Intramuscular myxoma is a rare benign soft tissue tumour of mesenchymal origin, which appears as a painless mass of slow growth. Early diagnosis is important in order to differentiate it from other entities, especially soft tissue sarcoma.
Clinical casesTwo cases, both women with a mean age of 52.5 years (range 40–65) are presented. The first was seen due to growth of a gluteal mass, and the second by coccydynia. Computed tomography and nuclear magnetic resonance were the diagnostic tests of choice. In one case, where there was a single but large lesion, radical extirpation of the gluteal muscle was chosen. In the other case, in which the lesions were multiple, individualised excision of cysts was performed. Postoperative functional limitation was low in both types of surgery, with good oncological results being obtained.
ConclusionIntramuscular myxomas are benign lesions. There are no cases of malignancy or recurrence due to incomplete resection. It has to be determined whether they are single or multiple, since in the latter case, they could be due to syndromes such as Mazabraud syndrome, which is associated with bone fibrous dysplasia, or Albright syndrome that is also associated with pigmented skin spots.
El mixoma intramuscular es un tumor benigno poco frecuente de tejidos blandos, de origen mesenquimal, que se presenta como una masa de crecimiento lento, indolora. Es importante el diagnóstico precoz para diferenciarla de otras entidades, especialmente del sarcoma de partes blandas.
Casos clínicosSe presentan 2 casos clínicos, ambos de mujeres con una edad media de 52.5 años (rango 40-65). La primera acudió por crecimiento de masa glútea y la segunda por coccigodinia. La tomografía computada y la resonancia magnética nuclear fueron las pruebas diagnósticas de elección. En un caso, en el que la lesión era única pero de gran tamaño, se optó por la glutectomía radical; en el otro caso, en el que las lesiones eran múltiples, se llevó a cabo la exéresis individualizada de los quistes. La limitación funcional postoperatoria fue escasa en los 2 tipos de cirugía, con buenos resultados oncológicos.
ConclusiónLos mixomas intramusculares son lesiones benignas, no existen casos de malignización y su recurrencia se debe a resección incompleta. Hay que diferenciar si son únicos o múltiples, ya que, en este último caso, pueden englobarse en síndromes como el de Mazabraud, que se asocia con displasia fibrosa ósea, o al síndrome de Albright, que se asocia además con manchas pigmentadas cutáneas.
Intramuscular myxoma is a soft tissue tumour of mesenchymal origin, of unknown aetiology. It is rare, with an incidence of between 0.1 and 0.13 in every 100,000 individuals. Onset is usually between the fourth and seventh decades of life, predominantly in women (70%).1
It most frequently affects the upper extremities (shoulder and arm), the thighs and gluteal muscles.2 It has also been described in other regions such as the deltoid muscle, scapular region, abdominal wall or paravertebral muscles, amongst others.
It usually presents as a solitary tumour, although there are multiple myxomas that are often associated with other entities, forming interesting syndromes.
The aim of our study was to describe 2 clinical cases of intramuscular myxoma, single and multiple, looking at the differential diagnosis, treatment and anatomopathological study. These premises are far-reaching, since myxomas can be confused with malignant lesions or can lead to a poor diagnosis and incomplete treatment if we are unaware of their association with other disorders with which they form syndromes.
Clinical casesClinical case 1A 65-year-old female patient with no history of interest, consulting with a left gluteal mass which had developed over the course of several years. On examination, a round, painless, immovable mass of around 12cm was found within the musculature.
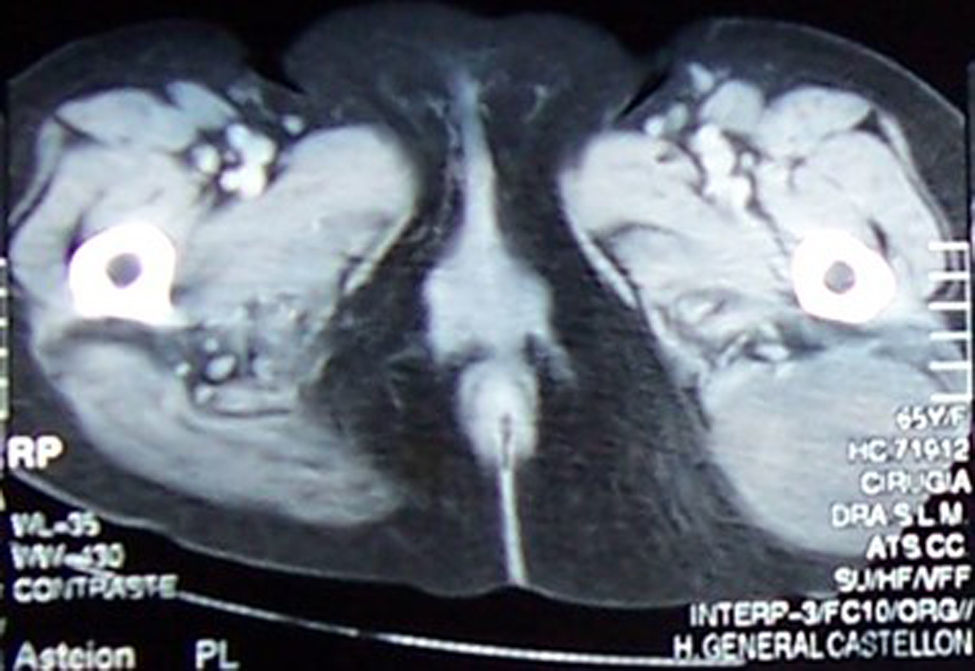
Ultrasound described a well-defined solid lesion in the external caudal face of the gluteus maximus, with characteristics of a possible sarcoma. There was no bone or joint involvement. The study was completed with computed tomography (CAT) (Fig. 1), showing a well-defined mass of 8cm×6cm, hypodense with no enhancement after injection of contrast inside the gluteus maximus, and with nuclear magnetic resonance (NMR) (Fig. 2), which confirmed these findings.
An incisional biopsy was performed of the lesion reporting a myxoid tumour with no signs of malignancy. However, because the myxoid substance and the areas of hypercellularity and hypervascularity made differential diagnosis with myxoid sarcomas difficult and because the imaging tests did not rule out malignancy, surgical intervention was decided.
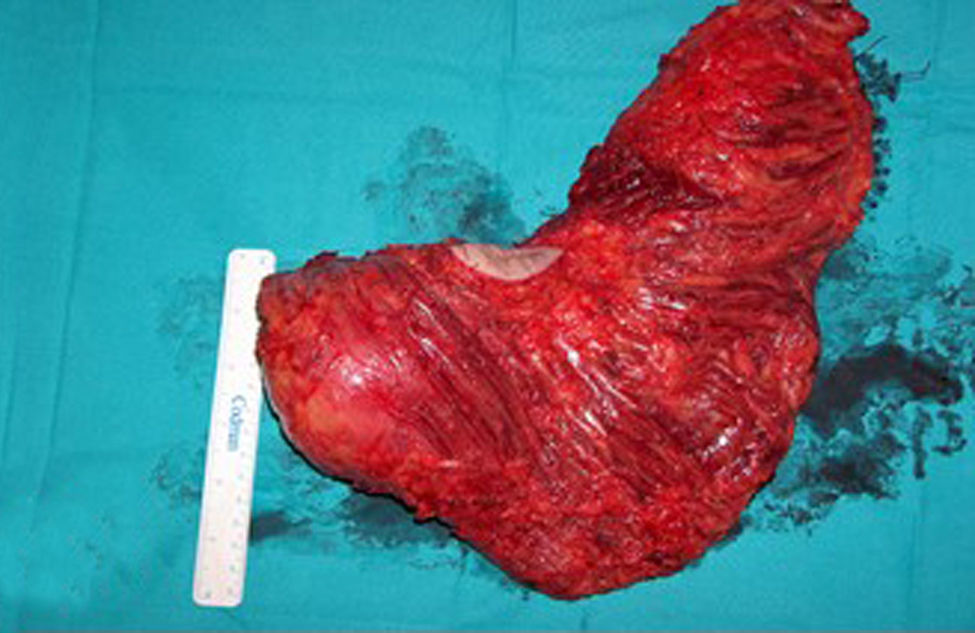
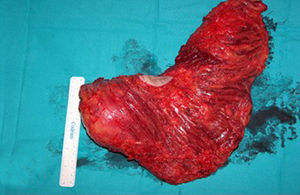
The treatment of choice was radical glutectomy, due to the location and size of the mass (Fig. 3).
The anatomopathological result of the surgical piece was a pseudo-encapsulated intramuscular myxoma.
Seven days postoperatively there were no complications and the patient was mobile.
Clinical case 2A 40-year-old female patient consulted with coccygodynia and left shoulder pain, over the course of several months, and no personal history of interest.
No pathological signs were found on physical examination. Plain hip and knee X-rays were performed, which were normal. Therefore conservative treatment with analgesia was prescribed.
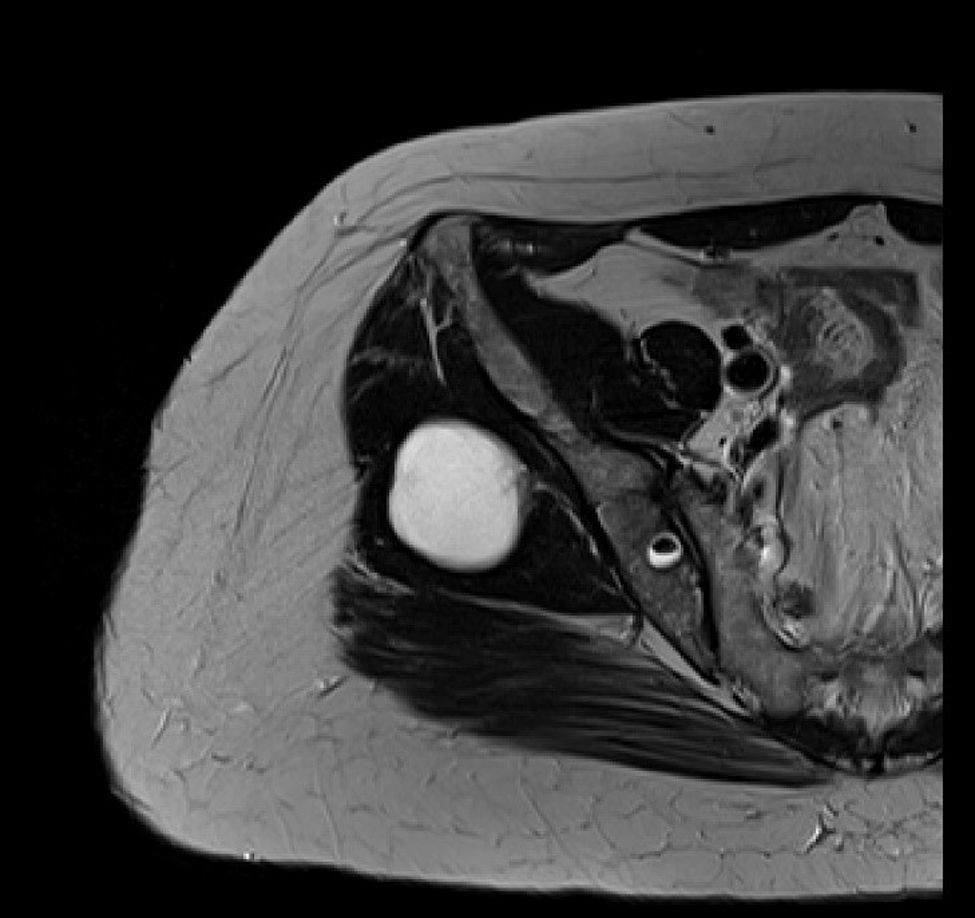
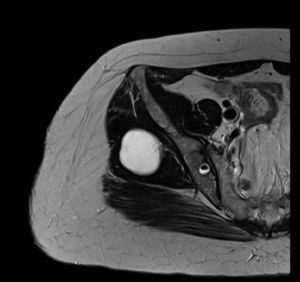
Because the symptoms persisted a left knee and back MRI scan was performed. At the level of the pelvis multiple intramuscular cystic lesions from between 14mm and 52mm were found, located in the right gluteus medius and maximus. These lesions were between the muscle fibres, displacing them, and there were no signs of infiltration (Fig. 4). The left knee showed an oblique tear where the body joined the posterior horn of the inner meniscus, which could be seen on the coronal plane, with no associated chondropathy.
The radiological characteristics of these lesions were compatible with hydatidic cysts, and therefore the study was completed with a CAT scan and serology. The CAT scan confirmed the intramuscular cystic lesions in the right gluteal muscles and revealed a further small (16mm) cystic lesion of smooth contours and defined borders at the level of the mesenteric fat anterior to the ascending colon but not contacting it, which might be another hydatidic cyst. Serology was negative for hydatidosis.
Because radiologically the lesions had the appearance of hydatidic cysts, treatment with albendazol was initiated despite the serology results. However, after 6 months, the patient's pain continued and she experienced discomfort on walking. Therefore, surgical intervention was decided to remove the cysts.
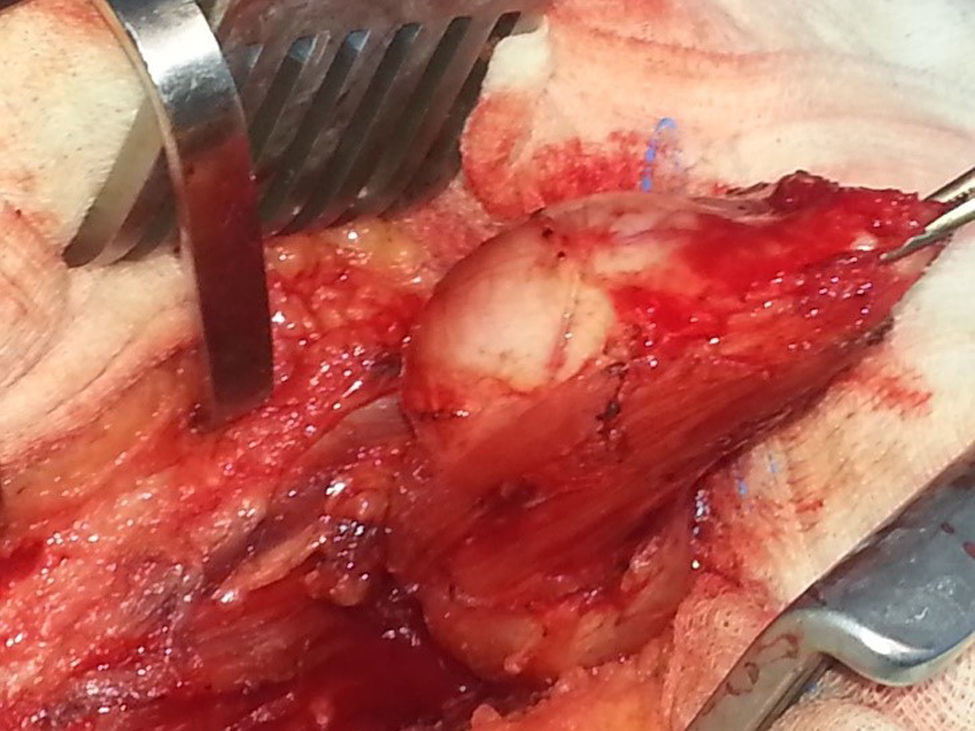
The patient was scheduled for surgery. She was placed in the left lateral decubitus position and the cysts were accessed via a longitudinal incision in the right thigh. The cysts were intramuscular in the gluteus maximus and gluteus medius and were removed with ease (Fig. 5). Their macroscopic appearance was not suggestive of hydatidic cysts (Fig. 6). An ultrasound was performed during the operation to locate the smallest cysts and achieve complete removal. A total of 7 cysts were removed.
Anatomopathological study described the lesions as multiple intramuscular myxomas in the context of Mazabraud's syndrome, taking into account that the characteristic bone lesions can present before the myxomas or appear subsequently.
Given the anatomopathological results, a complete radiological study was undertaken to locate bone dysplasias, but there were no pathological findings.
The patient was discharged after 5 days with no immediate complications and adequate right lower limb function.
In subsequent visits to the outpatient clinic, the intra-abdominal lesion was monitored and the patient was checked for any subsequent bone dysplasias, with periodic repetition of plain X-rays.
DiscussionThe term myxoma was introduced in 1863 by Virchow to describe a mesenchymal tumour, which histologically resembles the umbilical cord, with no other differentiation.3 According to Murphey et al.,4 the histological criteria for diagnosing a myxoma were established by Stout in 1948, who defined myxoma as “a true neoplasm composed of a paucity of stellate cells in a loose myxoid stroma of reticulin and collagen fibres”.
These are very rare tumours, whose aetiology is unknown, they have no predilection for race and no clear hereditary pattern. Onset is between the fourth and seventh decades of live, generally in females.5 This coincides with the features of our patients.
Myxomas that arise from the skeletal muscle are termed intramuscular myxomas and were described by Erzinger and Weiss in 1965.6 The most common location is the long muscles of the upper extremities (50%–60%).7 Their appearing in the gluteal muscles, as in one of our cases, is not unusual and this together with the pelvis, is the second most common location.
The most common form of presentation is as a single lesion, although there are cases of multiple myxomas that are usually associated with other entities, forming interesting clinicopathological pictures.
Mazabraud's syndrome8 is defined as the association of multiple intramuscular myxomas and fibrous bone dysplasia, which can be mono or poly-ostotic. In our second case, this syndrome was the main suspected diagnosis, although we did not identify bone lesions for definitive confirmation. It should not be forgotten that they can appear subsequently, so monitoring by X-ray is essential, since, unlike myxomas, fibrous bone dysplasias can become malignant. McCune-Albright9 syndrome is another disorder to consider. This condition consists of multiple myxomas, polyostotic fibrous dysplasia, café-au-lait spots and endocrine hyperfunction (precocious puberty).
This is a slow-growing tumour, which usually presents as a painless, firm and mobile mass. If there is pain, this is caused by compression of the surrounding structures, as described in some cases in the literature.7
The imaging tests necessary for diagnosis are plain X-ray, CAT and MRI. X-rays tend to be normal, CAT and MRI show characteristic findings, including the intramuscular location, tissue borders similar to fat and high water content. Thus it presents attenuated on CAT, hypointense in T1-weighted images and hyperintense in T2-weighted images.10
Histological diagnosis is recommended with fine needle aspiration or open-sky biopsy, prior to surgery.11 Although as we saw in the first case, this test is not definitive.
Treatment is wide resection of the lesions. Some authors prefer a more conservative approach for small masses, since these are benign lesions, and do not remove a mass until it becomes painful or large. In the first of our patients we opted for more aggressive treatment due to the size of the lesion, while in the second we chose to remove the lesions individually. There are no articles in the literature that describe the onset of metastases or malignancy. Cases of recurrence are due to enucleation or incomplete resection.12
Macroscopically, these are soft, ovoid or globular masses, dependent on collagen and myxoid material, gelatinous, occasionally with cystic spaces filled with fluid, and covered by skeletal skeletal muscle bundles or fascial tissue.
Cytologically, they are characterised by their myxoid base and scant and benign cellularity. However, they should be differentiated from other entities of myxoid origin, either benign (nodular fasciitis, neurotecoma) or malignant (lyposarcoma, fibrohistiocytoma, myxoid chondrosarcoma), and from intramuscular metastases of mucinous adenocarcinomas.
ConclusionsThis is a very rare mesenchymal tumour, of unknown aetiology, which appears in the long muscles of the upper extremities or pelvis. It is usually a single lesion, but the presence of multiple lesions could suggest part of a syndrome. Treatment is surgery, there is no risk of malignancy, and recurrence is due to incomplete excision of the lesion. The definitive diagnosis is anatomopathological.
Ethical disclosuresProtection of human and animal subjectsThe authors declare that the procedures followed were in accordance with the regulations of the relevant clinical research ethics committee and with those of the Code of Ethics of the World Medical Association (Declaration of Helsinki).
Confidentiality of dataThe authors declare that they have followed the protocols of their work center on the publication of patient data.
Right to privacy and informed consentThe authors have obtained the written informed consent of the patients or subjects mentioned in the article. The corresponding author is in possession of this document.
Conflict of interestsThe authors have no conflict of interests to declare.
Please cite this article as: Granel-Villach L, Alcalde-Sánchez M, Salvador-Marín M, García-Calvo R, Santonja-López N, Salvador-Sanchís JL. Diagnóstico diferencial y manejo de mixomas intramusculares: revisión de nuestra experiencia. Cir Cir. 2017;85:356–360.