Central serous choroidopathy is a macular disease, usually with a self-limited and benign course, and predominantly affects male patients between 20 and 45 years old.
Clinical caseA 68 year-old female patient complained of decreased visual acuity of her right eye of approximately 3 weeks of onset. Best corrected visual acuity in her right eye was 20/100. Fundus examination revealed a macular serous detachment involving its centre, as well as the presence of multiple calcified drusen. Fluorescein angiography showed late parafoveal leakage in a “smokestack” pattern in the right macular area. Optical coherence tomography showed a dome-shape macular detachment, also in the right eye. The patient was observed every 2 weeks and spontaneous resolution of the macular detachment was seen a month later. Based on these clinical features, a diagnosis was made of central serous choroidopathy of atypical presentation.
ConclusionsAtypical presentation cases of serous central choroidopathy might be seen occasionally. Hence, it is an important differential diagnosis of age related macular degeneration in patients older than 60 years.
La coroidopatía serosa es una afección macular, de curso autolimitado y, por lo general, benigno, que afecta predominantemente a varones de entre 20 y 45 años de edad.
Caso clínicoMujer de 68 años de edad, con baja de agudeza visual de aproximadamente 3 semanas de evolución del ojo derecho. Su capacidad visual en el ojo derecho era de 20/100. En el segmento posterior se apreció una imagen de desprendimiento seroso circular en mácula del ojo derecho, abarcando su centro. Se encontró presencia de múltiples drusas de aspecto calcificado. En la angiografía fluoresceínica se encontró fuga parafoveal con patrón «en humo de chimenea» en fases tardías del estudio en área macular derecha, mientras que la imagen por tomografía de coherencia óptica mostró despegamiento en domo de retina neurosensorial del ojo derecho a nivel macular. Se optó por mantener a la paciente en vigilancia cada 2 semanas, observándose la remisión espontánea del desprendimiento de retina seroso un mes después. Con base en los datos anteriores se integró el diagnóstico de coroidopatía serosa central del ojo derecho de presentación atípica.
ConclusionesPuede haber casos atípicos en cuanto a la presentación de la coroidopatía serosa central, estando dentro de los diagnósticos diferenciales de la enfermedad macular, sobre todo en maculopatía relacionada con la edad en pacientes de ambos sexos, mayores de 60 años de edad.
Central serous choroidopathy is generally a unilateral condition, which predominantly affects males between the ages of thirty and fifty, and in the majority of cases has a self-limited and benign evolution with regards to visual function. It is characterised by the presence of an abrupt, moderate loss of vision, accompanied on occasions by a relative, central, metamophopsia, micropsia scotoma. The presence of a circular circumscriptive detachment of the neurosensorial retina may be observed at the posterior pole, with no signs of exudation.1
There are however isolated cases which stray away from this clinical behaviour pattern in both presentation and course, i.e. the condition may present in patients outside this age range, in females and may significantly compromise the visual acuity of the patient with a recurrent and chronic course.2–4 We report a case of atypical presentation.
Clinical caseA female patient aged 68 who presented with a decreased visual acuity of her right eye of approximately 3 weeks of onset. She became aware of this complaint by coincidence. The patient stated there was no history of any significance nor was she taking any drugs at that time. Physical examination revealed visual acuity in her right eye of 20/100, whilst in her left eye it was 20/20. The Amsler test, which consists in giving the patient a quadricular drawing to assess if the patient sees distortion in the lines, tested positive in the right eye.
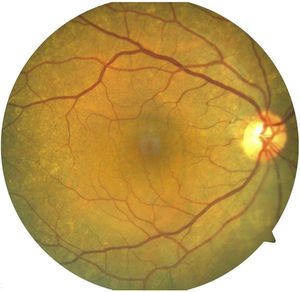
On examination of the anterior segment an incipient nuclear sclerosis was found in the lens of both eyes. In the posterior segment the image of a circular serous detachment was seen in the macular of the right eye, involving its centre. The presence of multiple calcified drusen was found, predominantly in the vascular arch pathways (Fig. 1).
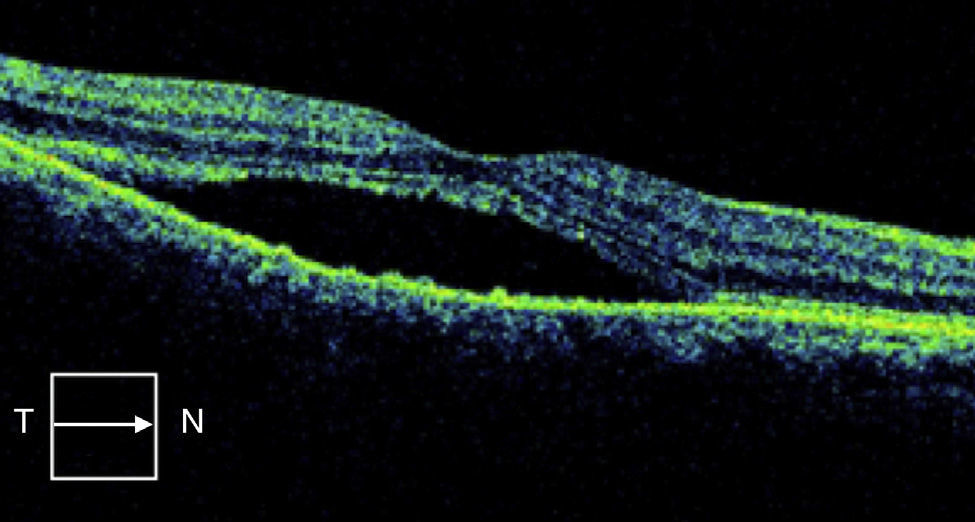
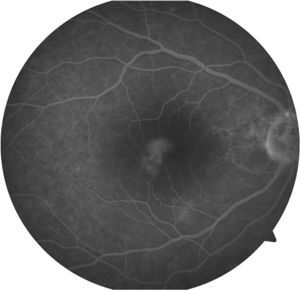
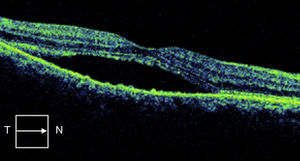
Fluorescein angiography showed late parafoveal leakage in a “smokestack” pattern in the right macular area (Fig. 2), whilst the optical coherence tomography showed a dome-shape macular detachment, in the right eye neurosensorial retina (Fig. 3) The patient was observed every two weeks, and spontaneous resolution of the macular detachment was seen a month later. Based on these clinical features, a diagnosis was made of central serous choroidopathy of the right eye. Based on the appearance of the leakage in a “smokestack” which showed up in the fluorescein angiography, the appearance of the optical coherence tomography and self-limitation of the condition, other much more widely prevalent conditions in the patient's age range, such as wet macular degeneration, were ruled out.
DiscussionCentral serous choroidopahy has certain demographic characteristics. The age range of presentation is between 20 and 45 years of age. However, more recent studies have reported an older average age range. In a 1996 study of 130 patients with central serous choroidopathy, the mean age was 51.2
Two recent major case studies and retrospective controls have been undertaken with this older age group. One study involving 230 patients found a mean age of 51,3 and the other study, with 312 patients, revealed a mean age of 45.4
Notwithstanding, a presentation age over 60 is much less frequent.3,4 As an example of an extreme of this assertion, Gobuty et al.5 reported a case similar to ours, of a female where the central serous choroidopathy presented at 91 years of age.
It is therefore important to underline the fact that when diagnosing a patient over 50, macular degeneration, choroidal neovasularision or polypoidal choroid vasculopathy6 should be ruled out, prior to making a diagnosis of central serous choroidopathy. It is also important to rule out concomitant drug regimes, since their ingestion has been associated with this condition, for example: corticosteroids, and the development of central serous choroidopathy in advanced ages.7,8
It affects mainly males, with a male:female ratio of approximately 6:1. This predilection was not present in our reported case history.
Furthermore, the disease is usually unilateral, although bilateral participation is common in chronic cases and in those cases related to the excess of endogenous or exogenous steroids.
In general the disease is self-limiting and in 90% of case there would be a spontaneous recovery in a few months, without any significant visual loss. Notwithstanding, several patients may develop chronic or recurrent processes causing areas of atrophy of the pigment epithelium of the retina or hypertrophy of the same, with visual loss. Up to 50% of patients may develop recurrence;9–12 this may present at any time, but in 50% of patients this occurs during the first year. A history of psychiatric disease is associated with a higher rate of recurrence, including anxiety or mood swing diseases such as bipolarity and major depression, among others.12
A minor proportion of patients develop an irreversible and serious visual loss from atrophy of the pigment epithelium of the retina and the development of choroid neovascularisation which is present in up to 6% of patients and its transformation into polypoidal choroid vasculopathy with exudation and haemorrhaging. Secondary choroid neovascularisation may develop in patients with chronic central serous choroidopathy or after treatment, such as photocoagulation with laser.
Polypoidal choroid vasculopathy, which is one of the major differential diagnoses is characterised by the development of abnormal polypoidal dilations from interior choroid circulation, which leads to recurrent episodes of exudative maculopathy with serous detachment or haemorrhaging of the pigment epithelium. When patients present with polypoidal choroid vasculopathy with just haemorrhagic detachment of the serous pigment macular epithelium, it may be confused with central serous choroidopathy. Diagnosis of polypoidal vasculopathy may be determined with angiography with indocyanine green angiography, where the ramification of choroid vascular pathways and polyps also appear at this level.13
Optical coherence tomography may help to differentiate between the 2 entities. It is capable of showing polyps in the polypoidal choroid vasculopathy, whilst in the central serous choroidopathy the subretinal space may be free from these lesions, as is the case of our patient.
The patient's age and the presence of degenerative changes in the posterior pole, such as the presence of drusen, may invite one initially to consider the presence of choroidal neovasularisation, a condition that must be taken considered as a primary diagnosis. A part of this diagnosis must always rule out the presence of detachment of the retina's pigment epithelium, which is an important component of choroidal neovasularisation. There are 4 main types with which a differential diagnosis must be made: haemorrhagic detachment, serous detachment, fibrovascular pigment epithelial detachment and drusenoid pigment epithelial detachment. In these cases the angiographic pattern is very different; for example, in fibrovascular pigment epithelial detachment of the retina, hyperflourescence presents up until the first or second minute of injected fluorescein with an irregular raising of the pigment epithelium and the presence of scattered stippling.2 Unlike the above-mentioned situation, the angiographic characteristics of the lesion, the presence of leakage in a “smokestack” pattern in the later phases of the study, the optical coherence tomography which showed a dome-shape macular detachment, the lack of hyperreflective images indicative of choroid neovascularisation or polyps in the subretinal space and the self-limitation of the process indicate the diagnosis of central serous choroidopathy.
ConclusionsSerous choroidopathy rarely presents in patients aged over 60, and also rarely in females, and it is established as one of the differential diagnoses of macular disease in this age group. However, for this same reason, it is important to sometimes carry out complementary studies to rule out or confirm diagnosis. These studies include fluorescein angiography, indocyanine green angiography and optical coherence tomography.
Conflict of interestsThe author has no conflict of interest to declare.
The author would like to thank the personnel of the David Clinic for their participation in the preparation of this case report.
Please cite this article as: Hernández-Da Mota SE. Presentación atípica de coroidopatía serosa central. Reporte de caso. Cir Cir. 2016;84:309–312.