Pancreatic diseases such as cancer, idiopathic recurrent pancreatitis, and chronic pancreatitis, can cause pain that is difficult to control. Pain is one of the most debilitating symptoms and demands increasing doses of analgesics and narcotics, as well as the number of hospital admissions, with a direct implication in the costs of medical treatments.
ObjectiveTo describe the experience with 2 paediatric patients who were subjected to an ultrasound-guided endoscopic celiac ganglion block for difficult pain management, secondary to chronic pancreatitis disease.
Clinical casesThe first case concerns a 9-year-old male with a diagnosis of chronic pancreatitis, and the second case is a 12-year-old female who developed episodes of intermittent acute pancreatitis. Both cases suffered from chronic abdominal pain, which was difficult to control with stronger painkillers, such as opioids. The pain decreased after patients were subjected to an ultrasound-guided endoscopic celiac ganglion block.
ConclusionsThis technique showed that both patients obtained satisfactory pain relief, with significant improvements in general symptomatology and the stopping of almost all analgesic medication. The authors suggest that celiac ganglion block must be considered, and implemented early before the usual complications, such as a consumption syndrome that is frequent in paediatric patients with chronic pancreatitis.
Las enfermedades pancreáticas como el cáncer, la pancreatitis recurrente idiopática y la pancreatitis crónica pueden causar dolor de difícil control. El dolor es uno de los síntomas más debilitantes para los pacientes y demanda el incremento, tanto de analgésicos y narcóticos, como de la cantidad de ingresos hospitalarios, con implicación directa en los costos.
ObjetivoDescribir la experiencia de 2 pacientes pediátricos que fueron tratados mediante un bloqueo del ganglio celiaco guiado por ultrasonido endoscópico, para el tratamiento de dolor de difícil control secundario a pancreatitis crónica.
Casos clínicosEl primer caso se trata de un paciente masculino de 9 años de edad con diagnóstico de pancreatitis crónica. El segundo caso es una mujer de 12 años de edad que cursó con cuadros de pancreatitis aguda intermitente. Ambos casos presentaron dolor crónico abdominal de larga evolución y de difícil control con analgésicos potentes del tipo opioide. El dolor remitió posteriormente a que los pacientes fueran tratados mediante un bloqueo del ganglio celiaco.
ConclusionesMediante el bloqueo del ganglio celiaco, ambos pacientes obtuvieron resultados analgésicos satisfactorios, con mejoras importantes de la sintomatología en general y la suspensión casi en su totalidad de la medicación. Los autores proponen que el bloqueo del ganglio celiaco sea considerado e implementado de forma temprana antes de que se presenten complicaciones, como el síndrome consuntivo que es frecuente en pacientes pediátricos con pancreatitis crónica.
Patients with chronic pancreatitis seek medical care for abdominal pain or symptoms of bad digestion, such as chronic diarrhoea, steatorrhea, weight loss and fatigue.1
Patients with chronic pancreatitis who present with pain state that it may be constant, intermittent and with occasional pain-free interludes. It has also been observed that eating exacerbates pain, which is why some patients even avoid eating so as not to feel pain, with consequent weight loss and physical impairment, that may even lead to wasting.2
The complexity and intensity of pain makes it difficult to control, which may trigger dependence on non steroid anti-inflammatory drugs (NSAID), and even narcotics. Several mechanisms have been described which explain pancreatic pain, for example: infiltration and inflammation of nerve sheaths and neural lymph nodes, increase in ductal and interstitial pressure, ulceration and secretion of neurolytic enzymes inside the pancreas, ischaemia and inflammation of the gland capsule, distal pancreatic stones or gallstones, sphincter stenosis and the presence of pseudocyst.3
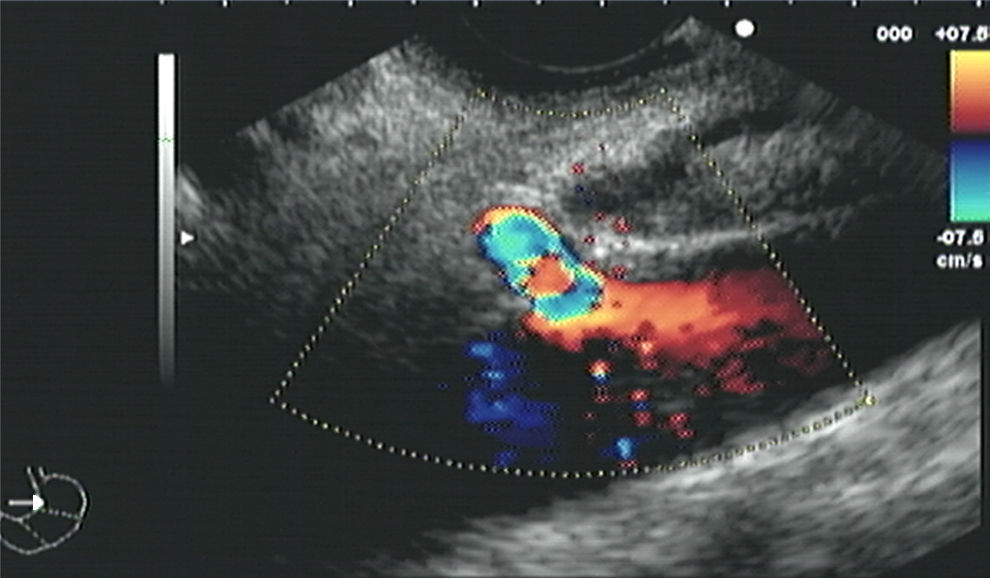
Pancreatic pain is transmitted through the celiac plexus block which primarily contains sympathetic nerve fibres in a neural structure located in the upper half of the abdomen, which is anterior to the diaphragmatic cruris, slightly anterior and cephalic to the arterial celiac trunk, and opposite the vertebral bodies at levels T12 to L2; their posterior limit is L1 and the kidneys; lateral limits are the suprarenal glands and the inferior vena cava to the right and anterior pancreas4 (Figs. 1 and 2).
When pain does not respond to drugs or they lead to side effects such as nausea, constipation, anorexia, somnolence, confusion, dependence and addiction, a nerve block with alcohol may be administered which acts directly on the nerves that convey the painful stimuli from the diseased pancreas to the brain. The celiac trunk, splanchnic nerves or celiac ganglions are thus blocked.5
The splanchnic nerves which cross over the diaphragm, enter the abdominal cavity and form the celiac plexus also play a part in pancreatic pain. They may be reached percutaneously using a needle through the lumbar wall with a posterior approach or trans-abdominally with an anterior approach guided by computed tomography or ultrasound. With the advent of endoscopic ultrasound (EUS) new therapeutic applications have been developed for ultrasound and it is now possible to safely guide a needle towards the celiac plexus using a transgastric anterior approach.6
ObjectiveTo describe the experience and clinical evolution of 2 paediatric patients who were treated with celiac ganglion block guided by EUS, for the management of pain which was difficult to control, secondary to chronic pancreatitis.
Clinical casesCase 1Male patient aged 9, who weighed 35kg and had a history of psychomotor delay and seizures.
At the age of 7 he presented with his first acute complicated pancreatitis with a pseudocyst located at the head of the pancreas. Evolution was torpid, with 5 episodes of chronic pancreatitis in one year, and the patient was therefore diagnosed as having chronic pancreatitis with clinical signs of intermittent chronic diarrhoea, constant abdominal pain, poor food intake, and weight loss. As a result parenteral nutrition was administered. Chronic pancreatitis was also reported based on biochemical parameters, imaging studies from computed tomography of the pancreas and magnetic cholangioresonance. Ultrasound report was: presence of chronic inflammatory changes, pancreatic lobe-shaped borders, tortuous and dilated main duct, normal bile ducts, and the presence of echogenic tracts and points throughout the gland. The diagnosis of chronic pancreatitis was therefore confirmed by imaging studies.
The patient was admitted to hospital on a weekly basis due to intense pain, which reached 8–9/10 on the visual numerical scale, and with poor analgesic response from the administration of NSAIDS, adjuvant treatment and upper limit doses of oral or intravenous opiods. In order to ameliorate the symptoms of pain, the patient was treated with a retrograde endoscopic cholangiopancreatograph in order to perform a sphincterotomy of the pancreas. As symptoms did not improve, it was decided to refer the patient to the endoscopic department for unilateral celiac plexus block.
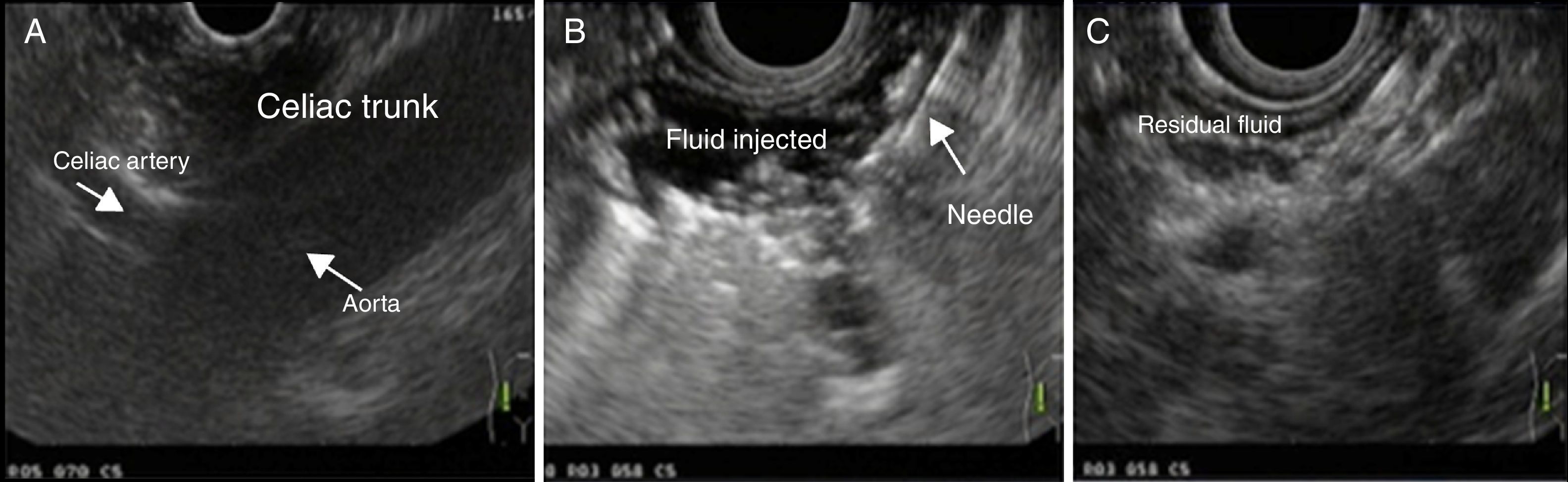
We will now describe the procedure of the unilateral celiac plexus block. Under general anaesthesia a lineal echoendoscopy was inserted, which crossed the diaphragmatic pillars and entered the gastric cavity for primary examination of the pancreas. The celiac trunk region was then located using anatomical references established by the colour Doppler. Once the site had been identified, a 19G calibre neurolysis needle was inserted in real time, through removal of the stylus and drawing of the syringe, with vascular puncture being ruled out. Following this, and with constant observation the content of the first syringes was injected. This consisted of 2ml of physiological saline solution to confirm puncture site. After this the content of the second syringe with 10ml of ropivacaine in 7.5mg/ml presentation was injected, and finally the third syringe with 500mg of methylprednisolone. The fourth syringe was again applied with 2ml of physiological saline solution to completely empty the pharmacological content applied.
The approximate duration of the procedure was 15 minutes, and the patient was then sent to the recovery room, where he was monitored for 8h to identify any complication or manifestation of pain.
During monthly follow-up which lasted for 3 months, clinical parameters were assessed, using the visual numerical scale. The score fell to 1–2/10 and there was an improvement in clinical symptomatology in general. Biochemical parameters were also assessed, with no abnormal data nor variation being observed. Finally, clinical assessment of pain was made which reported progressive reduction of NSAID and oral narcotics to a minimum dose. Analgesic response to the unilateral celiac plexus block was thereby confirmed and parenteral nutrition was removed. General symptoms improved and complete oral nutrition was achieved.
Case 2Female aged 12, who weighed 49kg. Since infancy she had suffered from symptoms of constipation, gastroesophageal reflux disease and urinary tract infections.
She had begun to have intense, extended abdominal pains 3 years previously, which were reported to be recurrent acute pancreatitis, since in 3 years she suffered from 8 episodes. The diagnosis of chronic pancreatitis was confirmed based on the clinical signs: increase of pancreatic enzymes and computed tomography of the pancreas which reported a tortuous pancreatic duct and small glandular calcium deposits.
The patient was treated with retrograde endoscopic cholangiopancreatograph with pancreatic and biliary sphincterotomy, with which partial improvement of symptoms was achieved. Due to the complexity of the abdominal pain treatment, the doctors in the pain clinic initiated analgesia with oral and parenteral opiods, in addition to a peridural block with which an improvement, but not full remission of pain was obtained. The attending physicians decided to treat the patient with a celiac plexus block guided by EUS with the standard unilateral technique used on adults.
Similarly to the first case, the operation was performed under general anaesthesia: the lineal echoendoscopy was inserted through the mouth, locating the celiac ganglion from the lower curvature of the stomach, following the aorta and using the colour Doppler. Through the 19G calibre neurolysis needle, in sequence, the contents of the first syringe were injected. This consisted of 2ml of physiological saline solution to confirm puncture site. After this the content of the second syringe with 10ml of ropivacaine in 7.5mg/ml presentation was injected, followed by the third syringe with 500mg of methylprednisolone. Finally, the fourth syringe was again applied with 2ml of physiological saline solution to completely empty the pharmacological content applied. The procedure concluded with no variations in vital parameters and no incidents, and the patient was therefore sent to the recovery area, where she remained pain free and under strict monitoring for 8h. She was then referred to her hospital with clinical indications.
Three month follow-up ensured and response to the block was satisfactory: the pain lessened considerably, with a drop in the numerical visual scale from 8/10 to 3/10. The procedure enabled the NSAIDS to be gradually reduced and the opioids were completely withdrawn. Food intake also improved, due to the non presentation of nausea and vomiting and weight gain was appreciated as a result Follow-up was therefore concluded.
DiscussionIn the paediatric population, inflammatory pancreatic diseases commonly lead to hospital admittance and pain clinic management in the Paediatric Hospital of the Centro Médico Nacional Siglo XXI. The use of EUS for the treatment of pain includes celiac block and neurolysis for chronic inflammatory diseases or in neoplasic-based diseases. In children, there is little experience in their use for the diagnosis of pancreatic illnesses and even less so as a method for alleviating pain with the use of celiac block.
It has been reported that chemical blocking of the celiac plexus guided by EUS offers several advantages,7,8 since topical anaesthetics may be used such as bupivacaine or can be combined with deposit steroids such as triamcinolone or methylprednisolone. A neurolytic block consists of the injection of agents such as 98% alcohol or 7.5% phenol solution which destroys the painful pathways from segmental demyelination or Wallerian degeneration. This technique is primarily indicated for the oncologic patient, although it has been recommended in cases of early recurrence in benign diseases and is based on neurolysis of the celiac trunk induced with ethanol for the remission of pain in pancreatic cancer.9
The agent of choice is injected using a needle for celiac neurolysis or a fine aspiration-injection 19G needle through ultrasound-guided endoscopy in real time, with a lineal variety echoendoscope, locating the region of the celiac ganglions in the lower curvature of the stomach after the appearance of the celiac trunk of the aorta.10 The anterior approach avoids the retrocrural space and reduces the risk of neurological complications such as paresthesia or paralysis to a minimum, which may occur during the posterior approach due to spasm or thrombosis of the anterior spinal artery. As a result, the ultrasound-guided celiac plexus block is considered a safe and effective technique to reduce the intensity of pain which involves low morbidity and on the whole surpasses other techniques.
Ultrasound-guided endoscopy of the celiac plexus block is performed with control Doppler, and is therefore a safer option than percutaneous celiac plexus block.11
This therapy has been used since the beginning of the year 2000 in patients with pain associated with pancreatic diseases. Traditionally, the EUS injection is based on neurolysis of the celiac trunk induced with ethanol for the remission of pain in cancer of the pancreas.12
The type of needle for neurolysis is variable and 19 and 22G calibre needles may be used, without any real variation in the technique (Fig. 3). Unilateral application is well accepted, although several authors recommend bilateral application. In both cases, unilateral block technique was used, because it is the one most commonly used in worldwide reports, and it has also been reported that no clinical differences exist regarding outcome with respect to the bilateral technique.13 In accordance with Membrillo,14 the Specialised Hospital offers support health care to the Paediatric Hospital in the aetiological search of patients with acute pancreatitis, recurrent idiopathic pancreatitis and chronic pancreatitis. The patients with these diagnoses are frequently admitted to the emergency department due to the pain syndrome they present.
Celiac plexus block guided by EUS should be considered as a treatment option once the frequency of hospital admittances has been analysed, together with the high doses of narcotics. An exhaustive study of the medical history, consultancy studies, laboratory findings which confirm the diagnosis of chronic pancreatitis and poor response to pain management should also be taken into consideration.
Both patients were presented in sessions with the attendant doctors and support services, among which were the Pain Clinic and the analysis, preparation and execution of procedures by the Gastropediatric and Gastroendoscopy Department, with prior authorisation from parents or tutors. Oral analgesics were significantly lower in dose after 4 weeks. Pain scores on the scale, together with symptoms generated by the pancreatitis, tended to improve with similar outcome to experience reported in scientific literature. Furthermore, the adverse effects produced by the use of opioids and consequent morbidity secondary to the procedures were non-existent in our cases.
ConclusionsThe technique in adults may be adapted to the paediatric patient, when pain caused by chronic pancreatitis is expected to be difficult to control. We propose that neurolysis or celiac block may be considered as an initial strategy for pain management, since it is possible to reduce morbidity and mortality with them in patients with recurrent pancreatitis. This would mean the reduction in under-nutrition and the other associated symptomatology which impact the development, functioning and quality of life for the paediatric patient. This technique may be used at intervals of 3–4 months until a final neurolysis is decided.
Publications concerning celiac block guided by EUS is limited to infants, and we therefore believe that further studies are needed with regard to the use of this technique. Experiences and outcome need to be shared in order to offer a more formal recommendation.
Ethical disclosuresProtection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of dataThe authors declare that they have followed the protocols of their work center on the publication of patient data.
Right to privacy and informed consentThe authors declare that no patient data appear in this article.
Conflict of interestsThe authors have no conflict of interests to declare.
Please cite this article as: Membrillo-Romero A, Rascón-Martínez DM. Bloqueo celiaco en Pediatría mediante ultrasonido endoscópico para el manejo de dolor por pancreatitis crónica. Revisión de la técnica en 2 casos. Cir Cir. 2017;85:264–268.