Pylephlebitis or septic thrombophlebitis of the portal venous system is a rare but serious complication of intra-abdominal infections which drain into the portal venous system. Its diagnosis is based on clinical suspicion and imaging tests, mainly a computed tomography scan, given the lack of specificity of the signs and symptoms. Spread of septic emboli is the major cause of morbidity and mortality.
The aim of the study was to analyse patients diagnosed in our hospital.
Material and methodsRetrospective descriptive study of patients diagnosed with pylephlebitis in our hospital.
Clinical casesFour patients were included, three men and one woman. In three cases it was acute cholecystitis that led to the diagnosis of pylephlebitis at the same time as the intra-abdominal infection. Emergency surgery was performed in one case, whilst the other two were treated conservatively. Blood cultures were performed in all cases, and empirical antibiotic treatment was used. In the only case of acute appendicitis, diagnosis of pylephlebitis was achieved during the study of postoperative fever, with empirical antibiotic treatment also being started. The haematologist was requested to start the required anticoagulation therapy in all cases.
ConclusionsPylephlebitis is a rare complication of intra-abdominal infections that may make lead to a worse outcome. A high level of suspicion is required as well as imaging tests to make an early diagnosis and appropriate treatment.
La pileflebitis o trombosis séptica portal es una complicación poco frecuente pero grave de aquellos procesos infecciosos intraabdominales, cuyo drenaje venoso depende del sistema portal. Su diagnóstico se basa en la sospecha clínica y en las pruebas de imagen, principalmente la tomografía abdominal, dada la inespecificidad de su sintomatología. La principal causa de morbilidad y mortalidad es la diseminación de los émbolos sépticos.
El objetivo de este estudio es analizar los casos diagnosticados en nuestro centro.
Material y métodosEstudio retrospectivo y descriptivo de pacientes diagnosticados de pileflebitis, en nuestro centro.
Casos clínicosSe incluyeron 4 pacientes, 3 varones y una mujer. En 3 casos se trataba de colecistitis aguda, en los que el diagnóstico de pileflebitis se realizó en el mismo momento que el proceso infeccioso intraabdominal. Un caso fue intervenido de forma urgente, mientras que los otros 2 se trataron de forma conservadora. En los 3 casos se realizaron hemocultivos y se inició tratamiento antibiótico empírico. En el único caso de apendicitis el diagnóstico de pileflebitis se realizó durante el estudio de fiebre en el postoperatorio, asociando también tratamiento antibiótico empírico. Se consultó con el servicio de Hematología para valorar la asociación de tratamiento anticoagulante, que fue necesario en todos los casos.
ConclusionesLa pileflebitis es una complicación poco frecuente, que puede acontecer en el contexto de múltiples infecciones intraabdominales, entorpeciendo su evolución. Será necesario un elevado índice de sospecha clínica, junto con la realización de pruebas de imagen para realizar el diagnóstico temprano y el tratamiento oportuno.
Pylephlebitis is septic thrombophlebitis of the portal vein or its tributaries and is a consequence of an intra-abdominal infection which drains into the portal venous system.1 These thrombosed veins may send septic emboli towards the liver and cause hepatic abscesses, generally on the right hand side, due to the blood flow from the superior mesenteric vein towards the right hepatic lobe.2 This complication is infrequent but the rate of mortality is high.3
The condition may adopt several clinical forms, from asymptomatic patients, whose diagnosis is incidental to carrying out an imaging test, to serious symptoms with septic shock and liver failure.4,5 The most frequent symptoms: fever, abdominal pain and even jaundice.6 Laboratory findings most observed are: leucocitosis, increased liver enzymes and changes in coagulation. The most frequently involved aetiological agent is the Bacteroides fragilis (B. fragilis), followed by Escherichia coli (E. coli).7 Diagnosis essentially depends on performing imaging tests, including abdominal scans, which would show the presence of echogenic material inside the vessels lumen or computed tomography which is the method of choice, to identify the different intra-abdominal infectious foci. The Doppler scan is also able to provide information on changes to porto-mesenteric flow.8
The main problem of a patient presenting with pylephlebitis is the uncontrolled infection, rather than the complications derived from the thrombosis. For this reason, once diagnosis has been established, treatment should be initiated using broad spectrum antibiotics, together with surgery in selected cases.9 The antibiotic treatment used will be based on the protocols of each hospital, but must provide protection against gram-negative bacilli and anaerobic bacilli for 4 weeks. If the patient presents with hepatic abscesses, duration would be 6 weeks, together with percutaneous or surgical drainage when required. The role of anticoagulation is controversial since risks remain and complications could arise in up to 20% of patients. The administration of low-molecular-weight heparin is indicated in the case of: extensive or radiological progression of thrombosis, suppurative pylephlebitis, intestinal resection caused by ischaemia secondary to thrombosis or states of hypercoagulability10; in our centre we consulted with the haematology unit for treatment adjustment.
Surgery is based on the treatment of the intra-abdominal infectious foci (appendicectomy, cholycystectomy, etc.), with no involvement of the infected blood vessels.
The aim of this study is to describe the cases of pylephlebitis diagnosed in the Surgical Unit of the Hospital Universitario de San Juan de Alicante, Spain.
Material and methodsA retrospective, descriptive study of a series of patients diagnosed with pylephlebitis was carried out in the Surgical Unit of the Hospital Universitario de San Juan de Alicante (Spain), during a 3 year period (January 1st 2010 to December 31st 2012), with an assigned population of 240,000 inhabitants.
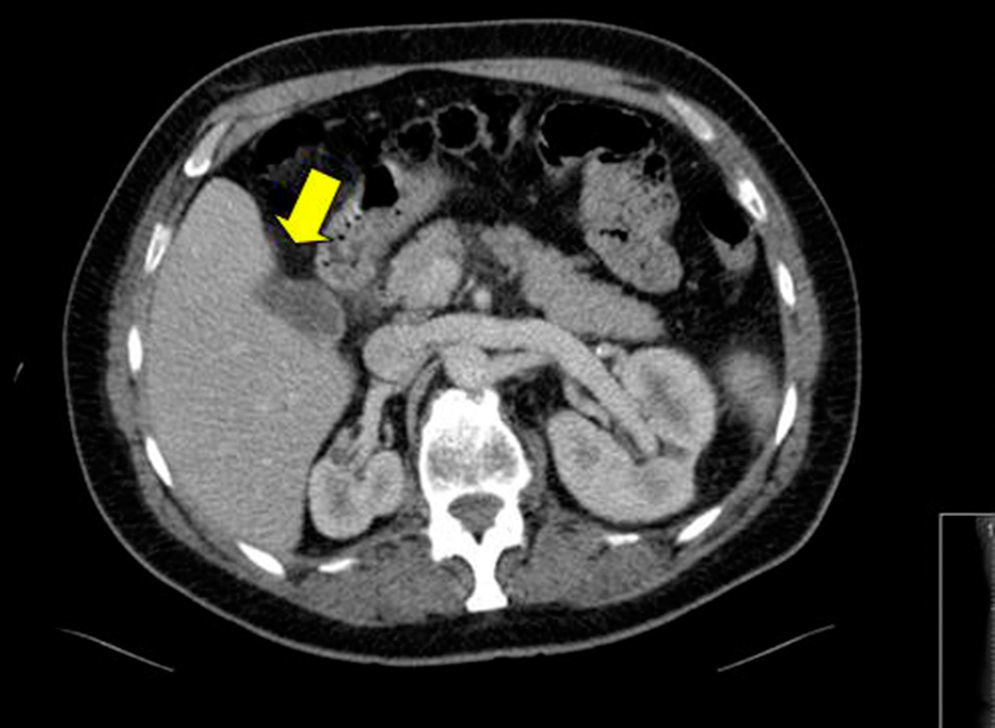
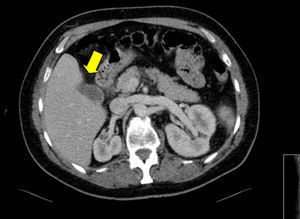
Clinical casesCase 162 year old male with clinical data compatible with acute cholecystitis associated with jaundice and fever, associated with septic thrombosis of the left portal vein, probably septic and secondary to the vesicular inflammatory process, which was confirmed by computed tomography of the abdomen and pelvis (Fig. 1). Emergency cholycystectomy was performed, followed by anti-biotic treatment with amoxycillin clavulanic acid at a dose of 1g/8h and anticoagulant initially with low-molecular-weight heparins, leading to the initiation of oral anticoagulant therapy. Blood cultures tested positive for Klebsiella oxytoca and the bile culture tested positive for Enterococcus faecium; as a result, anticoagulant treatment was maintained for 3 years following surgery, due to the persistence of repletion defects in the left portal vein. In the last abdominal CT scan performed, a major atrophy of the left liver lobe was observed, but with permeable portal vein and anti-coagulation therapy was suspended indefinitely as a result.
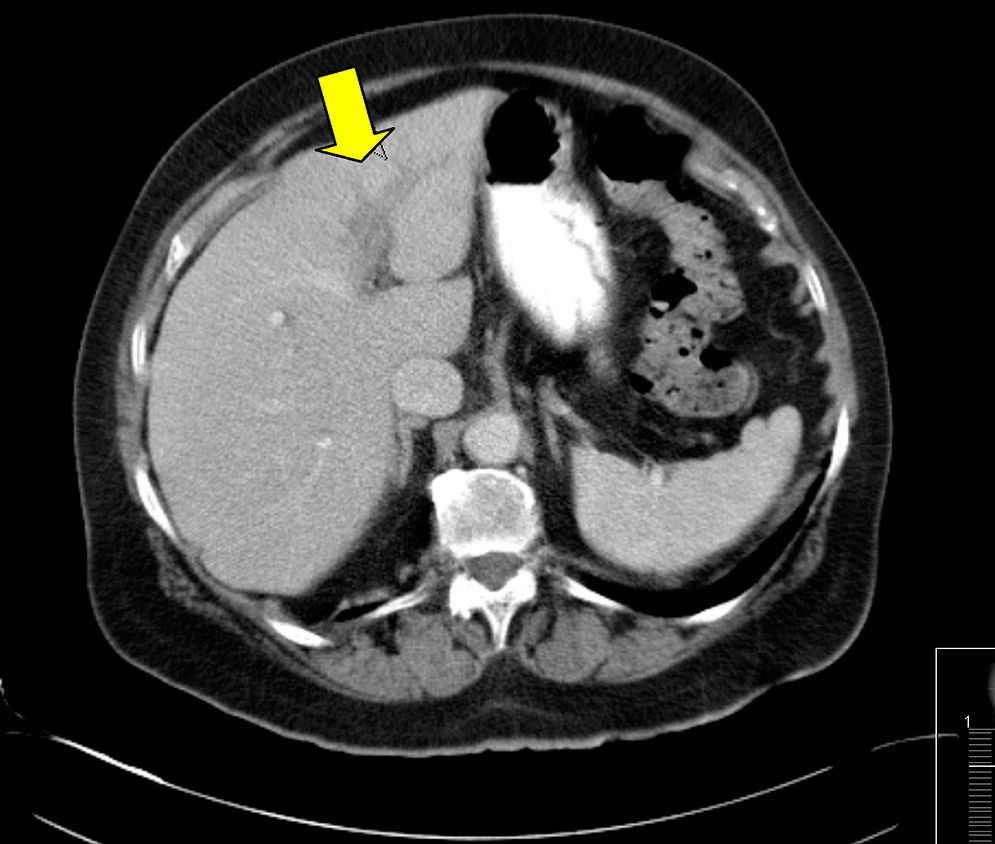
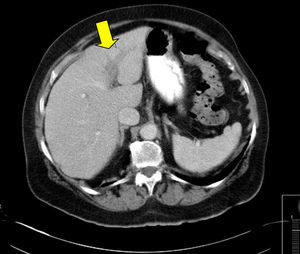
Case 2A 73 year old woman, with high blood pressure presented with an acute cholecystitis of 7-day duration and a diagnosis was made using computed tomography of the abdomen and pelvis; the iodinated contrast scan also revealed repletion defects in the portal system, particularly in the left portal vein, as an expression of venous thrombosis (Fig. 2). Treatment with antibiotics was initiated (piperacillin-tazobactam: 4.5g/8h) and anticoagulation with the same guidelines as in the previous case. Four months after the initial process, a control scan was performed which showed conservative calibre portal vein and permeability at hilum level, bifurcation and nearby portion of right and left branches, which enabled the suspension of the anticoagulant treatment. Cholecystectomy was performed at a later scheduled date, with no further complications.
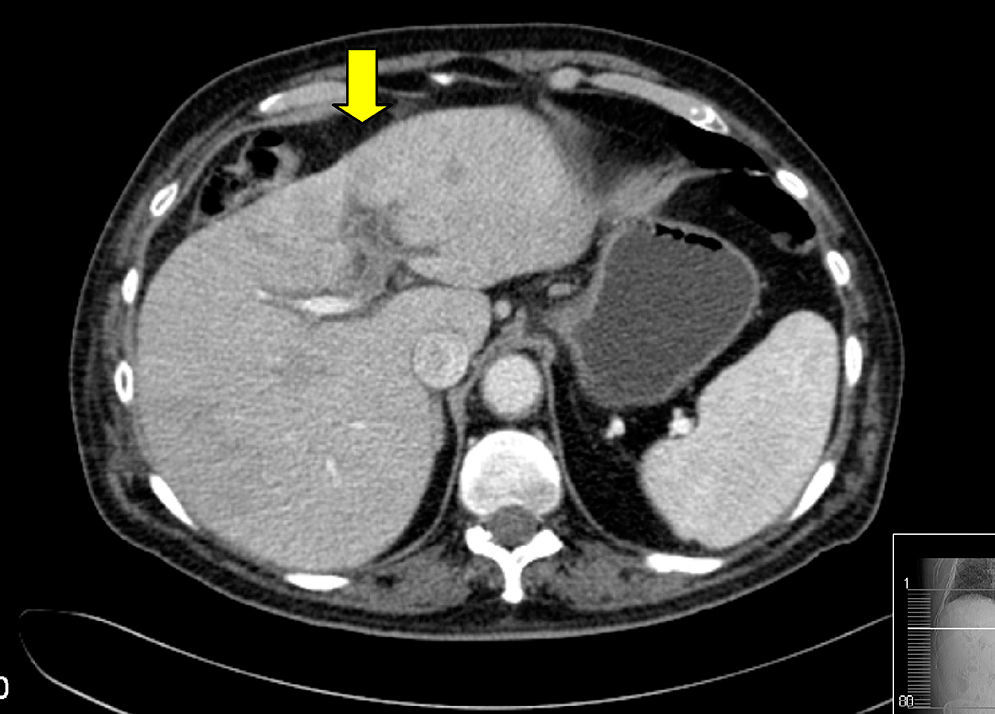
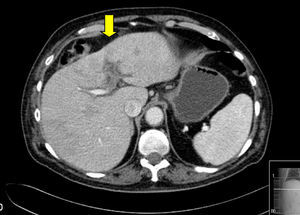
Case 3An 82 year old male, ex-smoker, with symptoms compatible with acute cholecystitis of 4-day duration which was confirmed by computed tomography of the abdomen. The same scan also revealed heterogeneous liver with hypodense areas in segments IV, V and VIII; the left intrahepatic portal vein and its branches appeared to be occupied by hypoattenuating material with enhancement to its walls, findings which were indicative of portal vein thrombosis (Fig. 3). Empirical antibiotic treatment was initiated with piperacillin-tazobactam at a dose of 4.5g/8h, and anticoagulant using low-molecular-weight heparins. Blood cultures were positive for Klebsiella pneumoniae.
The patient evolved favourably and was indicated for a scheduled cholecystectomy but this was suspended due to the patient's clinical deterioration which was not associated with his liver disease.
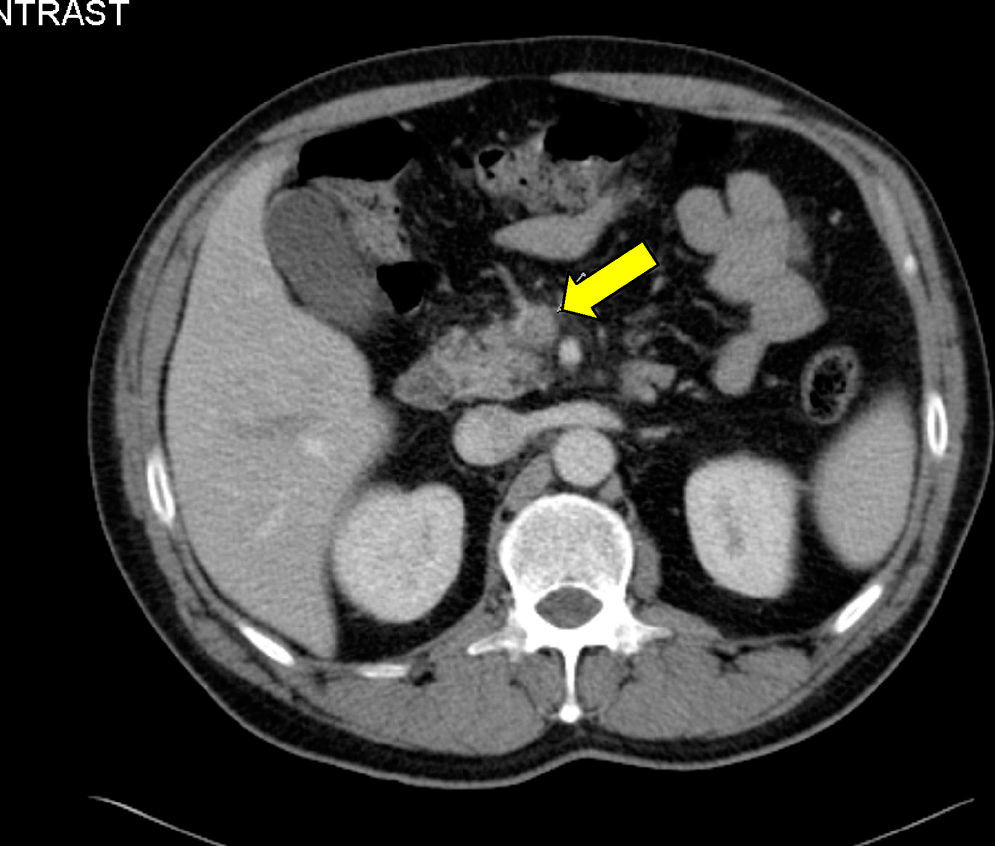
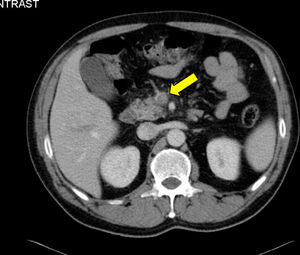
Case 4A 44 year old male, who had undergone surgery for acute gangrenous appendicitis, presented with fever on the 4th postoperative day but with no other clinical symptoms. Computed tomography of the abdomen was performed, which showed repletion defects in the upper mesenteric vein and posterior right portal branches, together with discreet postsurgical post-appendectomy changes, with no free fluid or intra-abdominal collections (Fig. 4) Anticoagulation treatment was initiated with low-molecular-weight heparins and empirical antibiotic therapy with amoxicillin-clavulanic acid of 1g/8h, whilst blood culture results were awaited. These tested positive to Bacteroides caccae; the peritoneal liquid culture tested negative. After 6 months an abdominal CT control scan was performed, where no intraluminal defects were observed in the portal system, and the mesenteric vein tested normal in calibre and permeability. Anticoagulant treatment was therefore suspended.
DiscussionPylephlebitis is an intra-abdominal infectious process the incidence of which has increased in recent years, mainly as a result of the advanced and general use of imaging techniques or abdominal computed tomography.2,3 The major causes of pylephlebitis are acute diverticulitis and appendicitis, although in our series 3 of the cases were caused by a biliary pathological process; in a third of the cases we found idiopathic shapes.4
Symptomatology depends on the degree of thrombosis of the portal vein and its tributaries. Some patients are almost asymptomatic whilst others suffer from serious cases of septic shock and liver failure.5 Only in one of our cases was diagnosis established from clinical suspicion due to symptomatology, which was the appearance of fever in the postoperative period of an acute appendicitis. In the other cases the diagnosis of pylephlebitis was established simultaneously as the intra-abdominal infection by means of imaging studies and was not previously suspected, as symptoms were nonspecific. Medical references consulted also revealed a diversity of opinions in establishing diagnosis, with 4 cases diagnosed postoperatively and another 4 diagnosed at the time of surgery.
The most frequently involved microorganism is B. fragilis, followed by E. coli, unlike our series where it was Klebsiella7.
Treatment of pylephlebitis is mainly based on broad spectrum antibiotic therapy, which must be initiated as early as possible.9 We use amoxycillin-clavulanic acid and piperacilin-tazobactam, as do the Granero-Castro,2 López-Rodríguez,4 and Gajendran et al. series.6 Another key element of treatment is surgery in the case of appendicitis or in patients selected with acute cholycystitis or acute diverticulitis, which enables us to treat the origin of the intra-abdominal infection.
The use of anti-coagulation is controversial, since it is not exempt from complications; in our hospital the Haematology Unit was consulted in this regard.10
Early diagnosis of pylephlebitis is essential for correct treatment initiation leading to reduced mortality rates.
ConclusionsPylephlebitis is a rare, severe complication of intra-abdominal infections, and patient evolution may deteriorate as a result. Imaging techniques are required to reach an early correct diagnosis, which enables us to imitate the most appropriate treatment in each case. This could be anti-coagulation alone or combined with surgical treatment for septic foci drainage.
Conflict of interestsThe authors have no conflict of interests to declare.
Please cite this article as: Pérez-Bru S, Nofuentes-Riera C, García-Marín A, Luri-Prieto P, Morales-Calderón M, García-Garcí S. Pileflebitis: una extraña pero posible complicación de las infecciones intraabdominales. Cir Cir. 2015;83:501–505.