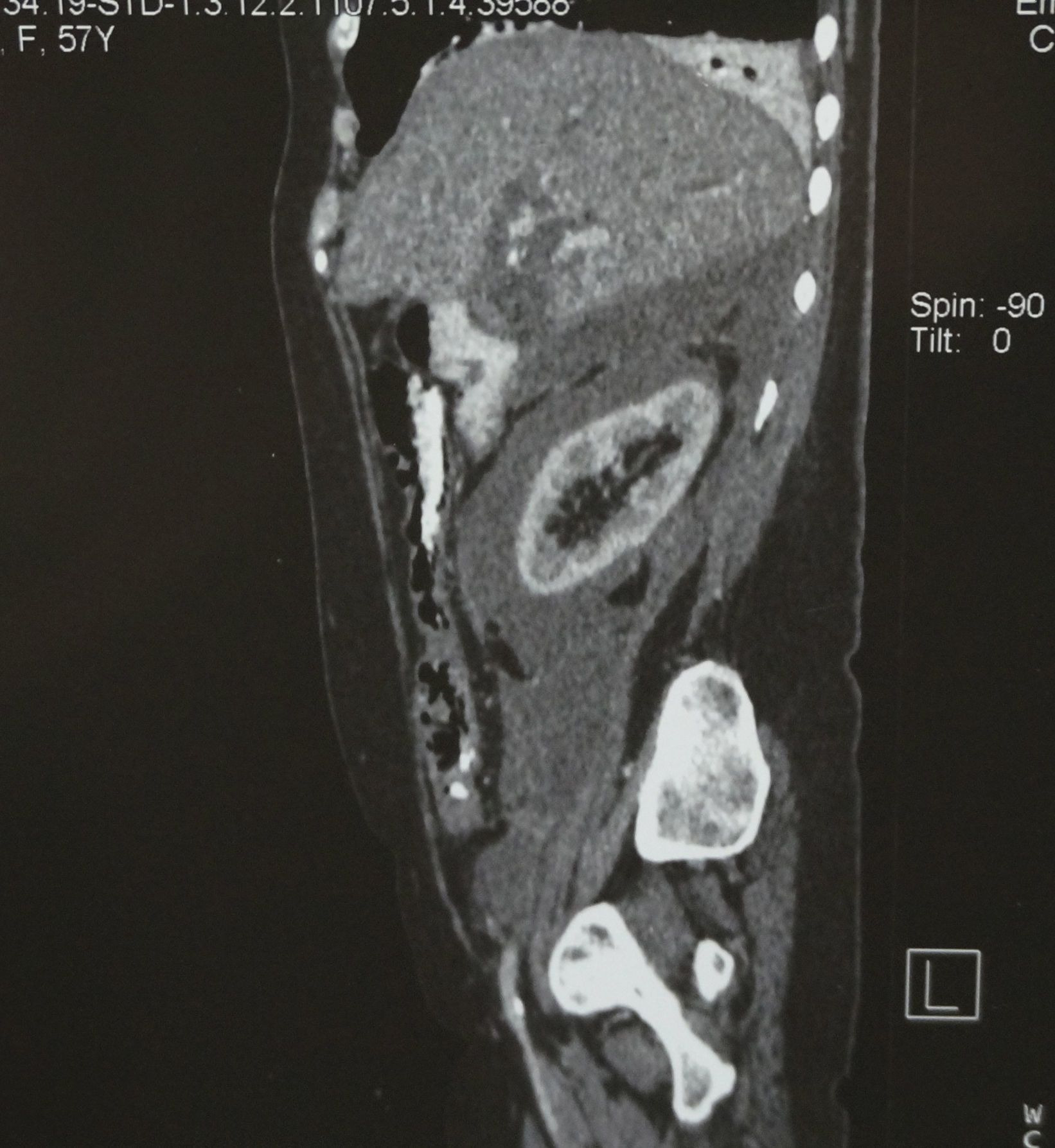
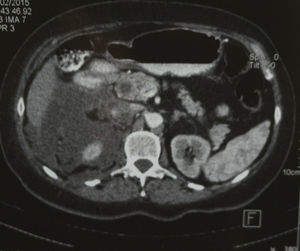
Computed axial tomography revealed marked dilation of the intra and extrahepatic biliary tract, without identifying the gallbladder; in addition, fluid was observed in the anterior and posterior pararenal area (Figs. 1–3).
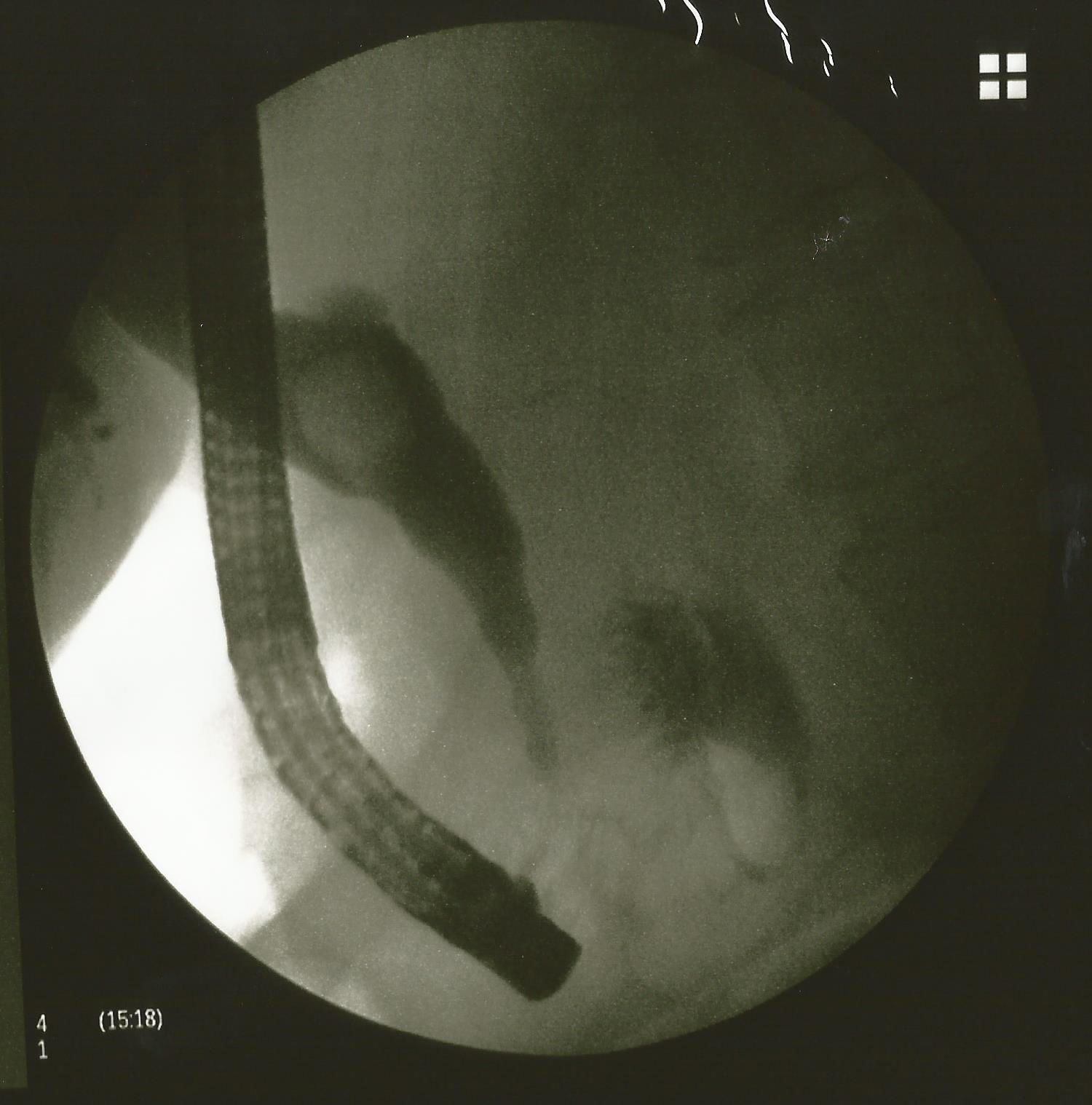
Retrograde endoscopic cholangiopancreatography revealed dilation of the extrapancreatic and common hepatic bile duct, with a large stone inside it. No leakage of contrast was observed and neither could the gallbladder be seen. Due to the large size of the stone, we did not attempt to extract it via this approach. We placed a 10fr biliary endoprosthesis, 10cm in length, to prevent cholangitis (Fig. 4).
A laparotomy was then performed via a right subcostal incision and we approached the peritoneal cavity. We incised the right parieto-colic gutter and the hepatic angle of the colon, to approach the retroperitoneum, from which we drained a clear, greenish fluid. The space that contained the fluid was dissected towards the right iliac fossa and psoas, respecting the pancreatic space.
Using Kocher's manoeuvre, we explored the retroperitoneal portion of the duodenum and the pancreatic head. We were not able to find the site of the bile leakage.
The gallbladder was very small and atrophied, a form of cyst button could be seen (see the retrograde endoscopic cholangiopancreatography in Fig. 4), and therefore we left it as it was.
The biliary tracts were explored, through an incision in the anterior surface of the bile duct, and a large stone, 3cm in diameter, was removed. The endoprosthesis was left in situ, a 16Fr T-tube was placed, and the common bile duct was sutured with chromic catgut suture of 1000.
Two 19Fr Blake closed drains were left in the retroperitoneum, which were exteriorised through a counter opening.
The patient made satisfactory postoperative progress; the drains were removed one week later, with practically no drainage. The T-tube was removed 19 days postoperatively after a control cholangiography, and 4 months later the biliary endoprosthesis was removed.
DiscussionA biliary fluid collection, either encapsulated or otherwise, in the abdomen as a consequence of bile leakage, in any segment of the bile ducts, principally from the extrahepatic segment or directly from the bile canaliculi, is termed biloma. The most common aetiology is surgical, endoscopic and traumatic injuries.5 If the biliary fluid collection is retroperitoneal it is termed choleretroperitoneum.1
This is a rare entity, with few cases reported in the literature. The first case was described in 1882 by Freeman.6 Chu reported 7 cases in 1984, and Sung-Burn et al.,7 reported 11 cases of non-traumatic bile duct perforation over the last 10 years.
In addition to surgical, endoscopic and traumatic injuries, duodenal diverticuli,5 stones lost inside the cavity after cholecystectomy,8 pancreatic cancer,9 perforation of the common bile duct diverticulum10 and chronic pancreatitis11 are also aetiological factors.
It is difficult to determine the aetiology of the event, since it is occasionally not possible to identify the site of the injury. The retroperitoneal portion can be the possible source of the bile leakage,7 this segment also has an intrapancreatic portion.1
Another possible pathophysiological explanation is a perforation in the gallbladder, which through a chronic inflammatory process adheres to the parietal peritoneum that, as it erodes, creates a route of communication between the biliary tract and the retroperitoneum.1
If the aetiology of the perforation is acute pancreatis, necrosis of the intrapancreatic bile duct causes this collection.1
A perivesical abscess, as it erodes the parietal peritoneum, creates a communication between the bladder and the retroperitoneum. The abscesses that form due to free stones within the cavity after cholecystectomy can drain towards the retroperitoneum.8
Despite all the possible pathophysiological explanations, the most accepted is that if there is increased pressure of the bile duct, either caused by a stone obstructing the extrahepatic biliary tract or by a spasm of the sphincter of Oddi, and combined with an infectious process in the duct or perivesical abscess, this results in a perforation in the retroperitoneal segment of the duct. Once the pressure has been released, this millimetre perforation heals in a few hours, and this is why this perforation is not located or corroborated on imaging studies or surgical exploration, resulting in uncertainty and confusion for the medical team.7
Clinically, all patients have abdominal pain and diffuse or localised abdominal distension in the upper right quadrant.10 Most patients have fever and may or may not be jaundiced.
Abdominal ultrasound is the first study that will raise the suspicion of a choleretroperitoneum, since it determines a retroperitoneal and perirenal collection, which can be confused with a renal abscess. Dilatation of the bile duct is observed in most cases.2,12 Needle aspiration of the collection will reveal retroperitoneal bile, and rule out other diseases; however, diagnosis will very often be reached intra-operatively.
Axial computed tomography is essential to evaluate this collection and the integrity of the retroperitoneal organs more accurately.
In children, nuclear medicine with technetium-99 reveals perforation of the bile duct and bile leakage, either to the cavity or the retroperitoneum.13
If diagnosed preoperatively, retrograde endoscopic cholangiopancreatography will reveal dilation of the extrahepatic bile duct, and the presence of one or several stones in the biliary tract. It will be difficult to identify the site of the leakage, since in most cases it will have closed.10
Retroperitoneal collection can be drained by needle aspiration under ultrasound or computed axial tomography guidance,2 leaving a pigtail catheter, or by open or laparoscopic surgery. These will depend on the hospital's available resources.
The stone can be removed by retrograde endoscopic cholangiopancreatography or surgically.12
We performed retrograde endoscopic cholangiopancreatography in our patient. However, the stone was very large, which made extraction difficult; therefore the drainage and extraction of the stone were undertaken under open surgery.
ConclusionInjuries to the biliary tract still pose a diagnostic and therapeutic challenge. Fortunately, the advent of new technologies has facilitated the issue, and patients recover satisfactorily without sequelae, in most cases. This case shows us that if can rule out choledocolithiasis, we are sure to be dealing with a retroperitoneal biloma.
Ethical disclosuresProtection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of dataThe authors declare that they have followed the protocols of their work centre on the publication of patient data.
Right to privacy and informed consent.The authors declare that no patient data appear in this article.
Conflict of interestThe authors have no conflict of interests to declare.
Please cite this article as: Blake-Siemsen JC, Kortright-Farias M. Biloma retroperitoneal espontáneo: reporte de un caso. Cir Cir. 2017;85:552–556.