The high frequency of post-operative pain in the patients after laparoscopic cholecystectomy has led to the need to use multiple analgesic therapies. These include auriculotherapy, although not very good results have been obtained with the traditional techniques.
ObjectiveTo evaluate the effectiveness of modified auriculotherapy for post-operative pain control in laparoscopic cholecystectomy patients.
Material and methodsDouble-blind controlled clinical trial. Experimental group: Different points ear puncture with xylocaine without needles vs. placebo group. Post-operative visual analogue scale (VAS) at 6, 12, 18, 24, 36, and 48h and rescue doses of analgesics, were measured in both groups.
ResultsAt 6h post-operative, 87% of the auriculotherapy group had a VAS of <4 vs. 48% of placebo group (p=0.004), and 96 vs. 74% (p=0.008) at 18h. At 24, 36 and 48h after surgery there were no differences, and as all of the patients in both groups had a VAS <4, they were discharged to the hospital.
ConclusionsModified auriculotherapy was better to the conventional analgesics for post-operative pain control in patients subjected to laparoscopic cholecystectomy.
La presencia de dolor en el postoperatorio de la colecistectomía laparoscópica nos obliga al uso de múltiples terapias analgésicas, incluyendo entre todas estas a la auriculoterapia, aunque con la técnica habitual tradicionalmente utilizada se han reportado resultados moderados.
ObjetivoEvaluar la eficacia de la auriculoterapia modificada en el control del dolor postoperatorio en la colecistectomía laparoscópica.
Material y métodosEnsayo clínico controlado doble ciego. Grupo experimental: auriculoterapia con xilocaína sin agujas vs. group placebo. Evaluación de escala visual análoga (EVA) a las 6, 12, 18, 24, 36 y 48h. Medición de analgésico necesario de rescate en ambos groups.
ResultadosA las 6 h, presentaron EVA<4, un 87% del group de auriculoterapia vs. un 48% del group de placebo (p=0.004); a las 18 h, 96 vs. 74% (p=0.008). A las 24, 36 y, 48 h no hubo diferencias, ya que todos los pacientes presentaron EVA<4 o se egresaron.
ConclusiónLa auriculoterapia modificada es superior a la analgesia convencional para el control del dolor en el postoperatorio de pacientes a quienes se les realiza colecistectomía laparoscópica.
Although the first laparoscopic cholecystectomy in humans was performed in 1987 by Mouret,1 it was not until 1992 in the National Institutes of Health Consensus in Bethesda when it was concluded that laparoscopic cholecystectomy was the treatment of choice for cholecistitis.2 Since then the procedure has become rapidly accepted compared with open cholecystectomy, due to the advantages of minimal invasion, which include: less postoperative pain, faster recovery, reduction of hospital stay and lower costs.3–6
However, despite its advantages, laparoscopic cholecystectomy may incur postoperative pain, which is one of the major reasons to prolong hospital stay, readmit patients and for prolonged convalescence.7,8 Many alternatives have been administered to control postoperative pain, such as the administration of preoperative analgesics or local pre-emptive anaesthetic at the insertion sites,9,10 irrigating with xylocaine in the right hemidiaphragm,11 using a different type of gas such as helium (He) instead of CO212 or using CO2 humid and tepid, instead ofcold,13 without any proof of significant efficacy.
Similar to auriculotherapy, acupuncture has been used to control different types of pain, among which the following are of note: headaches, back pain and articular pain.14 The use of auricular therapy for the control of postoperative pain in laparoscopic cholecystectomy has been proven to be effective as reported by King,15 Usichenko16 and Lequang et al.17 in their works, although the use of a modified acupuncture method combined with ear puncture with xylocaine without leaving the needles in place would help patient management for the postoperative period.
ObjectiveTo assess the usefulness of modified auricular acupuncture for the control of postoperative pain, in patients who are treated with laparoscopic cholecystectomy.
Material and methodsA controlled clinical trial was conducted in the Surgery Service of the Central Hospital Ignacio Morones Prieto in the city of San Luis Potosí (Mexico). All patients over 15 years of age, of any gender, and who were willing to participate in the study, scheduled for elective laparoscopic cholecystectomy were included. Patients with clinical, laboratory or ultrasound data regarding acute cholecystitis, biliary obstruction or cholangitis and pancreatitis were excluded, and those who had received premedication with analgesics by any pathway (including during anaesthetic induction), with coagulation conditions, those allergic to ketorolac, and those with kidney failure, or decompensated concomitant diseases (diabetes mellitus, high blood pressure, liver cirrhosis, etc.). Patients who had undergone an open procedure conversion were eliminated, and those treated with complementary surgical procedures in addition to the cholecystectomy (hernioplasty, appendectomy, biopsies of any type, etc.) and patients with intraoperative findings of pancreatitis, gallbladder perforation or vesicular neoplasm. Prior to the cholecystectomy, the patients were randomly assigned to receive auriculotherapy plus conventional rescue analgesia when necessary (group A) or only conventional analgesia when necessary (group B).
All the patients were informed about the puncture procedure in the pinna when surgery had terminated and only those in group A were punctured. In both groups the ear under observation was occluded. A third independent researcher who was unaware to which groups the patients belonged carried out an assessment of the variables, asking the patients about their abdominal pain, or shoulder pain and requesting they quantify the pain intensity using the visual analog scale (VAS). The researcher interviewed each patient 6, 12, 18, 24, 36 and 48h after the operation whilst they were in the hospital and concluded their evaluations when the patient was discharged, when the patient was pain free or gave a VAS score of <4, was walking and tolerated oral foods (concordance analysis, kappa biased=0.96).
This study was registered with the local ethics committee and confidentiality of findings was maintained.
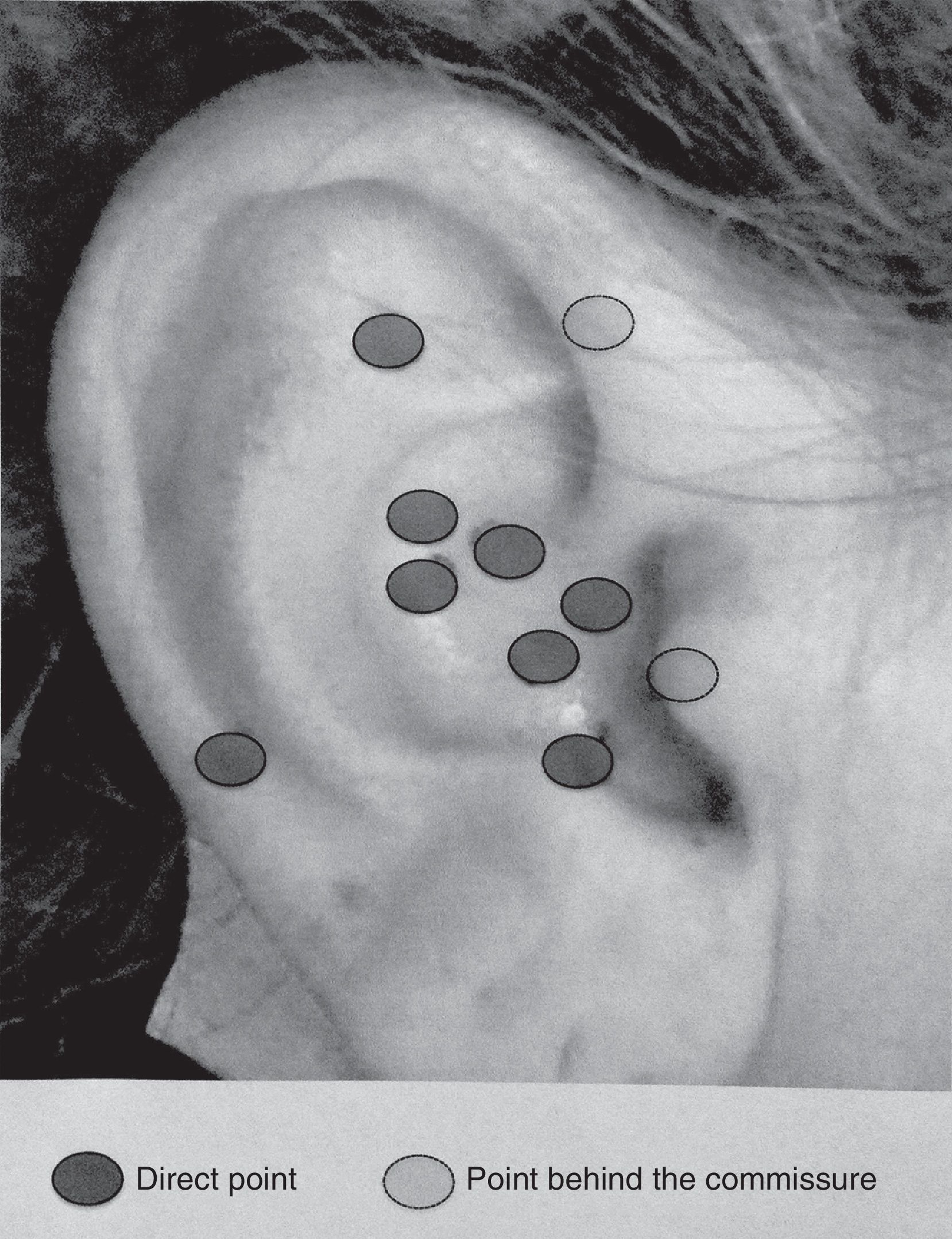
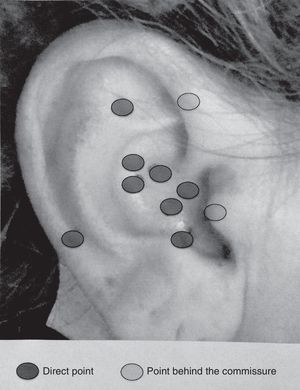
All patients assigned to group A were injected in the key auricular points: abdomen, shoulder, diaphragm, sympathetic nerve, adrenalin glands, hypothalamus, shen-men, stomach, pancreas and gallbladder) by the doctor assigned to surgery or the resident doctor who had been previously trained in the application of these points (Fig. 1). After finalising the laparoscopic cholecystectomy surgical procedure, whilst in the surgery and prior to the patient's extubation, simple 2% xylocaine was prepared, mixed with sterile water to obtain a 1% dilution in a syringe of insulin. Before injection, asepsia of the pinna was carried out with alcohol and 0.1ml was injected into each key point and the ear was covered up. In the patients assigned to group B simulated application was made and the area was also covered up. In those who were administered conventional rescue analgesia, the treatment consisted in the administration of ketorolac at a 30mg dose on each occasion, with as many doses as necessary to control the pain, when the patient stated the pain on the VAS scale was 4 or above in both groups. Demographic data was recorded on all the patients: gender, age, concomitant diseases, length of hospital stay, analgesic dose required and VAS pain scale.
Statistical analysisThis was calculated by measuring the central tendency and dispersion tendency on a variable measurement scale. For bivariate analysis the Mann–Whitney U, Chi-square or exact Fisher tests were used if the expected number was lower than 5. Statistical significance was considered to be a p value under <0.05.
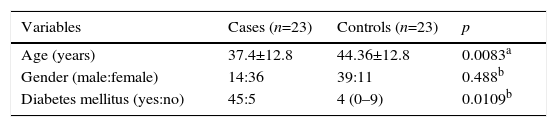
ResultsDuring the study period 46 patients were included who had undergone laparoscopic cholescystectomy: 23 were randomly assigned to group A (auriculotherapy), and 23 to group B (conventional analgesia). Group A included 20 women and 3 men with an average age of 36.9 years. Group B included 17 women and 6 men with an average age of 26.9 years. No significant differences were presented in the review of the socio-demographic data of both study groups (Table 1).
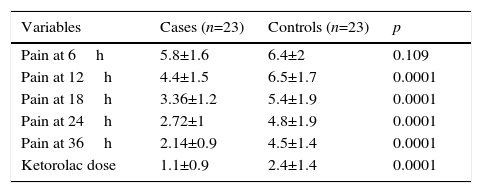
Measurements during the first 6 and 12 postoperative hours showed that 20 patients from the group with auriculotherapy gave a VAS score <4 (87%) which was almost double that observed in the control group, where only 11 patients (48%) gave a VAS score of <4 (p=0.004). However, this difference increased at 18h, since out of the total of the first group VAT <4 was presented in 96% compared with 74% of the second group (p=0.008). At 24, 36 and 48 hours there were no differences, since all patients presented VAS at <4 or were discharged (Table 2).
Comparison between degree of pain (VAS) by study group.
| Variables | Cases (n=23) | Controls (n=23) | p |
|---|---|---|---|
| Pain at 6h | 5.8±1.6 | 6.4±2 | 0.109 |
| Pain at 12h | 4.4±1.5 | 6.5±1.7 | 0.0001 |
| Pain at 18h | 3.36±1.2 | 5.4±1.9 | 0.0001 |
| Pain at 24h | 2.72±1 | 4.8±1.9 | 0.0001 |
| Pain at 36h | 2.14±0.9 | 4.5±1.4 | 0.0001 |
| Ketorolac dose | 1.1±0.9 | 2.4±1.4 | 0.0001 |
Mann–Whitney U test.
The average accumulated dose of analgesic administered to the patients in group A was significantly lower than that administered in group B: 1.1±0.9 vs. 2.4±1.4 dose/day in the first 24h after the operation (p=0.0001) and no difference after 48h. No collateral effects associated with intervention were recorded.
DiscussionAlthough laparoscopic cholecystectomy is a minimally invasive procedure which produces notable advantages in patient recovery, as it is regularly associated with less pain, this symptom continues to be a problem in some patient management,7,8 since immediate postoperative pain is the cause of a longer hospital stay and readmittance of the patient who has had a laparoscopic cholecystectomy.18,19 Maximum peak in intensity is within the first 4–8h after intervention although in the following 24h the pain continues being appreciable in a third of all patients operated on.20,21
There are 3 components in postoperative pain which differ in intensity and physiopathological mechanism: the parietal component which correspond to pain of the wound; the visceral component which corresponds to the intra-abdominal pain due to irritation, injury or traction of the parietal peritoneum and shoulder pain, probably from the before-mentioned visceral pain or radiated. It has thus been determined that the postoperative mechanism of pain is mainly due to visceral irritation of the hepatic site which leads to intense pain for the first 24h after an operation. This pain increases with the cough reflex of the patient caused by the descent of the liver, but is not changed by body movement, unlike the parietal pain that presents in conventional laparoscopic cholecystectomy.22
Alternative and complementary medicine refers to practices for therapeutic purposes which veer away from conventional medicine and which may be used alone or concomitantly with mainstream medicine.23 Alternative medicine consists of and uses treatments and remedies which are perceived as being less toxic or harmful than allopathic treatments. These practices have led to scepticism and are commonly not accepted or rarely included in research and teaching of the conventionally established scientific medicine.24 However, alternative medicine is increasingly used and several doctors have shown that these therapeutic interventions are highly accepted by the population in general.25 Alternative medicine has recently been the object of well-designed studies and systematic analysis which have proven their potential usefulness in clinical practice.26,27
One of the best studied alternative medicine techniques and with the greatest therapeutic potential in the area of pain control is auricular acupuncture.28,29 Auricular acupuncture is defined as a form of body stimulation whereby several points of the ear are punctured to obtain a certain effect on the body.30 This technique has undergone many changes. At present it uses electronic instruments, magnetic fields, the application of minor drug doses and different types of laser, evolving to what is called “auricular medicine”.31
Our study has demonstrated the effectiveness of this technique with modification from its traditional form for the control of postsurgical pain in patients who have undergone laparoscopic cholecystectomy, since the efficacy of traditional methods with analgesics is often lower than that observed here. Equally, the findings previously reported with the regular non modified auriculotherapy had only demonstrated an efficacy of 66% after 6 and 12h, which is lower than that reported here.
ConclusionsDue to the above, we propose that this technique be used as an alternative in the treatment of postoperative pain in the patient who has undergone laparoscopic cholecystectomy. We therefore consider that this therapeutic alternative may enable the application of low cost intervention and one which is not associated with serious adverse effects in patients at risk or with the contraindications from NSAIDS usage.
Ethical disclosuresProtection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of dataThe authors declare that they have followed the protocols of their work center on the publication of patient data.
Right to privacy and informed consentThe authors declare that no patient data appear in this article.
Conflict of interestsThe authors have no conflict of interests to declare.
Please cite this article as: Toca-Villegas J, Esmer-Sánchez D, García-Narváez J, Sánchez-Aguilar M, Hernández-Sierra JF. Eficacia de la auriculoterapia modificada como tratamiento para el control del dolor postoperatorio en pacientes intervenidos mediante colecistectomía laparoscópica. Cir Cir. 2017;85:220–224.